Jan 31, 2026
You have tried everything. The benzoyl peroxide that dried your skin until it cracked. The antibiotics that worked for three months and then stopped. The retinoids that made you peel like a sunburn in July. And still, every morning, you look in the mirror and see new breakouts forming along your jawline, your cheeks, your forehead.
The frustration is real. It is exhausting. And it makes you wonder whether anything out there actually targets acne at its root rather than just masking symptoms while creating new problems. Here is the truth that most dermatology articles will not tell you: the conventional approach to acne treatment is fundamentally limited. Antibiotics breed resistance. Harsh topicals destroy the skin barrier.
Accutane works but carries serious risks. Meanwhile, an entirely different class of molecules has been quietly demonstrating remarkable potential in both laboratory and clinical settings.
These molecules are peptides. They are small chains of amino acids that your body already recognizes, already uses, and already trusts. Peptides for acne represent a genuine shift in how we think about skin health, moving away from scorched-earth tactics and toward intelligent, targeted interventions that work with your biology rather than against it. This guide covers everything. The science behind why peptides fight acne differently than conventional treatments. The specific peptides that target active breakouts, heal scars, and rebuild damaged skin. The practical routines, timelines, and combinations that actually deliver results. Whether you are dealing with stubborn hormonal acne, persistent post-inflammatory marks, or antibiotic-resistant breakouts that nothing seems to touch, the answers you need are here.
Why acne happens (and why most treatments fall short)
Acne is not a simple problem. It is the visible result of four interconnected processes happening beneath the surface of your skin, and understanding these processes is the first step toward understanding why peptides offer something genuinely different.
The four drivers of every breakout
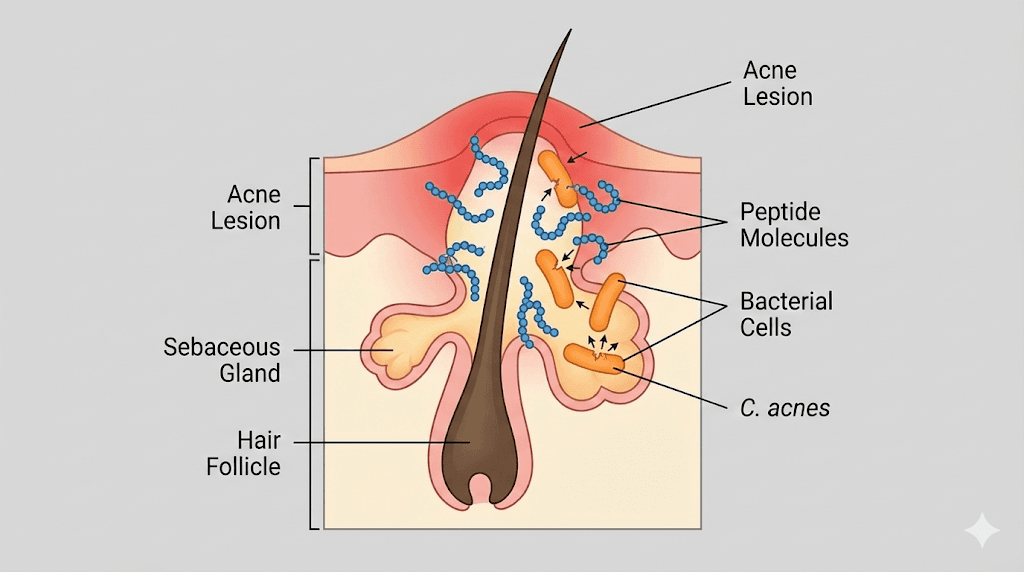
Every single acne lesion, from the smallest whitehead to the most painful cystic nodule, traces back to four key factors working together. First, the sebaceous glands produce too much sebum. This oily substance normally protects and moisturizes the skin, but when production goes into overdrive, it creates a greasy environment where problems begin. Second, the cells lining the hair follicle start multiplying too quickly and sticking together. This process, called follicular hyperkeratinization, plugs the pore with a mixture of dead skin cells and excess oil. A microcomedo forms. You cannot see it yet, but the stage is now set.
Third, a bacterium called Cutibacterium acnes (formerly Propionibacterium acnes) thrives in this oxygen-poor, oil-rich environment. It feeds on the trapped sebum and multiplies rapidly. Fourth, and this is where the real damage happens, your immune system responds to the bacterial overgrowth with inflammation. The C. acnes bacteria activate toll-like receptor 2 (TLR2) on surrounding cells, triggering a cascade of inflammatory signals. Interleukin-8 floods in, recruiting neutrophils to the site. TNF-alpha and IL-12 amplify the response. Th17 cells arrive and release IL-17, which further damages tissue and prolongs the inflammatory cycle.
The result? Redness. Swelling. Pain. Scarring.
Hormones and the sebum connection
Behind the scenes, hormones are pulling the strings. Androgens like testosterone and dihydrotestosterone (DHT) bind to receptors on the sebaceous glands and tell them to produce more sebum. This is why acne often flares during puberty, before menstruation, during periods of stress, and in conditions like polycystic ovary syndrome. The IGF-1/PI3K/Akt/mTOR signaling pathway also plays a critical role. When insulin-like growth factor 1 (IGF-1) levels rise, whether from hormonal changes, diet, or other factors, this pathway activates and drives both sebum production and keratinocyte proliferation. It is the same pathway that responds to high-glycemic diets and dairy consumption, which is why those dietary connections to acne are not just anecdotal. Women dealing with hormonal acne often find that conventional treatments fail to address this underlying driver, which is why breakouts keep returning the moment treatment stops.
The antibiotic resistance crisis in acne treatment
For decades, antibiotics have been a frontline acne treatment. Topical clindamycin. Oral doxycycline. Minocycline. Erythromycin. They worked, at first. But C. acnes adapted. Research shows that antibiotic resistance can develop after just eight weeks of topical antibiotic monotherapy. Eight weeks. That is barely two months of treatment before the bacteria learn to shrug off the medication. The numbers are staggering. In some regions, antibiotic-resistant C. acnes strains account for more than half of all clinical isolates. This means that for many patients, the most commonly prescribed acne treatments are becoming less effective with each passing year. And every course of antibiotics does not just affect acne bacteria. It disrupts the entire skin and gut microbiome, potentially creating cascading health effects that extend far beyond the face.
This is the fundamental problem. Conventional acne treatments are either too harsh, too temporary, or increasingly ineffective. They treat symptoms while ignoring the sophisticated biological processes that drive the condition. The need for a smarter approach has never been more urgent.
How peptides fight acne differently
Peptides do not work like antibiotics. They do not work like retinoids. They do not work like benzoyl peroxide. The way peptides work is fundamentally different from every conventional acne treatment, and this difference is exactly why they deserve serious attention.
Your skin already uses peptides to fight infection
Here is something remarkable. Your skin produces over 100 different antimicrobial peptides (AMPs) as part of its natural defense system. These are not foreign chemicals. They are molecules that your body manufactures every single day to protect against infection, regulate inflammation, and maintain the integrity of the skin barrier. Keratinocytes produce them. Sebocytes produce them. Sweat glands, mast cells, and neutrophils all contribute to this peptide defense network. The most well-studied skin AMPs include cathelicidin LL-37, human beta-defensins (hBD-2 and hBD-3), dermcidin, and RNase-7. Each plays a distinct role. Some puncture bacterial membranes directly. Others recruit immune cells to sites of infection. Some do both.
