Jan 22, 2026
Your body is on fire. Not the kind you can see, but something far more destructive. Chronic inflammation eats away at your joints, your gut, your brain. It ages you from the inside out. And the worst part? Most people have no idea it is happening until the damage becomes irreversible.
Traditional anti-inflammatory drugs come with a price. NSAIDs destroy your gut lining. Steroids suppress your immune system. And neither addresses the root cause of inflammation, they just mask the symptoms while the underlying fire continues to burn.
This is where peptides change everything.
Anti-inflammatory peptides work differently. They do not simply block pain signals or suppress immune responses. Instead, they modulate the inflammatory cascade at its source, calming overactive immune pathways while promoting genuine tissue repair. Research published in the Journal of Inflammation Research shows that bioactive peptides can reduce pro-inflammatory cytokines like TNF-alpha and IL-6 without the devastating side effects of conventional medications.
This guide covers the most effective peptides for inflammation, from the gut-healing power of KPV to the tissue-regenerating capabilities of BPC-157 and TB-500. You will learn exactly how these compounds work, which conditions they target best, and how to use them safely. Whether you are dealing with autoimmune flares, chronic joint pain, or systemic inflammation that refuses to resolve, peptide therapy offers a path forward that conventional medicine cannot match.
Understanding inflammation and why it matters
Inflammation is not your enemy. At least, not always. Acute inflammation is your body doing its job, rushing immune cells and healing factors to damaged tissue, fighting off invaders, and initiating repair. Cut your finger, and inflammation seals the wound. Catch a virus, and inflammation helps destroy it.
The problem starts when inflammation refuses to turn off.
Chronic inflammation is different. It persists for weeks, months, even years. Instead of healing, it damages. Instead of protecting, it destroys. The same immune responses that save your life in acute situations become weapons turned inward when they become chronic.
Research from the peptide research community shows that chronic inflammation underlies virtually every major disease. Heart disease. Cancer. Alzheimer's. Diabetes. Autoimmune conditions. Depression. The inflammatory markers elevated in these conditions are not coincidental. They are causal.
The inflammatory cascade explained
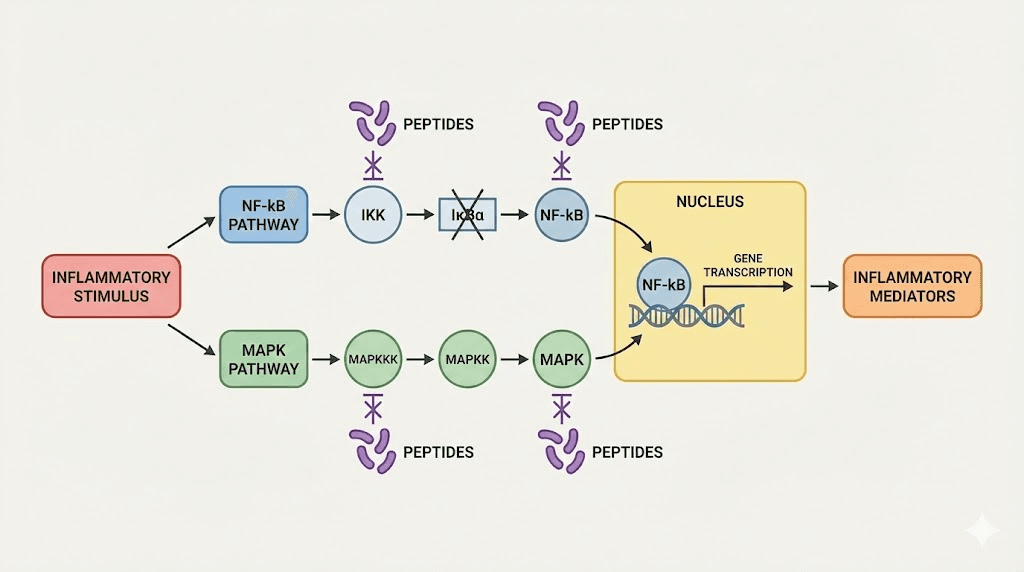
Understanding how peptides work requires understanding the inflammatory cascade itself. When tissue damage or infection occurs, your body initiates a complex signaling sequence involving multiple pathways.
The NF-kB pathway is central. Nuclear factor kappa-light-chain-enhancer of activated B cells, to use its full name, acts as a master switch for inflammatory gene expression. When activated, NF-kB triggers the production of pro-inflammatory cytokines including TNF-alpha, IL-1beta, IL-6, and dozens of others. These cytokines recruit immune cells, increase vascular permeability, and initiate the inflammatory response.
The MAPK pathway runs parallel. Mitogen-activated protein kinases amplify inflammatory signals and regulate cellular responses to stress. When chronically activated, this pathway drives sustained inflammation and tissue damage.
Anti-inflammatory peptides interrupt these cascades at multiple points. Unlike NSAIDs, which simply block COX enzymes downstream, peptides modulate the master regulatory switches themselves. This upstream intervention is why peptide therapy produces more comprehensive anti-inflammatory effects with fewer side effects.
Signs you are dealing with chronic inflammation
Chronic inflammation does not announce itself with the obvious redness and swelling of acute inflammation. It is subtle. Insidious. Many people live with it for years without realizing the fire burning inside them.
Persistent fatigue that sleep does not resolve. Joint pain that moves around and never fully disappears. Brain fog and difficulty concentrating. Digestive issues that defy diagnosis. Skin problems that flare and recede without clear triggers. Slow wound healing. Frequent infections. Weight gain around the midsection that resists diet and exercise.