When acne develops, it often signals that this natural peptide defense system is either overwhelmed or imbalanced. The therapeutic use of peptides for acne essentially reinforces and restores what your skin is already trying to do on its own.
Membrane disruption: why bacteria cannot easily resist peptides
Antibiotics typically target a single specific mechanism in bacterial cells, such as protein synthesis or cell wall construction. This specificity makes it relatively easy for bacteria to develop resistance through a single genetic mutation. Peptides take a different approach entirely. Most antimicrobial peptides kill bacteria by physically disrupting their cell membranes. They interact with the lipid bilayer of the bacterial membrane, inserting themselves into it and creating pores or destabilizing the entire structure. The bacterium essentially falls apart.
This mechanism is extraordinarily difficult for bacteria to resist. To develop resistance to membrane-disrupting peptides, a bacterium would need to fundamentally alter the composition of its cell membrane, a change so dramatic that it would likely compromise the bacterium ability to survive. This is why antimicrobial peptides have remained effective for millions of years of evolution while antibiotics can lose their power in weeks. For anyone dealing with antibiotic-resistant acne, this distinction matters enormously.
Multi-target action: beyond just killing bacteria
What makes peptides particularly promising for acne is that many of them do not just kill bacteria. They simultaneously address multiple aspects of the acne cascade. A single peptide can reduce sebum production, calm inflammation, kill C. acnes, promote healing of existing lesions, and stimulate collagen production to minimize scarring. No antibiotic does all of that. No retinoid does all of that. No single conventional treatment addresses the full spectrum of acne pathology the way certain peptides can. This multi-target approach means fewer products, fewer side effects, and more comprehensive results. Understanding peptide formulations is essential for anyone looking to leverage these benefits effectively.
The dual role of LL-37: a cautionary note about complexity
Peptide biology is not without its nuances. Cathelicidin LL-37, one of the most potent antimicrobial peptides in human skin, illustrates an important point. While LL-37 is highly effective at killing C. acnes and other pathogens, it also functions as an alarmin, a molecule that can amplify inflammation under certain conditions. In acne lesions, elevated LL-37 levels have been associated with increased inflammatory signaling. This dual role demonstrates that peptide-based acne treatment requires specificity. It is not enough to simply boost all peptide activity in the skin. The right peptides must be chosen for the right purposes, in the right concentrations, applied through the right delivery methods. The following sections identify exactly which peptides meet these criteria for active acne, scarring, and overall skin health.
The best peptides for active acne
Not all peptides target acne equally. Some excel at killing bacteria. Others calm inflammation. A select few do both while simultaneously regulating the excess sebum that starts the entire acne cascade. Here are the peptides with the strongest evidence for treating active breakouts.
GHK-Cu (copper peptide): the multi-purpose powerhouse
GHK-Cu is a naturally occurring tripeptide, just three amino acids (glycyl-L-histidyl-L-lysine) bound to a copper ion. It was discovered in human blood plasma by Dr. Loren Pickart in 1973, and decades of research have revealed it to be one of the most versatile healing molecules in the human body. For acne specifically, GHK-Cu offers a remarkable combination of benefits.
Its anti-inflammatory properties reduce the redness and swelling of active acne lesions by modulating inflammatory cytokine production. Its wound-healing capabilities accelerate the closure and repair of damaged skin, meaning breakouts heal faster and with less risk of permanent scarring. And its ability to stimulate fibroblast activity and boost collagen and elastin production means that the skin rebuilds stronger and smoother after each lesion resolves. A twelve-week study demonstrated that GHK-Cu improved collagen production in 70% of women tested, compared to 50% for vitamin C and 40% for retinoic acid. Those numbers are significant.
Perhaps most importantly for acne sufferers, GHK-Cu is well-tolerated by all skin types, including sensitive and oily skin. Unlike retinoids, which often cause dryness, peeling, and irritation that can actually worsen breakouts in the short term, copper peptides work gently. They do not strip the skin barrier. They do not cause purging in the way that many conventional acne treatments do. They support the skin rather than attacking it.
For those concerned about potential adverse reactions, understanding the evidence around copper peptide side effects is important. The safety profile is generally excellent. Some users report temporary warmth or mild tingling at the application site, but serious adverse reactions are rare. The question of copper peptide purging also comes up frequently. True purging is uncommon with GHK-Cu because it does not work through the same mechanisms as retinoids or acids. If you experience worsening breakouts, it is more likely a sensitivity reaction than a purging phase, and the guide on whether GHK-Cu is making skin worse covers how to differentiate and respond.
Dosing matters. For topical application, serums containing GHK-Cu at concentrations discussed in the copper peptide concentration guide are appropriate for acne-prone skin. The best copper peptide serums deliver the peptide in stable, bioavailable formulations that penetrate effectively without clogging pores.
KPV peptide: the inflammation killer
If GHK-Cu is the versatile multi-tool, KPV is the precision instrument for one specific and critical target: inflammation. KPV is a tripeptide derived from alpha-melanocyte stimulating hormone (alpha-MSH), consisting of just three amino acids: lysine, proline, and valine. Small molecule. Massive impact.
KPV works by blocking the NF-kB signaling pathway, which is the master switch for inflammatory gene expression in the body. When NF-kB is activated in acne, it drives the production of TNF-alpha, IL-6, IL-8, and other inflammatory mediators that cause the redness, swelling, and pain of breakouts. KPV turns that switch off. It inhibits the ERK/p38 MAPK/NF-kB axis in keratinocytes, which means it does not just reduce one inflammatory signal. It suppresses the entire inflammatory cascade at its source.
Research shows that KPV also possesses direct antimicrobial activity against Staphylococcus aureus and Candida albicans. While these are not the primary bacteria involved in acne vulgaris, this antimicrobial spectrum suggests broader protective effects for the skin microbiome. KPV accelerates wound closure and reduces visible redness, both of which directly benefit active acne lesions. For severe inflammatory acne, the kind that creates deep, painful nodules and cysts, KPV anti-inflammatory properties offer a targeted approach that conventional treatments often struggle to match.
The KPV dosage protocols vary depending on the route of administration. KPV can be administered orally, intravenously, subcutaneously, or transdermally. For acne, topical and subcutaneous routes are most commonly discussed in research contexts. Timing also matters, and whether to take KPV in the morning or at night may influence effectiveness based on the circadian rhythm of inflammatory processes in the skin.
Antimicrobial peptides from the research frontier
Beyond the established peptides, researchers are developing entirely new antimicrobial peptides designed specifically to target C. acnes. These next-generation molecules represent some of the most exciting developments in acne science.
LZ1 peptide is a fifteen-amino-acid designed peptide that has shown extraordinary potency against C. acnes in laboratory studies. Its minimum inhibitory concentration (MIC) against the acne bacterium is 0.6 micrograms per milliliter, which is four times lower than clindamycin, one of the most commonly prescribed topical antibiotics for acne. In a mouse model, LZ1 significantly reduced C. acnes colonization in treated skin. It also inhibited the secretion of TNF-alpha and IL-1beta, demonstrating both antimicrobial and anti-inflammatory activity. Critically, LZ1 showed low cytotoxicity on keratinocytes, meaning it targets the bacteria without damaging the surrounding skin cells.
DAP-7 and DAP-10 are novel designed antimicrobial peptides that address what may be the most urgent problem in acne treatment: antibiotic resistance. These peptides are active against both antibiotic-susceptible and antibiotic-resistant C. acnes strains. They maintain stability for twelve or more hours after protease exposure, meaning they remain active long enough to be therapeutically useful on the skin surface. In mouse models, DAP-7 reduced C. acnes colonies and decreased ear swelling, a proxy for inflammation, demonstrating dual antimicrobial and anti-inflammatory effects.
These research peptides are not yet available commercially, but they illustrate the trajectory of peptide-based acne treatment. The field is moving rapidly from laboratory discoveries toward practical applications. Understanding the full landscape of available peptides helps contextualize where these emerging molecules fit within the broader peptide ecosystem.
Oligo Peptide-10 and sebum regulation
One of the most overlooked aspects of acne treatment is sebum regulation. Most treatments focus on killing bacteria or reducing inflammation after the breakout has already formed. Oligo Peptide-10 takes a different approach by targeting the process upstream. This signaling peptide interacts with cellular pathways that control sebum production in the sebaceous glands. By reducing the amount of excess oil that clogs pores in the first place, it addresses acne at one of its earliest stages. It also reduces comedone formation, which means fewer of those initial plugged pores that eventually develop into full-blown breakouts.
For people with persistently oily skin who find that even after treating active lesions, new breakouts keep forming, a sebum-regulating peptide like Oligo Peptide-10 can fill a critical gap in their routine.
Palmitoyl Tetrapeptide-7: anti-inflammatory and antibacterial
Palmitoyl Tetrapeptide-7 brings a dual mechanism to acne management. It reduces inflammatory signaling in the skin while also demonstrating direct activity against acne-causing bacteria. This combination makes it particularly useful for the type of inflammatory acne where bacterial proliferation and immune overreaction work together to create persistent, angry lesions. Its skin regeneration properties further accelerate the healing of active breakouts, reducing the window during which a lesion can cause permanent damage to the surrounding tissue. The peptide is commonly found in advanced skincare formulations and pairs well with other anti-inflammatory peptides for comprehensive acne management.
Peptides for acne scars and skin repair
Clearing active breakouts is only half the battle. For millions of people, the real source of frustration is not the acne itself but the marks it leaves behind. Post-inflammatory hyperpigmentation. Pitted atrophic scars. Raised hypertrophic scars. Ice pick marks. Rolling scars. Boxcar scars. Each type tells a story of tissue damage and imperfect healing, and each type responds to the right peptide intervention.
BPC-157: the tissue repair specialist
BPC-157 is a fifteen-amino-acid peptide originally isolated from human gastric juice. Its full name, Body Protection Compound-157, hints at its remarkable range of protective and healing effects. For acne scarring, BPC-157 offers several mechanisms that directly promote skin repair and regeneration.
It promotes angiogenesis, the formation of new blood vessels, which is essential for delivering oxygen and nutrients to healing tissue. It exhibits potent anti-inflammatory activity, reducing the prolonged inflammation that contributes to scar formation. It supports skin hydration and helps repair the skin barrier, which is often compromised in acne-affected areas. Understanding what BPC-157 is at a molecular level helps explain why it has become one of the most discussed peptides in the recovery and healing community.
The BPC-157 dosing protocols depend on the delivery method. For skin-related applications, subcutaneous injection near the affected area is one approach discussed in research literature. The BPC-157 dosage calculator can help determine appropriate amounts based on individual parameters. Some researchers have explored BPC-157 alternatives that may offer similar tissue repair benefits through different mechanisms. What sets BPC-157 apart is the breadth of its healing action, it does not just address one aspect of scar remodeling but supports the entire repair process from initial inflammation through collagen deposition and tissue restructuring.
TB-500 (Thymosin Beta-4): accelerated healing and reduced scarring
TB-500, also known as Thymosin Beta-4, is a naturally occurring peptide found in virtually all mammalian cells. Its role in the body centers on cell migration, tissue repair, and the regulation of actin, a protein crucial for cellular movement and structural integrity. For acne scars, the research on TB-500 is compelling.
Studies have demonstrated that TB-500 increases re-epithelialization, the process by which new skin cells cover a wound, by 42% at four days and 61% at seven days compared to untreated controls. That is not a marginal improvement. That is a dramatic acceleration of healing that directly translates to less time for scar-forming processes to take hold. TB-500 promotes the migration of cells to wound sites, mobilizes stem cells that contribute to tissue regeneration, and critically, decreases scar formation and fibrosis. The full range of TB-500 benefits extends beyond skin healing to include anti-inflammatory effects and support for various tissue types.
The combination of BPC-157 and TB-500 has generated particular interest. The BPC-157 and TB-500 stacking guide covers how these two peptides complement each other, with BPC-157 primarily promoting angiogenesis and tissue protection while TB-500 drives cell migration and re-epithelialization. Together, they address the full spectrum of healing mechanisms needed for scar remodeling. Understanding how to approach peptide stacking in general is valuable for anyone considering combination protocols. The peptide stack calculator provides additional guidance on timing and dosing combinations.
Matrixyl (Palmitoyl Pentapeptide-4): the collagen builder
Acne scars, particularly atrophic (pitted) scars, represent a deficit of collagen in the affected tissue. The skin was damaged during the inflammatory phase of a breakout, collagen was destroyed, and the body did not produce enough new collagen to fully rebuild the area. Matrixyl addresses this directly.
Palmitoyl Pentapeptide-4, the active compound in Matrixyl, signals fibroblasts to increase production of collagen types I and III, the primary structural proteins in skin. Clinical studies have shown that Matrixyl reduces deep wrinkle surface area by 68% over six months of consistent use. While wrinkle reduction and scar filling are not identical processes, the underlying mechanism, increased collagen deposition in targeted areas, is relevant to both.
For acne-prone skin specifically, safety is paramount. Many collagen-boosting ingredients can clog pores or irritate sensitive skin. Matrixyl at 3% concentration has been shown to be safe for all skin types, including oily and acne-prone skin. Matrixyl 3000, an advanced formulation, matched retinol in anti-aging effectiveness without the irritation, dryness, and initial breakout period that retinol commonly causes. This makes it an excellent choice for people who need collagen support for scarring but cannot tolerate the aggressive ingredients typically recommended for that purpose. Those interested in how peptides compare to retinol should explore the detailed peptides versus retinol comparison.
GHK-Cu for scar remodeling
GHK-Cu appears again here because its role in scar management is distinct from its role in treating active acne. While treating breakouts focuses on its anti-inflammatory and healing-acceleration properties, scar treatment leverages its ability to remodel existing tissue. GHK-Cu has been shown to attract immune cells and promote both the breakdown of damaged collagen and the synthesis of new, properly organized collagen. This remodeling process is essential for improving the appearance of atrophic scars, where the goal is not just to fill the deficit but to restructure the tissue architecture.
The evidence for copper peptides for acne scars specifically is encouraging. Users report visible improvement in scar depth and skin texture over consistent use, and before-and-after documentation supports these anecdotal reports. For post-inflammatory hyperpigmentation, the dark marks that persist after a breakout heals, combining copper peptides with niacinamide and hyaluronic acid has shown promise. The broader topic of peptides for scars covers additional options beyond copper peptides alone.
The glow peptide approach to comprehensive skin repair
An emerging approach combines multiple healing and repair peptides into what is sometimes called glow peptide therapy. This typically involves GHK-Cu for collagen remodeling, BPC-157 for tissue repair and angiogenesis, and TB-500 for accelerated re-epithelialization and reduced fibrosis. The glow stack concept recognizes that scar healing is not a single-mechanism process but rather a complex interplay of repair pathways that benefit from multi-peptide support.