These symptoms share a common root. Elevated inflammatory markers like C-reactive protein, homocysteine, and fibrinogen indicate systemic inflammation even when specific symptoms vary. Understanding peptide safety and mechanisms becomes crucial when addressing these underlying inflammatory drivers.
The best peptides for inflammation
Not all peptides address inflammation equally. Some target specific tissues. Others work systemically. Understanding which peptide matches your specific inflammatory condition is essential for optimal results. The complete peptide list includes dozens of compounds, but a handful stand out for anti-inflammatory applications.
BPC-157: the body protection compound
BPC-157 is a 15-amino-acid peptide fragment derived from a protein found in human gastric juice. Its name, Body Protection Compound, reflects its remarkable ability to protect and heal damaged tissue throughout the body.
The anti-inflammatory mechanisms of BPC-157 operate through multiple pathways. It modulates the nitric oxide system, promoting vasodilation and improved blood flow to damaged tissues. It activates growth hormone receptors without raising systemic growth hormone levels. It influences the dopaminergic and serotonergic systems, which partially explains its effects on gut-brain axis inflammation.
Research shows BPC-157 decreases levels of TNF-alpha and IL-6, two of the most destructive pro-inflammatory cytokines. Unlike immunosuppressive drugs, BPC-157 does not simply shut down immune function. It modulates the inflammatory response toward resolution rather than suppression.
The peptide shows particular promise for gastrointestinal inflammation. Studies demonstrate protection against inflammatory bowel disease, gastric ulcers, and intestinal damage from NSAIDs. For anyone whose gut lining has been compromised by chronic NSAID use, BPC-157 offers a path to healing that the drugs themselves cannot provide.
Musculoskeletal inflammation also responds remarkably well. Tendon injuries, ligament damage, and joint inflammation show accelerated healing in animal models. The best peptides for tendon repair consistently include BPC-157 at the top of the list.
Typical research protocols use 200-300mcg administered subcutaneously twice daily. The BPC-157 dosage calculator can help determine exact amounts based on body weight. Most protocols run 4-6 weeks, though some conditions require longer intervention. Learn more about how to take BPC-157 for detailed administration guidance.
KPV: the gut inflammation specialist
KPV is a tripeptide, just three amino acids: lysine, proline, and valine. Despite its small size, this fragment of alpha-melanocyte stimulating hormone packs enormous anti-inflammatory power. KPV peptide benefits center primarily on its ability to resolve gut and skin inflammation.
The mechanism is elegant. KPV directly inhibits NF-kB activation, preventing the nuclear translocation that triggers inflammatory gene expression. It suppresses pro-inflammatory cytokine release including IL-1beta, IL-6, and TNF-alpha. It reduces the production of reactive oxygen species that damage tissue during inflammation.
For inflammatory bowel conditions, KPV peptide for inflammation demonstrates remarkable efficacy. Research in colitis models shows KPV improves mucosal healing, reduces intestinal permeability, and decreases inflammatory cell infiltration. Users report improvements in Crohn's disease, ulcerative colitis, and IBS symptoms that failed to respond to conventional treatments.
Skin inflammation responds equally well. Dermatitis, psoriasis flares, and wound healing all improve with KPV administration. The peptide accelerates wound closure while reducing scarring and immune cell infiltration, a combination conventional treatments rarely achieve.
The KPV peptide dosage guide recommends starting at 200-400mcg daily, though doses up to 1mg show good tolerability. One advantage of KPV is its versatility in administration routes. Subcutaneous injection works well for systemic effects, but oral and even topical application show efficacy for localized inflammation. Check the KPV morning or night guide for optimal timing.
TB-500 (thymosin beta-4): tissue regeneration and inflammation control
TB-500, the synthetic version of thymosin beta-4, is a 43-amino-acid peptide found throughout the human body with highest concentrations in platelets and white blood cells at wound sites. This positioning is not accidental. Thymosin beta-4 is a master regulator of tissue repair and inflammation resolution.
The TB-500 benefits extend far beyond simple anti-inflammatory effects. The peptide promotes angiogenesis, creating new blood vessels to supply healing tissue. It enhances cell migration, helping repair cells reach injury sites. It regulates actin, a structural protein critical for cellular movement and wound closure. It decreases fibrosis, preventing excessive scar formation.
For inflammation specifically, TB-500 downregulates inflammatory cytokines while promoting anti-inflammatory mediators. Studies show reduced levels of IL-1, IL-6, and TNF-alpha in treated tissues. Wounds treated with TB-500 exhibit more organized collagen alignment and lower inflammatory cell counts compared to untreated controls.
The peptide excels for musculoskeletal inflammation. Joint injuries, muscle strains, and tendon damage all respond well. The best peptides for injury recovery almost always include TB-500 for its dual action on inflammation and tissue regeneration. The TB-500 dosage calculator can help determine appropriate amounts based on injury severity and body weight.
Standard protocols use 2-2.5mg twice weekly during loading phases, transitioning to once weekly for maintenance. Most users run 4-6 week cycles, though chronic conditions may require longer protocols.
Thymosin alpha-1: immune modulation and chronic inflammation
Thymosin alpha-1 represents a different approach to inflammation. Rather than directly suppressing inflammatory pathways, this thymic peptide modulates immune function to restore balance. For inflammation driven by immune dysfunction, autoimmunity, or chronic infection, thymosin alpha-1 addresses root causes rather than symptoms.