The glow peptide dosage guide covers specific protocols, while the general category of glow peptides continues to expand as more research identifies complementary combinations. For anyone dealing with significant acne scarring who has been disappointed by single-ingredient approaches, the multi-peptide strategy represents a more sophisticated and often more effective path forward.

Topical peptides versus injectable peptides for acne
One question comes up constantly in peptide discussions. Should I use topical products or injectable peptides for my acne? The answer depends on what you are trying to achieve, the severity of your condition, and your comfort level with different delivery methods.
When topical peptides make sense
Topical peptide formulations are the starting point for most people. They are accessible, non-invasive, and effective for mild to moderate acne and surface-level scarring. A well-formulated peptide serum delivers active molecules directly to the epidermis and upper dermis, where they can interact with keratinocytes, sebocytes, and the superficial immune cells that drive the inflammatory component of acne.
Topical GHK-Cu serums, for example, have demonstrated meaningful improvements in skin texture, inflammation, and collagen production when used consistently. Matrixyl and Palmitoyl Tetrapeptide-7 are exclusively topical applications that perform well in their intended roles. For daily maintenance, prevention of new breakouts, and gradual improvement of mild scarring and skin tone, topical peptides are effective and practical. Building a proper copper peptide skincare routine is a good foundation for topical peptide use. Formulations like creams with copper peptides and collagen peptide serums provide established options for topical delivery.
The limitation of topical peptides is penetration depth. The stratum corneum, the outermost layer of skin, acts as a barrier that limits how much of a topical peptide actually reaches its target cells in the deeper dermis. Smaller peptides penetrate better than larger ones, and formulation technology (liposomal delivery, microneedling-assisted delivery, carrier peptides) can improve absorption. But for deep scarring or severe systemic inflammation, topical delivery may not be sufficient on its own.
When injectable peptides offer more
Injectable peptides bypass the skin barrier entirely. Subcutaneous injection delivers the peptide directly into the tissue, where it can reach deeper structures, enter systemic circulation, and achieve concentrations that topical application simply cannot match. For severe acne scarring, particularly deep ice pick and boxcar scars, injectable peptides like BPC-157 and TB-500 can stimulate repair processes at a level that topical products cannot reach.
The full list of injectable peptides extends well beyond those used for acne, but BPC-157 and TB-500 are the most relevant for skin repair applications. Injectable versus oral peptide delivery is another comparison worth understanding, as some peptides like KPV can be administered through multiple routes.
The trade-offs are real, though. Injectable peptides require proper reconstitution, sterile technique, and careful storage. The peptide reconstitution calculator helps ensure accurate preparation, and understanding bacteriostatic water for peptides is essential for safe reconstitution. Proper storage conditions, including whether peptides require refrigeration and how long they last in the fridge, directly impact both safety and effectiveness.
A practical comparison
For mild to moderate active acne, topical peptide serums containing GHK-Cu, Matrixyl, Oligo Peptide-10, and Palmitoyl Tetrapeptide-7 provide meaningful benefits with minimal complexity. For moderate to severe acne with significant scarring, a combined approach using daily topical peptides plus periodic injectable peptides (BPC-157, TB-500) addresses both surface and deep-tissue healing. For antibiotic-resistant acne, emerging antimicrobial peptides and KPV offer alternatives that work through mechanisms resistant to bacterial adaptation. The choice is not either/or. Many people start with topical formulations, see partial improvement, and add targeted injectable peptides to address what topical delivery alone cannot resolve. Getting started with peptides provides a comprehensive overview for anyone new to peptide use, regardless of the delivery method chosen.
Building a peptide skincare routine for acne-prone skin
Theory is valuable. Practice is what clears skin. This section translates the science into a concrete, daily skincare routine that incorporates peptides strategically for maximum acne-fighting benefit.
Morning routine
Step 1: Gentle cleanser. Start with a non-stripping, pH-balanced cleanser. Avoid anything that leaves your skin feeling tight or squeaky clean, as this strips the skin barrier and triggers compensatory oil production that makes acne worse. A micellar water or gentle foaming cleanser with a pH between 4.5 and 5.5 is ideal.
Step 2: Peptide serum. Apply your primary peptide serum to clean, slightly damp skin. For acne-prone skin, a GHK-Cu serum is an excellent morning choice because of its anti-inflammatory and protective properties. Apply a thin, even layer across the entire face, not just on active breakouts. Peptides work best as a preventive measure across all acne-prone areas. The GHK-Cu dosage guidelines cover appropriate concentrations for topical use.
Step 3: Niacinamide. Follow with a niacinamide serum at 5-10% concentration. Niacinamide reduces sebum production, strengthens the skin barrier, fades post-inflammatory hyperpigmentation, and has mild anti-inflammatory effects. It pairs beautifully with peptides. The combination of copper peptides and niacinamide is one of the most synergistic pairings in acne skincare.
Step 4: Non-comedogenic moisturizer. Even oily, acne-prone skin needs moisture. Choose a lightweight, oil-free, non-comedogenic moisturizer. Look for formulations containing hyaluronic acid for hydration without heaviness.
Step 5: Sunscreen. Non-negotiable. UV exposure worsens post-inflammatory hyperpigmentation, degrades peptides on the skin surface, and increases inflammation. Use a broad-spectrum SPF 30 or higher. Mineral sunscreens (zinc oxide, titanium dioxide) are less likely to trigger breakouts than chemical sunscreens.
Evening routine
Step 1: Double cleanse. If you wear sunscreen or makeup, start with an oil-based cleanser or micellar water to dissolve surface products, followed by your gentle water-based cleanser. This ensures a truly clean canvas for your evening peptides without over-stripping the skin.
Step 2: Active treatment. This is where you apply your strongest actives. If using benzoyl peroxide or salicylic acid, apply it now. Wait five to ten minutes for it to absorb and do its work before moving to peptides. This separation prevents the acid pH from degrading your peptide molecules.
Step 3: Peptide serum. In the evening, you can use either the same GHK-Cu serum from your morning routine or rotate to a different peptide. A Matrixyl-based serum is excellent for evenings because collagen synthesis is more active during sleep. Those looking to understand peptides for skin tightening and peptides for wrinkles will find that evening application maximizes the collagen-building benefits.
Step 4: Targeted scar treatment. If you have specific areas of scarring, apply a concentrated copper peptide treatment directly to those spots. The detailed guide on GHK-Cu injection dosage is relevant for those exploring more intensive scar treatment options beyond topical application.
Step 5: Night moisturizer. Use a slightly richer moisturizer than your morning product, but still non-comedogenic. Nighttime moisturizers that include ceramides help restore the skin barrier while you sleep.
Weekly additions
Once or twice per week, consider adding a gentle chemical exfoliant (a low-concentration AHA or BHA) to your evening routine. Apply it before your peptide serum, with at least a thirty-minute gap between the exfoliant and the peptide. Exfoliation removes dead skin cells that can trap sebum and contribute to comedone formation, and it also improves the penetration of subsequently applied peptides. Do not overdo it. Excessive exfoliation damages the skin barrier and creates more problems than it solves.
Combining peptides with other acne ingredients
Peptides do not exist in a vacuum. Most people with acne are already using other active ingredients, and knowing which combinations enhance your results and which combinations waste your money (or worse, damage your skin) is essential knowledge.
Peptides and niacinamide: the dream team
If there is a single combination that every acne sufferer should know about, it is peptides plus niacinamide. Niacinamide (vitamin B3) reduces sebum production by up to 23% in clinical studies. It strengthens the skin barrier by increasing ceramide production. It fades post-inflammatory hyperpigmentation by inhibiting melanosome transfer. And it has its own anti-inflammatory properties that complement the anti-inflammatory action of peptides like GHK-Cu and KPV.
The practical beauty of this combination is that niacinamide is stable across a wide pH range and plays well with virtually every other skincare ingredient. You can layer a niacinamide serum directly over a peptide serum without any waiting time or concern about degradation. This is the combination to build your routine around.
Peptides and retinol: proceed with caution
Retinol and its derivatives (tretinoin, adapalene, retinaldehyde) are among the most well-studied acne treatments. They work by increasing cell turnover, preventing follicular plugging, and reducing inflammatory signaling. The question of whether you can use peptides and retinol together is one of the most common in skincare forums.
The short answer: yes, but with caveats. Retinol is acidic and can denature some peptides if applied simultaneously. The solution is simple separation. Apply retinol as your first active step in the evening. Wait twenty to thirty minutes. Then apply your peptide serum. This allows the retinol to absorb and the skin pH to normalize before the peptides go on. The detailed guide on peptides and retinol covers specific protocols for this combination. For acne-prone skin specifically, starting with a low retinol concentration (0.25-0.5%) and gradually increasing helps avoid the irritation flare that drives many people to abandon retinol before it starts working.
Another approach is to alternate nights: retinol on Monday, Wednesday, and Friday. Peptide focus on Tuesday, Thursday, and Saturday. Sunday as a rest night with just moisturizer. This gives your skin the benefits of both without the risk of overwhelming a compromised barrier.
Peptides and salicylic acid
Salicylic acid (BHA) is oil-soluble, which means it can penetrate into pores and dissolve the mixture of sebum and dead cells that forms comedones. It is one of the most effective ingredients for preventing the clogged pores that initiate the acne process. Peptides and salicylic acid work on different aspects of acne and complement each other well. Apply your salicylic acid treatment first, wait ten to fifteen minutes for it to work, and then layer your peptide serum on top. The acid does the pore-clearing work. The peptide handles inflammation, healing, and long-term tissue repair.
Peptides and benzoyl peroxide
Benzoyl peroxide is a powerful antibacterial agent that kills C. acnes through oxidation. It is one of the few acne treatments to which bacteria have not developed significant resistance. However, benzoyl peroxide is also one of the most irritating and drying common acne treatments. It can bleach fabrics, degrade other ingredients, and compromise the skin barrier with overuse.
Use benzoyl peroxide as a short-contact treatment. Apply a thin layer to acne-prone areas, leave it on for five to ten minutes, then wash it off. Follow with your peptide serum. This approach gets the antibacterial benefits of benzoyl peroxide while minimizing irritation and avoiding direct contact between the oxidizing agent and your peptide molecules. Peptides applied after the benzoyl peroxide wash-off can help soothe and repair any irritation the treatment caused.
Peptides and vitamin C
Vitamin C (L-ascorbic acid) is an antioxidant that brightens skin, fades hyperpigmentation, and supports collagen production. For acne, its main benefit is addressing post-inflammatory marks. The combination with peptides requires attention to pH. Vitamin C serums are typically formulated at low pH (around 3.5), while most peptides perform best at a more neutral pH. The interaction between copper peptides and vitamin C deserves special attention. L-ascorbic acid can reduce the copper ion in GHK-Cu, potentially deactivating the peptide. The solution is simple: use vitamin C in the morning and copper peptides in the evening, or apply them at least thirty minutes apart. The broader discussion of vitamin C and peptides covers all the compatibility details.
Peptides and copper peptides and retinol together
The question of copper peptides and retinol compatibility specifically comes up often. Both are potent actives. Both are pH-sensitive. And both have strong evidence for acne and scar treatment. The safest approach is alternating nights rather than layering, especially when starting out. Once your skin tolerates both ingredients individually, you can experiment with same-evening use with a time gap between applications.
How long peptides take to work for acne
Patience is not a popular word when your face is breaking out. But understanding realistic timelines prevents the frustration that leads people to abandon effective treatments too early and jump to the next miracle ingredient, never giving anything enough time to work.
The first two weeks
During the first two weeks of consistent peptide use, visible changes are minimal. This does not mean nothing is happening. Beneath the surface, peptides are beginning to modulate inflammatory pathways, influence sebocyte behavior, and support the skin barrier. Some people notice a slight reduction in redness and irritation during this period. Active breakouts may begin to heal slightly faster. But this is not a dramatic transformation phase.
Weeks two through four
This is where peptide mechanisms start producing visible results. Inflammatory acne lesions begin to heal more quickly. New breakouts may be slightly less severe. Post-inflammatory redness begins to fade as the anti-inflammatory effects accumulate. If you are using peptides alongside other actives like salicylic acid or niacinamide, you may notice that these other ingredients seem to work better than before. This is not your imagination. Peptides support the skin barrier, which improves the penetration and effectiveness of other products in your routine.
A general reference for how long peptides take to work across various applications provides broader context, but for acne specifically, the four-week mark is when most users report their first clear improvement.
Weeks four through eight
The four-to-eight-week window is when peptides for acne truly hit their stride. The frequency of new breakouts typically decreases noticeably. Existing scars begin to soften and blend. Skin texture improves as collagen-stimulating peptides like Matrixyl and GHK-Cu accumulate their structural benefits over multiple skin cell turnover cycles. The skin overall looks healthier, more even-toned, and more resilient.
This is also the critical window where many people make the mistake of reducing or stopping their peptide routine because they feel like the job is done. It is not. The improvements at eight weeks represent the beginning of long-term cumulative benefits, not the end point.
Three months and beyond
At the three-month mark, the full scope of peptide benefits becomes apparent. Collagen remodeling is well underway, which is particularly relevant for scar improvement. The skin barrier is significantly strengthened. Sebum production may have normalized. The inflammatory threshold of the skin is higher, meaning it takes more to trigger a breakout. Understanding peptide cycle planning can help you structure long-term use, including whether to cycle peptides or use them continuously.
For deep acne scars, realistic improvement timelines extend to six months or longer. Collagen remodeling is a slow process. The body does not rebuild tissue architecture overnight. Consistent peptide use over six to twelve months can produce meaningful scar improvement that compounds over time. Before-and-after results from peptide users show the gradual but significant changes that occur with committed, consistent application.
When to adjust your approach
If you have been using peptides consistently for eight weeks and see zero improvement, it is time to evaluate. Are you using the right peptides for your specific type of acne? Is the formulation delivering adequate concentrations? Are other products in your routine degrading or counteracting your peptides? Is the delivery method appropriate for the severity of your condition? A topical serum may be insufficient for someone with deep cystic acne, while injectable peptides may be unnecessary for someone with mild comedonal acne. The peptide dosing guide and peptide dosage chart provide reference points for ensuring you are in the right therapeutic range.
Common mistakes when using peptides for acne
Even the best peptides fail when used incorrectly. These are the mistakes that undermine results most frequently, and every one of them is avoidable.
Mistake 1: using too many actives at once
Enthusiasm kills skin routines. Someone reads about peptides, niacinamide, retinol, vitamin C, AHAs, BHAs, and benzoyl peroxide, and decides to use all of them simultaneously. The result is a destroyed skin barrier, increased sensitivity, more inflammation, and paradoxically, more breakouts. Start with one or two actives plus your peptide serum. Add additional products one at a time, with at least two weeks between each new introduction. Understanding how many peptides you can use simultaneously is equally important. More is not always more.