The peptide enhances T-cell function, restores immune balance, and improves resistance to both viral and bacterial pathogens. It is particularly valuable for immune exhaustion, where the immune system has become simultaneously overactive in some ways and underactive in others, the hallmark of autoimmune conditions and chronic infections.
Research demonstrates thymosin alpha-1 reduces inflammatory markers in chronic viral infections, autoimmune conditions, and even cancer-related inflammation. The peptide does not suppress immune function like steroids. Instead, it rebalances it, enhancing beneficial immune activity while dampening excessive inflammatory responses.
The best peptides for immune system support typically include thymosin alpha-1 as a cornerstone for anyone dealing with chronic infections or autoimmune inflammation.
Typical protocols use 1.6mg administered subcutaneously 2-3 times weekly. Some conditions require daily dosing during acute phases. Protocol length varies significantly based on the condition being addressed, from 4 weeks for acute support to ongoing maintenance for chronic autoimmune conditions.
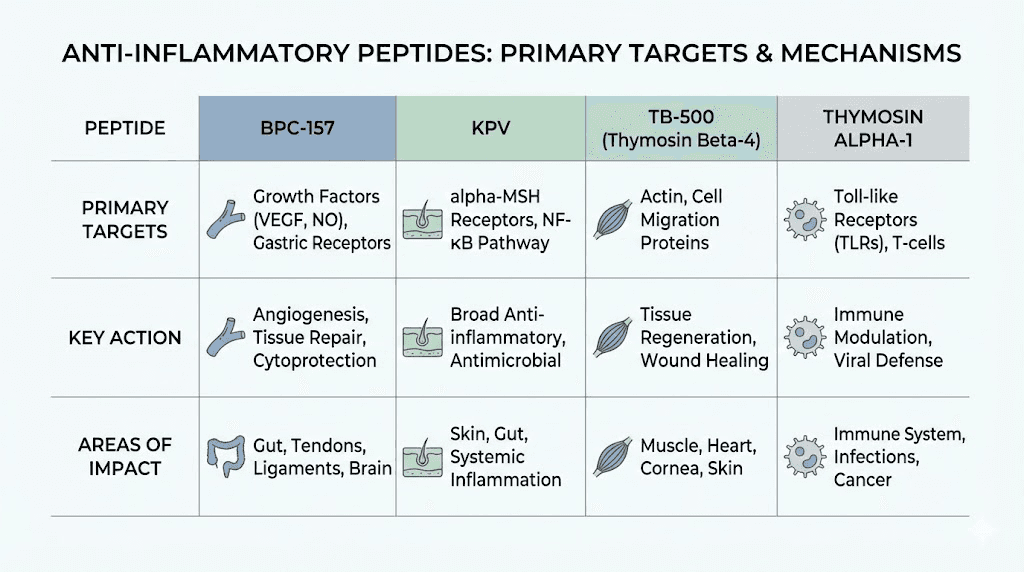
GHK-Cu: copper peptide anti-inflammatory effects
GHK-Cu is a naturally occurring copper-binding peptide that decreases significantly with age. While primarily known for skin and hair benefits, GHK-Cu demonstrates potent anti-inflammatory effects that extend far beyond cosmetic applications.
The peptide reduces the expression of inflammatory genes while upregulating genes associated with tissue remodeling and repair. Research shows GHK-Cu decreases production of TGF-beta, a cytokine associated with excessive inflammation and fibrosis. It modulates iron levels in tissues, reducing oxidative stress that drives inflammatory damage.
For skin inflammation specifically, copper peptides show remarkable efficacy. Dermatitis, inflammatory acne, and wound healing all improve. The copper peptides for acne scars protocol addresses both the inflammatory component of acne and the tissue remodeling needed for scar reduction.
Systemic GHK-Cu administration for inflammation typically uses 1-2mg daily via subcutaneous injection. The GHK-Cu peptide dosage guide covers both injectable and topical protocols. The GHK-Cu dosage chart provides weight-based calculations for optimal dosing.
VIP: vasoactive intestinal peptide
VIP is a naturally occurring peptide produced in the brain and gastrointestinal tract.
It binds to class II G-protein-coupled receptors and demonstrates broad anti-inflammatory effects across multiple organ systems.
The peptide is particularly valuable for reducing inflammation in the heart, GI tract, central nervous system, and joints. It modulates immune cell activity, reducing the release of pro-inflammatory mediators while promoting regulatory T-cell function. For neuroinflammation specifically, VIP crosses the blood-brain barrier and directly addresses central nervous system inflammation.
Researchers explore VIP for conditions ranging from inflammatory bowel disease to rheumatoid arthritis to neurological conditions with inflammatory components. Its broad spectrum of activity makes it valuable for systemic inflammation affecting multiple organ systems.
LL-37: the antimicrobial anti-inflammatory
LL-37, also called cathelicidin, represents a unique class of antimicrobial peptide with significant anti-inflammatory properties.
The human body produces LL-37 as part of innate immune defense, but supplementation can enhance its anti-inflammatory effects.
Unlike most anti-inflammatory compounds, LL-37 simultaneously fights infection while controlling inflammatory responses. This dual action makes it particularly valuable for inflammation driven by chronic or low-grade infections. The peptide disrupts bacterial membranes while modulating host inflammatory responses to prevent excessive tissue damage.
Research shows LL-37 reduces inflammatory markers in wound healing, respiratory infections, and skin conditions. It promotes resolution of inflammation rather than simple suppression, allowing beneficial immune responses while preventing excessive damage.
Inflammation peptides for specific conditions
Different inflammatory conditions respond best to different peptide approaches. Understanding which peptides target your specific type of inflammation optimizes results while minimizing unnecessary complexity.
Gut inflammation and inflammatory bowel conditions
The gut presents unique challenges for anti-inflammatory therapy. The intestinal lining must balance protection against pathogens with tolerance of beneficial bacteria and food antigens. Conventional anti-inflammatory drugs often damage the gut while treating inflammation elsewhere.
For peptides for gut health, BPC-157 and KPV stand out as primary options. BPC-157 protects the gut lining while promoting healing of existing damage. KPV directly suppresses intestinal inflammation through NF-kB inhibition.
A combined protocol for inflammatory bowel conditions might include BPC-157 at 250mcg twice daily plus KPV at 400mcg daily. This stacking approach addresses both tissue repair and inflammatory suppression simultaneously. Many users report improvement in IBD symptoms within 2-4 weeks, with continued gains over 8-12 week protocols.
The peptides to take with Ozempic often include BPC-157 to counter the GI side effects common with GLP-1 agonists while preserving their weight loss benefits.
Joint inflammation and arthritis
Joint inflammation requires peptides that address both the inflammatory component and the structural damage it causes. Cartilage does not heal well on its own, and chronic inflammation accelerates degeneration.
The best peptides for joint pain typically combine TB-500 for tissue regeneration with BPC-157 for anti-inflammatory effects. This combination addresses both the fire and the damage it leaves behind.
For peptides for bone and cartilage repair, adding GHK-Cu can enhance collagen synthesis and tissue remodeling. The copper peptide promotes proper extracellular matrix formation, essential for functional joint repair rather than scar tissue.
Protocols for joint inflammation typically run 8-12 weeks minimum, as cartilage regeneration is slow even with peptide support. Many users transition to maintenance protocols after initial healing, using lower doses long-term to prevent recurrence.
Autoimmune inflammation
Autoimmune conditions present the most challenging inflammatory situations. The immune system attacks the body's own tissues, and conventional treatments suppress immune function broadly, increasing infection risk while sometimes failing to control the autoimmune process.
Thymosin alpha-1 offers a different approach. By rebalancing immune function rather than suppressing it, the peptide can reduce autoimmune inflammation while preserving beneficial immune responses. This immunomodulatory effect makes thymosin alpha-1 valuable for conditions from rheumatoid arthritis to Hashimoto's thyroiditis to lupus.
Combining thymosin alpha-1 with tissue-specific peptides addresses both the systemic immune dysfunction and local tissue damage. For autoimmune joint conditions, adding TB-500 supports tissue repair. For autoimmune gut conditions, adding BPC-157 and KPV protects and heals the intestinal lining.
The best peptides for fibromyalgia, often considered an autoimmune or neuroimmune condition, typically include this combination approach addressing both inflammation and tissue healing.
Neuroinflammation and brain health
Neuroinflammation underlies conditions from Alzheimer's disease to depression to chronic fatigue. The blood-brain barrier complicates treatment, as many compounds cannot reach the central nervous system where inflammation occurs.
Several peptides cross the blood-brain barrier effectively. VIP directly addresses neuroinflammation. Semax and Selank, while primarily considered nootropic peptides, demonstrate significant anti-inflammatory effects in the central nervous system. The best peptides for brain function often work partially through reducing neuroinflammation.
BPC-157 also shows neuroprotective and anti-inflammatory effects in brain tissue, despite being primarily known for peripheral tissue repair. Animal studies demonstrate protection against neurotoxins and inflammatory brain damage.
For peptides for anxiety, addressing neuroinflammation often produces benefits that pure anxiolytics cannot match. The inflammatory component of mood disorders is increasingly recognized, and anti-inflammatory peptides offer a mechanistically different approach.
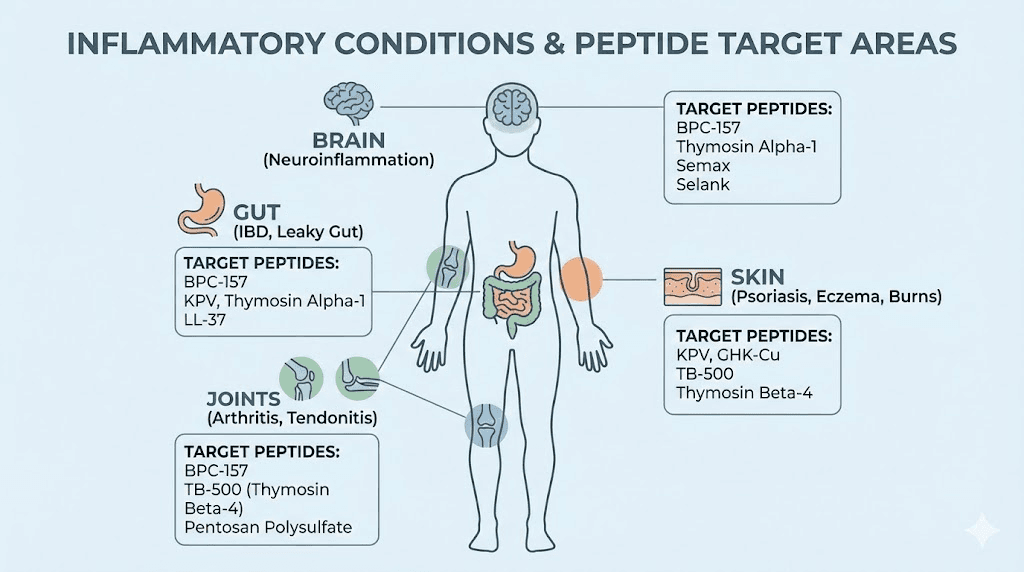
Skin inflammation and dermatological conditions
Skin inflammation presents both challenges and opportunities for peptide therapy. The skin is accessible, allowing topical application in addition to systemic treatment. But skin conditions often reflect deeper systemic inflammation that topical treatment alone cannot address.