Mistake 2: applying peptides to dirty skin
Peptides need to reach living skin cells to work. If you apply a peptide serum over a layer of sunscreen, makeup, sebum, and dead cells, most of the active molecules will never penetrate to their targets. Always apply peptides to freshly cleansed skin. Double cleansing in the evening is not optional for people using peptides for acne.
Mistake 3: using occlusive formulas over peptide serums
Some people follow their peptide serum with a heavy, occlusive moisturizer or sleeping mask. For acne-prone skin, this can trap sebum, bacteria, and dead cells against the skin surface, creating exactly the conditions that cause breakouts. Use lightweight, non-comedogenic moisturizers that allow the skin to breathe while sealing in hydration.
Mistake 4: expecting overnight results
Peptides are not pimple patches. They do not eliminate a breakout overnight. They work by modulating biological processes that take weeks to produce visible results. If you abandon peptides after five days because you still have acne, you never gave them a chance to work. Set your expectations appropriately. Commit to eight weeks minimum before evaluating effectiveness.
Mistake 5: storing peptides improperly
Peptides are biological molecules that degrade under heat, light, and oxidation. Leaving a peptide serum on your bathroom counter where it is exposed to steam, heat, and light from the shower degrades the active ingredients over time. Store peptide products in a cool, dark place. For reconstituted injectable peptides, refrigerated storage and shelf life must be taken seriously. Even for topical serums, understanding whether and when peptides expire ensures you are using effective products rather than degraded ones. The guide on peptide stability in powder form and at room temperature provides practical storage guidance.
Mistake 6: ignoring the rest of your routine
A peptide serum is not magic. It works within the context of a complete skincare routine. If you apply GHK-Cu in the morning but then use a pore-clogging foundation, skip sunscreen, and sleep in your makeup, the peptide cannot overcome those constant insults to your skin. Peptides amplify the effectiveness of a good routine. They cannot rescue a bad one.
Mistake 7: choosing the wrong delivery method
Someone with mild comedonal acne does not need injectable BPC-157. Someone with deep, widespread scarring may not get sufficient results from a topical serum alone. Match the delivery method to the severity of your condition. Peptide capsules, nasal spray peptides, and topical formulations each have their appropriate use cases. Understanding the differences between lyophilized versus liquid peptides and research versus pharmaceutical grade also impacts the quality and effectiveness of what you are using.
Special considerations: peptides for different acne types
Acne is not one disease. It is a spectrum of related conditions, and the peptide approach that works best depends on where you fall on that spectrum.
Hormonal acne
Hormonal acne, characterized by deep cysts along the jawline, chin, and lower cheeks, is driven by androgen fluctuations that increase sebum production. For this type, peptides that regulate sebum (Oligo Peptide-10) and reduce deep inflammation (KPV) are particularly relevant. The anti-inflammatory power of GHK-Cu also helps manage the intense redness and swelling that hormonal cysts produce. Peptides recommended for women often include those specifically addressing hormonal skin concerns. For women navigating hormonal changes, peptide options for women over 40 and peptides for perimenopause address the intersection of hormonal shifts and skin health.
Comedonal acne
Comedonal acne, the kind dominated by blackheads and whiteheads without much inflammation, responds well to sebum-regulating and cell-turnover-promoting peptides. Oligo Peptide-10 for sebum control, combined with Matrixyl for cell turnover support, addresses the primary drivers without introducing the inflammation that more aggressive treatments can cause. Pairing these peptides with salicylic acid for pore clearing creates an effective comedonal acne strategy.
Inflammatory acne
Red, swollen papules and pustules. This is where anti-inflammatory peptides shine brightest. KPV to block the NF-kB cascade. GHK-Cu to calm tissue-level inflammation and promote rapid healing. Palmitoyl Tetrapeptide-7 for its dual anti-inflammatory and antibacterial action. The complete guide to inflammation peptides covers the full range of options for managing inflammatory skin conditions.
Cystic and nodular acne
The most severe forms of acne, deep cysts and nodules that can cause permanent scarring, often require a more intensive approach. Topical peptides alone may not penetrate deeply enough to address these lesions effectively. This is where injectable peptides like BPC-157 and TB-500 offer advantages, delivering healing and anti-inflammatory molecules directly to the tissue level where the damage is occurring. Understanding the full spectrum of tissue repair peptides provides context for building a comprehensive protocol for severe acne management.
Post-acne skin: hyperpigmentation and texture
Even after active acne resolves, many people are left with a legacy of dark spots, uneven texture, and visible scars. For post-inflammatory hyperpigmentation, the combination of GHK-Cu, niacinamide, and vitamin C addresses melanin overproduction through multiple pathways. For textural scarring, Matrixyl and BPC-157 promote the collagen remodeling needed to fill atrophic scars and smooth the skin surface. The peptide approach to dark circles and discoloration shares overlapping mechanisms with PIH treatment.
Peptides, the skin microbiome, and acne
The skin microbiome has emerged as a critical factor in acne research, and peptides interact with it in ways that distinguish them from conventional treatments.
Why antibiotics damage the microbiome
Broad-spectrum antibiotics used for acne, whether topical or oral, do not just kill C. acnes. They kill beneficial bacteria too. The skin microbiome is a delicate ecosystem of hundreds of bacterial species, fungi, and viruses that work together to maintain skin health. When antibiotics wipe out this ecosystem indiscriminately, the result can be opportunistic infections, increased sensitivity, and paradoxically, a skin environment that becomes even more hospitable to acne-causing organisms once the antibiotic course ends.
How peptides preserve microbial balance
Antimicrobial peptides, both naturally produced and therapeutically applied, tend to be more selective than antibiotics. Many AMPs preferentially target pathogenic bacteria while sparing commensal organisms that contribute to skin health. This selectivity means that peptide-based approaches to acne can reduce C. acnes overgrowth without causing the collateral microbiome damage that antibiotics produce. The implications extend beyond the skin. Oral antibiotics for acne also disrupt the gut microbiome, and the connection between gut health and skin health is well-established in dermatological research.
Collagen peptides and the acne question
One frequently asked question deserves direct attention: can collagen peptides cause acne? Oral collagen supplements are extremely popular, and some users report breakout flares after starting supplementation. The evidence suggests that this is relatively uncommon and may be related to specific formulation ingredients rather than the collagen peptides themselves. Understanding the difference between collagen hydrolysate and collagen peptides can help navigate this concern, as molecular weight and processing methods affect how the body responds.
For topical collagen peptides, the risk of acne exacerbation is minimal when the product is formulated correctly. The key is choosing non-comedogenic formulations from reputable sources. The question of collagen peptides and weight gain and collagen peptides and weight loss also comes up, reflecting the broader interest in how these supplements affect overall body composition, which in turn can influence hormonal acne through insulin sensitivity and hormonal balance pathways.
Argireline and sebum control: the unexpected connection
Argireline, or Acetyl Hexapeptide-8, is primarily known as a "Botox alternative" for wrinkle reduction. Its mechanism of action, inhibiting SNARE complex formation to reduce muscle contraction, is what earns it that reputation. But there is a lesser-known aspect of Argireline that makes it relevant for acne: it helps balance oil production.