For inflammatory skin conditions, GHK-Cu and KPV both demonstrate significant efficacy. Copper peptides before and after results show dramatic improvements in inflammatory acne, rosacea, and eczema. The best copper peptide serum options deliver anti-inflammatory benefits directly to affected skin.
For systemic skin inflammation, particularly conditions like psoriasis that reflect immune dysfunction, combining topical and injectable approaches produces better results than either alone. Thymosin alpha-1 addresses the underlying immune dysregulation while topical peptides manage local symptoms.
The peptides for skin tightening often work partially through anti-inflammatory mechanisms, as chronic low-grade inflammation contributes to skin aging and loss of elasticity.
Post-injury and surgical inflammation
Acute inflammation following injury or surgery serves a purpose, but excessive or prolonged inflammatory responses delay healing and increase complications. Peptides offer a way to modulate post-injury inflammation without completely suppressing the beneficial immune responses needed for healing.
The best peptides for injury recovery typically include BPC-157 and TB-500, which both reduce excessive inflammation while promoting tissue repair. This combination addresses the apparent contradiction of needing some inflammation for healing while preventing the damage of excessive inflammation.
Starting peptide protocols before surgery when possible allows tissue to begin building repair capacity before the inflammatory insult. Continuing through the post-operative period supports healing while controlling inflammation that could delay recovery.
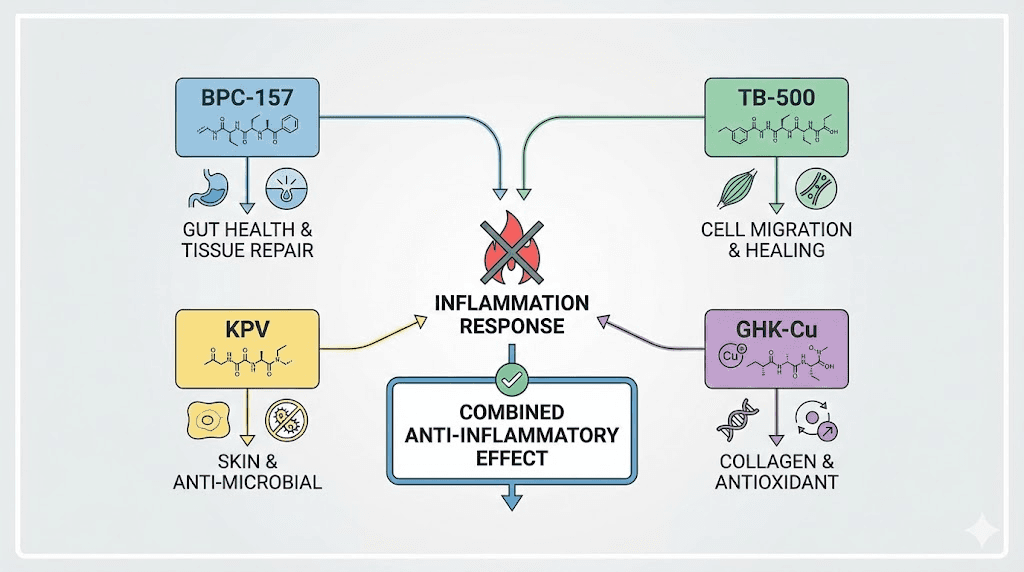
Peptide stacking for inflammation
Single peptides produce benefits, but strategic combinations often outperform individual compounds. Understanding peptide stacking principles allows you to design protocols that address your specific inflammatory situation from multiple angles.
The synergy of BPC-157 and TB-500
The BPC-157 and TB-500 combination is perhaps the most well-documented anti-inflammatory stack. The peptides work through different mechanisms that complement rather than duplicate each other.
BPC-157 modulates the nitric oxide system and reduces inflammatory cytokines directly. TB-500 promotes tissue regeneration and reduces fibrosis while independently suppressing inflammation. Together, they address both the inflammatory fire and the tissue damage it causes.
A retrospective study comparing BPC-157 alone to BPC-157 plus TB-500 for knee injections found the combination produced superior outcomes. The BPC-157 vs TB-500 comparison often misses the point, as these peptides work best together rather than as alternatives.
Standard stacking protocols use BPC-157 at 250mcg twice daily with TB-500 at 2.5mg twice weekly. This combination addresses most musculoskeletal and gut inflammation effectively.
Adding KPV for gut-focused protocols
When gut inflammation is primary, adding KPV to the BPC-157 and TB-500 stack creates what some researchers call the regenerative quad for gut healing. The combination addresses inflammation through multiple pathways while promoting tissue repair and barrier function restoration.
KPV at 400mcg daily combines well with standard BPC-157 and TB-500 doses. The addition of GHK-Cu further enhances tissue remodeling and reduces fibrosis. The Klow peptide blend represents one commercial combination of these compounds.
Immune support stacks
For inflammation driven by immune dysfunction, thymosin alpha-1 forms the foundation of effective stacks. Adding tissue-specific peptides addresses local damage while thymosin alpha-1 rebalances systemic immune function.
For autoimmune gut conditions, thymosin alpha-1 plus BPC-157 and KPV addresses both immune dysregulation and intestinal inflammation. For autoimmune joint conditions, thymosin alpha-1 plus TB-500 targets both the systemic immune dysfunction and the joint damage it causes.
Understanding how many peptides you can take at once helps design stacks that remain manageable while addressing complex inflammatory conditions.
The glow protocol for anti-aging inflammation
Chronic low-grade inflammation, sometimes called inflammaging, contributes significantly to aging. The glow peptide protocol addresses this aging-related inflammation while promoting tissue regeneration.
The glow peptide dosage typically combines GHK-Cu for skin and tissue remodeling with BPC-157 for systemic anti-inflammatory effects. Some protocols add TB-500 for enhanced regenerative capacity. The glow stack addresses both the inflammatory component of aging and the tissue degeneration it accelerates.
Administration and dosing protocols
Proper administration maximizes peptide effectiveness while minimizing waste and side effects. Understanding peptide dosing principles allows you to implement protocols confidently.
Reconstitution basics
Most research peptides come in lyophilized (freeze-dried) powder form requiring reconstitution before use. The peptide reconstitution guide covers this process in detail.
Use bacteriostatic water for reconstitution. This sterile water contains 0.9% benzyl alcohol as a preservative, allowing multiple uses from a single vial over days or weeks. Plain sterile water lacks this preservative and must be used immediately after reconstitution.
The peptide reconstitution calculator determines exact water volumes for your desired concentration. Standard practice is to reconstitute to concentrations that allow convenient dosing with insulin syringes, typically creating solutions where each 10 units equals your target dose.
Reconstituted peptides require refrigeration. The peptide fridge storage guide covers stability after reconstitution. Most peptides remain stable 2-4 weeks refrigerated, though some are more fragile.
The peptide storage guide provides specific timelines for different compounds.
Injection technique
Subcutaneous injection is the standard administration route for most anti-inflammatory peptides. The peptide injections guide covers proper technique in detail.
Inject into fatty tissue, typically the abdomen or thigh. Pinch the skin to create a fold, insert the needle at a 45-degree angle, inject slowly, release the skin, and withdraw the needle. Rotate injection sites to prevent tissue damage.
Some peptides benefit from local injection near the site of inflammation. BPC-157 for tendon injuries, for example, shows enhanced effects when injected near the damaged tissue rather than distally. However, systemic injection also produces benefits and may be more practical for chronic or systemic inflammation.
Alternative administration routes
Not all peptides require injection. Nasal spray peptides offer an alternative for certain compounds. KPV, for example, demonstrates oral bioavailability and can be taken in capsule form for gut inflammation. BPC-157 also shows activity via oral administration, though injectable forms may be more potent.
The injectable vs oral peptides comparison helps determine which route suits your specific situation. For gut-targeted effects, oral administration delivers peptides directly to the intestinal lining where they are needed. For systemic effects, injectable administration ensures predictable absorption.
Timing and cycling
Most anti-inflammatory peptides work best with consistent daily or twice-daily administration. Morning and evening dosing maintains stable levels. The peptide cycle planning guide covers timing strategies for different compounds.
Understanding how long peptides take to work helps set realistic expectations. Anti-inflammatory effects typically begin within days to weeks, though tissue regeneration effects may take longer to become apparent. Most protocols run 4-8 weeks minimum, with some conditions requiring 12 weeks or longer.
The peptide cycling guide addresses whether breaks between protocols are necessary. Unlike hormones, most peptides do not require cycling to prevent receptor downregulation. However, periodic reassessment helps determine whether continued treatment is necessary.
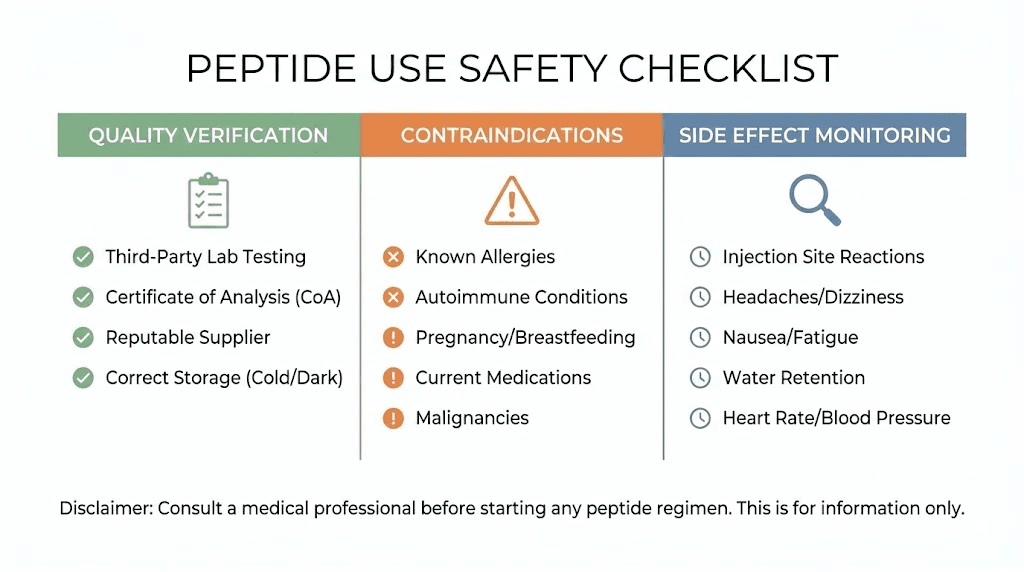
Safety considerations and side effects
Anti-inflammatory peptides demonstrate excellent safety profiles in research, but responsible use requires understanding potential risks. The peptide safety and risks guide provides comprehensive coverage of this topic.