Research indicates that Argireline can modulate sebum secretion, potentially reducing the excess oiliness that contributes to comedone formation and bacterial overgrowth. For people with oily, acne-prone skin who are also concerned about fine lines (a common combination, especially in the late twenties and thirties), Argireline offers dual benefits without the irritation that many anti-aging actives cause on acne-prone skin. Understanding the comparison between peptides and Botox provides context for how topical peptides like Argireline fit into the broader anti-aging and skin-health landscape.
The Snap-8 peptide, a next-generation version of Argireline with an eight-amino-acid chain instead of six, offers similar benefits with potentially improved efficacy. Syn-Ake, another neuromuscular peptide, rounds out the category of signal peptides that offer indirect benefits for acne-prone skin through sebum modulation and skin texture improvement.
Natural peptides in acne management
Not all effective peptides come from a laboratory. Some of the most interesting recent research involves peptides derived from natural sources.
Burdock root peptides
A panel of 46 peptides isolated from burdock root demonstrated significant anti-acne properties in laboratory studies. These peptides showed antibacterial activity against gram-positive bacteria, including those relevant to acne pathogenesis. Importantly, they were not toxic to fibroblast cultures, indicating safety for surrounding skin tissue. Burdock root has been used in traditional medicine for skin conditions for centuries, and identifying the specific peptide components responsible for its benefits opens the door to more targeted and effective formulations.
Marine and plant-derived peptides
The broader category of natural peptides for skin includes marine-derived AMPs, plant defensins, and insect-derived peptides that show promise against acne-related bacteria. Marine collagen peptides specifically have gained attention for their bioavailability and skin health benefits, including support for the skin barrier integrity that is crucial for acne prevention.
Bioregulator peptides
An emerging category of bioregulator peptides represents small peptide sequences that regulate specific organ and tissue functions. While the primary research focus has been on aging and organ health, the skin-specific bioregulator peptides offer intriguing possibilities for long-term acne management by normalizing the cellular processes that become dysregulated in acne-prone skin.
The cost and accessibility of peptide acne treatment
A practical conversation about peptides for acne must address the reality of cost. Not every peptide approach carries the same price tag, and understanding the economics helps you allocate your skincare budget where it will have the most impact.
Topical peptide serums
Quality peptide serums vary widely in price, from affordable drugstore options to premium clinical formulations. The active peptide concentration, formulation quality, stability mechanisms, and delivery technology all influence the price. Higher price does not always mean better results, but extremely cheap peptide products often contain peptides at concentrations too low to produce meaningful effects. The guide on how much peptides cost provides a comprehensive overview across different categories and formats. The peptide cost calculator can help estimate ongoing expenses based on your specific protocol.
Injectable peptides
Injectable peptides like BPC-157 and TB-500 represent a higher investment due to the cost of the peptides themselves plus reconstitution supplies (bacteriostatic water, insulin syringes, alcohol swabs). The complete guide to peptide therapy costs breaks down the full financial picture. For those considering working with a practitioner, finding peptide therapy providers and understanding the clinic landscape helps make informed decisions. Online peptide therapy options have also expanded access for many people.
Source quality matters
Not all peptide products are created equal. For topical serums, look for products that list specific peptide names and concentrations, use airless pump packaging that protects against oxidation, and come from brands with third-party testing documentation. For injectable peptides, sourcing from reputable vendors who provide certificates of analysis is not optional, it is essential for safety. The guide on best peptide vendors and peptide testing labs covers quality verification in detail. Understanding current peptide regulations and legality also ensures you are making informed, compliant decisions about your peptide use.
The future of peptide-based acne treatments
The peptides available for acne today represent only the beginning. Several research directions promise to transform how we treat acne in the coming years.
AI-designed antimicrobial peptides
In a landmark study published in Nature, researchers used deep learning algorithms to design 42 novel antimicrobial peptides. Of these, five showed high potency against C. acnes with minimum inhibitory concentrations of just 2-4 micrograms per milliliter. This approach, using artificial intelligence to scan the vast space of possible amino acid sequences and identify those with optimal antimicrobial properties, represents a paradigm shift in drug discovery. Instead of testing thousands of natural compounds hoping to find one that works, AI can predict and design peptides tailored to specific targets.
The implications for acne treatment are profound. Imagine antimicrobial peptides custom-designed to target the specific C. acnes strains prevalent in a patient skin, optimized for stability, penetration, and minimal side effects. This is not science fiction. The technology exists today. The pipeline from laboratory to clinical application is the remaining hurdle.
The peptide vaccine approach
Researchers at the University of California, San Diego are developing a peptide-based vaccine against acne. Instead of treating breakouts after they form, this approach trains the immune system to prevent them. The vaccine targets hyaluronidase, an enzyme produced by C. acnes that breaks down hyaluronic acid in the skin and contributes to tissue damage and inflammation.
In mouse studies, vaccinated animals showed reduced acne severity scores and lower levels of IL-1beta, a key inflammatory cytokine in acne. The concept is revolutionary. A single vaccination series could potentially provide long-term protection against the inflammatory cascade that drives acne, eliminating the need for daily topical treatments or chronic medication use. While clinical trials in humans are still in early stages, the preliminary data is encouraging enough that this approach is being actively pursued.
Next-generation delivery systems
One of the biggest limitations of current peptide-based acne treatments is delivery. Getting peptide molecules through the skin barrier in sufficient quantities and to the right depth remains a technical challenge. Emerging delivery technologies, including nanoparticle encapsulation, microneedle patches, lipid-based carriers, and cell-penetrating peptide conjugates, promise to dramatically improve the bioavailability of topical peptides.
Microneedle patches deserve special attention. These thin, adhesive patches contain hundreds of microscopic needles that painlessly penetrate the stratum corneum and deliver their peptide payload directly into the epidermis and upper dermis. For acne, this could mean targeted delivery of antimicrobial and anti-inflammatory peptides directly to the depth where C. acnes colonies and inflammatory cells reside. The technology already exists for other applications and is being adapted for acne treatment.
Personalized peptide protocols
The future of acne treatment is personalization. As skin microbiome testing becomes more accessible and genomic analysis identifies individual susceptibility factors, peptide protocols can be tailored to each person unique acne drivers. Someone with predominantly microbial-driven acne might receive a different peptide combination than someone whose acne is primarily hormonal or primarily inflammatory. SeekPeptides tracks these developments closely, providing members with current information on emerging peptide research and practical applications as the field evolves.
Combining lifestyle factors with peptide treatment
Peptides do not work in isolation. The biological environment in which they operate, your overall health, diet, stress levels, sleep quality, affects how effectively they can do their job.
Diet and acne: the mTOR connection
Remember the IGF-1/PI3K/Akt/mTOR pathway discussed earlier? This signaling cascade is directly influenced by diet. High-glycemic foods cause insulin spikes that activate mTOR, driving sebum production and keratinocyte proliferation. Dairy products, particularly skim milk, have been associated with increased acne severity in multiple studies, potentially through IGF-1 content. A diet that emphasizes low-glycemic foods, healthy fats, and adequate protein creates an internal environment where peptides can work more effectively because the underlying hormonal and inflammatory drivers are modulated.
Sleep and skin repair
Collagen synthesis, cellular repair, and immune regulation all peak during sleep. If you are using peptides to promote healing and collagen production (Matrixyl, GHK-Cu, BPC-157), inadequate sleep directly undermines their effectiveness. Seven to nine hours of quality sleep creates the optimal biological backdrop for peptide-mediated skin repair. For those exploring peptides for overall wellness, DSIP peptide benefits specifically relate to sleep regulation, which indirectly supports skin health.