Known side effects
Most users tolerate anti-inflammatory peptides well. Injection site reactions, including mild redness, itching, or soreness, occur occasionally and typically resolve within hours. More significant side effects are rare with standard doses.
BPC-157 occasionally causes temporary nausea or dizziness, particularly at higher doses. Some users report increased appetite. Serious side effects are rare in research literature.
KPV typically produces minimal side effects. Mild fatigue has been reported occasionally. The peptide's natural origin as a fragment of alpha-MSH contributes to its excellent tolerability.
TB-500 may cause temporary headache or flu-like symptoms, particularly during loading phases. These typically resolve within 24-48 hours. The peptide may temporarily increase inflammation before reducing it, a phenomenon sometimes called a healing crisis.
GHK-Cu at injectable doses occasionally causes injection site irritation. Topical forms rarely cause issues beyond occasional initial purging as skin turnover increases.
Contraindications and cautions
Active cancer is a concern with any growth-promoting peptide. While anti-inflammatory peptides do not cause cancer, peptides that promote tissue regeneration could theoretically accelerate existing malignancies. Anyone with known or suspected cancer should consult with their oncologist before using regenerative peptides.
Pregnancy and breastfeeding lack sufficient safety data for most peptides. Conservative practice avoids peptide use during these periods unless clearly medically necessary.
Autoimmune conditions may require caution with certain peptides. While thymosin alpha-1 can help rebalance immune function, other peptides that stimulate immune activity could theoretically worsen autoimmune flares in some individuals. Starting with low doses and monitoring responses helps identify any problematic reactions.
Quality and sourcing
Peptide quality varies dramatically between sources. Impure or degraded peptides may be ineffective or potentially harmful. The best peptide vendors provide third-party testing certificates verifying purity and identity.
Look for vendors that provide high-performance liquid chromatography (HPLC) results showing purity above 98%. Mass spectrometry results confirm the peptide identity. The peptide testing labs guide covers how to verify quality independently.
Understanding research vs pharmaceutical peptides helps set appropriate expectations. Research-grade peptides are intended for laboratory use and have not undergone the rigorous clinical trials required for pharmaceutical approval.
Drug interactions
Limited data exists on peptide interactions with conventional medications. However, peptides that affect inflammation may theoretically interact with immunosuppressive drugs, anticoagulants, or other anti-inflammatory medications.
Using anti-inflammatory peptides while taking NSAIDs may increase bleeding risk, though this has not been well-studied. The gut-protective effects of BPC-157 may help counter NSAID-induced gut damage, but this does not eliminate interaction concerns.
Anyone taking prescription medications should inform their healthcare provider before adding peptides to their regimen.
Comparing peptides to conventional anti-inflammatories
Understanding how peptides compare to conventional anti-inflammatory options helps determine when peptide therapy makes sense and when other approaches may be more appropriate.
NSAIDs: fast relief with long-term costs
Nonsteroidal anti-inflammatory drugs provide rapid pain relief by inhibiting cyclooxygenase (COX) enzymes that produce inflammatory prostaglandins. This mechanism is effective for acute inflammation but problematic for chronic use.
COX enzymes also produce protective prostaglandins in the gut, kidneys, and cardiovascular system. Chronic NSAID use damages the gastrointestinal lining, increases cardiovascular risk, and can impair kidney function. These risks increase with dose and duration.
Peptides work upstream of COX enzymes, modulating the inflammatory cascade at its source rather than blocking downstream enzymes. This mechanistic difference explains why peptides can reduce inflammation without the organ damage associated with chronic NSAID use.
For acute pain relief, NSAIDs may provide faster results. For chronic inflammation, peptides offer a safer long-term approach. Many users transition from NSAIDs to peptides, using BPC-157 to help heal the gut damage that NSAIDs caused.
Corticosteroids: powerful but problematic
Corticosteroids suppress inflammation more powerfully than any other conventional option. They work by broadly suppressing immune function and inflammatory gene expression. For severe inflammatory crises, this immunosuppression can be life-saving.
Long-term corticosteroid use, however, produces devastating side effects. Bone loss, muscle wasting, metabolic dysfunction, immune suppression, skin thinning, and adrenal suppression make chronic steroid use a last resort for most conditions.
Peptides cannot match the immediate anti-inflammatory power of corticosteroids. But they offer a sustainable alternative for chronic inflammation that does not require the dangerous tradeoffs of long-term steroid therapy. The peptides vs steroids comparison explores these differences in detail.
Biologics: targeted but expensive
Biologic drugs like adalimumab and infliximab target specific inflammatory mediators, typically TNF-alpha. These drugs revolutionized treatment of autoimmune conditions but come with significant drawbacks.