Stress and cortisol
Chronic stress elevates cortisol, which increases sebum production, impairs wound healing, compromises the skin barrier, and amplifies inflammatory responses. All of these effects directly counteract what peptides are trying to accomplish. Stress management is not an optional add-on to a peptide acne routine. It is a fundamental requirement for getting the most out of your investment. Peptides for anxiety and stress management represent another avenue where peptide science intersects with skin health.
Exercise and skin health
Regular exercise improves circulation, which enhances nutrient delivery to skin cells and supports the removal of waste products. It reduces insulin resistance, which helps modulate the mTOR pathway. And it promotes lymphatic drainage, which can reduce facial puffiness and improve the clearance of inflammatory mediators from acne-affected skin. The connection between athletic performance peptides and skin health is indirect but real. Improved fitness creates systemic improvements that benefit every organ, including the skin.
Understanding peptide safety for acne treatment
Safety is non-negotiable. Before incorporating any peptide into your acne routine, understanding the risk profile is essential.
Topical peptide safety
The safety profile of topical peptides is generally excellent. GHK-Cu, Matrixyl, Palmitoyl Tetrapeptide-7, Argireline, and other established skincare peptides have extensive safety data from both clinical trials and decades of consumer use. Side effects are rare and typically mild: temporary redness, mild tingling, or slight irritation during the adjustment period. Allergic reactions are possible but uncommon.
The most important safety consideration with topical peptides is not the peptides themselves but the other ingredients in the formulation. Fragrances, preservatives, silicones, and comedogenic carriers can all cause problems for acne-prone skin. Read ingredient lists carefully. The comprehensive peptide safety guide covers both topical and injectable safety considerations in detail.
Injectable peptide safety
Injectable peptides carry additional considerations. Sterile technique must be maintained to prevent infection. Peptide purity and source quality directly impact safety. Dosing accuracy matters, and the peptide calculator helps ensure precise preparation. Understanding what water to use for reconstitution and proper storage conditions are practical safety requirements for anyone using injectable peptides.
For BPC-157 specifically, the question of regulatory status is worth understanding. Peptide legality varies by jurisdiction, and staying informed about current regulations is part of responsible use. The comparison between peptides and SARMs is relevant here because they occupy different regulatory categories with different risk profiles, and understanding these distinctions matters.
Interactions and contraindications
Peptides used for acne can interact with other treatments. Retinoids can increase the penetration of topical peptides, which may increase both effectiveness and the potential for irritation. Immunosuppressive medications may alter the response to anti-inflammatory peptides. Anyone taking prescription acne medications (isotretinoin, spironolactone, oral antibiotics) should discuss peptide use with their healthcare provider to avoid unintended interactions. Resources on cycling different peptides address how to structure multi-peptide protocols safely over time.
Frequently asked questions
Which peptide is best for cystic acne?
For cystic acne, KPV stands out because of its potent NF-kB pathway inhibition, which directly targets the deep inflammatory response that characterizes cystic lesions. GHK-Cu supports healing once the inflammation is controlled. For severe cases, injectable BPC-157 can deliver anti-inflammatory and tissue repair benefits at the tissue level where cystic acne resides. A combined approach using KPV for inflammation control, GHK-Cu for healing support, and BPC-157 for deep tissue repair addresses all aspects of cystic acne pathology.
Can I use peptides if I am on accutane (isotretinoin)?
Isotretinoin dramatically thins the skin and increases sensitivity. Topical peptides, particularly gentle ones like GHK-Cu, may actually help support the skin barrier during isotretinoin treatment, but this should be discussed with your prescribing dermatologist. Avoid injectable peptides during isotretinoin treatment without medical guidance. After completing isotretinoin, peptides can play a valuable role in rebuilding skin health and addressing any residual scarring.
Are peptide serums safe for sensitive, acne-prone skin?
Yes. Peptides are among the gentlest actives available for acne-prone skin. Unlike retinoids, benzoyl peroxide, and chemical exfoliants, peptides do not strip, dry, or irritate the skin. GHK-Cu and Matrixyl in particular are well-tolerated by even the most sensitive skin types. Always patch test any new product on a small area before applying it to your entire face, and introduce one new product at a time with at least two weeks between additions.
How do peptides compare to prescription acne treatments?
Peptides and prescription treatments target acne through different mechanisms and are not mutually exclusive. Prescription retinoids excel at normalizing cell turnover. Prescription antibiotics kill bacteria (though with resistance concerns). Isotretinoin shuts down sebaceous gland activity. Peptides offer anti-inflammatory, antimicrobial, healing, and collagen-building benefits with minimal side effects. Many dermatologists are beginning to recommend peptides as complementary to, rather than replacements for, prescription treatments. The clinical peptide therapy landscape reflects this integrative approach.
Can peptides prevent acne or only treat existing breakouts?
Peptides can do both. Sebum-regulating peptides like Oligo Peptide-10 reduce the excess oil that initiates comedone formation, working preventively. Anti-inflammatory peptides maintain a lower baseline inflammatory state in the skin, raising the threshold for breakout triggering. Barrier-supporting peptides keep the skin resilient against environmental insults that can trigger acne flares. Used consistently as part of a daily routine, peptides function as both treatment and prevention.
Do topical peptides interact with birth control or hormonal medications?
Topical peptides are not systemically absorbed in significant quantities and do not interact with hormonal medications, including birth control pills or hormone replacement therapy. Injectable peptides like KPV or BPC-157 reach systemic circulation and theoretically could interact with certain medications, though significant interactions have not been documented in the research literature. As always, inform your healthcare provider about all substances you are using, including peptides.
What is the minimum effective concentration for GHK-Cu in acne treatment?
Research suggests that GHK-Cu concentrations as low as 0.01% can produce measurable effects on gene expression in skin cells, but for practical acne treatment benefits, concentrations discussed in the concentration guide are more appropriate. Higher is not always better with copper peptides, as excessive concentrations can potentially be pro-oxidant rather than antioxidant. The therapeutic window is well-defined and favors moderate, consistent application over aggressive dosing.
Can I use peptides for body acne (back, chest, shoulders)?
Absolutely. The same peptide mechanisms that work on facial acne apply to body acne. The main practical challenge is application coverage, since body acne affects larger surface areas.
Peptide body lotions and sprays can address this.
For injectable peptides, subcutaneous administration provides systemic delivery that reaches all skin regardless of location. Body acne, particularly on the back and shoulders, often involves deeper lesions that may benefit from the tissue-level delivery that injectable peptides provide.
External resources
Antimicrobial peptides and the skin immune defense system - Comprehensive review in the Journal of Dermatological Science covering the role of endogenous AMPs in skin health and disease.
American Academy of Dermatology: Acne resource center - Evidence-based acne information from the leading dermatology professional organization.
GHK-Cu peptide: biological activity and potential therapeutic applications - Published review of copper peptide research spanning wound healing, anti-inflammatory, and tissue remodeling applications.
For anyone serious about understanding peptides for acne, SeekPeptides offers one of the most comprehensive educational platforms available. Members gain access to detailed peptide profiles, dosing protocols, stacking guides, and regularly updated research summaries that translate complex science into practical, actionable information. Whether you are exploring topical peptides for the first time or building an advanced multi-peptide protocol for stubborn acne and scarring, SeekPeptides membership provides the depth of knowledge and community support that makes the difference between guessing and knowing exactly what you are doing.