Cost is prohibitive for many patients, often exceeding $50,000 annually. Injection or infusion requirements are inconvenient. Immunosuppression increases infection risk, including reactivation of latent tuberculosis. Some patients develop antibodies that reduce drug effectiveness over time.
Peptides targeting similar inflammatory pathways cost a fraction of biologics. While less studied than FDA-approved biologics, peptides offer accessible options for those who cannot access or tolerate conventional treatments.
When to choose peptides
Peptides make the most sense for chronic inflammation that has not responded adequately to conventional treatments, or when conventional treatments produce intolerable side effects. They also make sense for prevention and optimization, addressing low-grade inflammation before it produces disease.
For acute severe inflammation, conventional medical treatment remains appropriate. Peptides work best as part of a comprehensive approach, supporting resolution of chronic inflammation while other factors, diet, stress, sleep, and exercise, address root causes.
Lifestyle factors that affect inflammation
Peptides work best in conjunction with lifestyle approaches that reduce inflammatory load. Ignoring these factors while expecting peptides to overcome them produces disappointing results.
Diet and inflammation
The standard Western diet promotes inflammation through multiple mechanisms. Excess sugar drives inflammatory cytokine production. Refined vegetable oils provide inflammatory omega-6 fatty acids while lacking anti-inflammatory omega-3s. Processed foods contain additives that disrupt gut barrier function and promote immune activation.
Anti-inflammatory diets emphasize whole foods, particularly vegetables, fatty fish, and olive oil. Eliminating or reducing sugar, refined grains, and processed foods decreases inflammatory load significantly. For some individuals, identifying and eliminating specific food sensitivities produces dramatic improvements.
Sleep and circadian rhythm
Sleep deprivation and circadian disruption directly increase inflammatory markers. A single night of poor sleep elevates C-reactive protein and inflammatory cytokines.
Chronic sleep disruption maintains elevated inflammation that peptides alone cannot overcome.
Prioritizing consistent sleep timing, adequate duration (7-9 hours for most adults), and proper sleep hygiene creates the foundation for anti-inflammatory interventions to work. Peptides cannot substitute for adequate sleep.
Stress and the inflammatory response
Psychological stress activates inflammatory pathways through cortisol dysregulation and direct neural-immune connections. Chronic stress maintains inflammatory activation even in the absence of physical triggers.
Stress management practices, meditation, breathwork, time in nature, social connection, and appropriate work-life balance reduce inflammatory burden. These practices complement peptide therapy and may enhance its effectiveness.
Exercise: the anti-inflammatory sweet spot
Moderate exercise produces anti-inflammatory effects through multiple mechanisms. It improves insulin sensitivity, reduces visceral fat (a major source of inflammatory cytokines), and directly triggers anti-inflammatory signaling pathways.
Excessive exercise, however, creates inflammation that requires recovery. Finding the individual sweet spot that produces anti-inflammatory benefits without excessive stress requires attention to recovery capacity and overall lifestyle load.
Environmental factors
Toxins, pollutants, and mold exposure drive inflammatory responses that lifestyle and peptides must work against. Addressing environmental exposures where possible reduces total inflammatory burden and improves response to anti-inflammatory interventions.
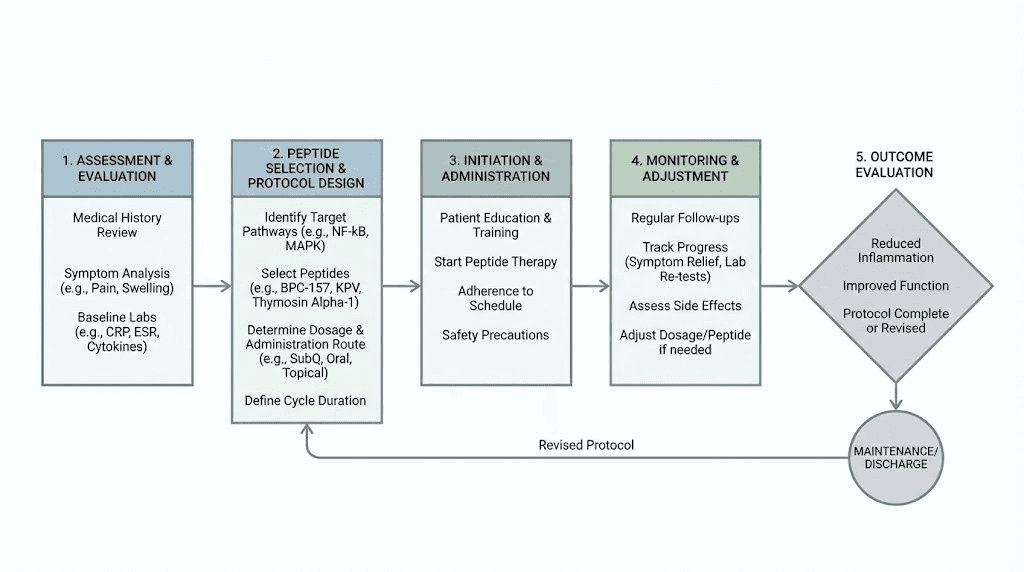
Building your anti-inflammatory protocol
Creating an effective anti-inflammatory peptide protocol requires understanding your specific situation, selecting appropriate peptides, and implementing supporting lifestyle factors.
Assessment and planning
Before starting peptides, assess your inflammatory situation. What symptoms suggest inflammation? What conditions have been diagnosed? What conventional treatments have you tried, and how well did they work? What lifestyle factors may contribute to your inflammatory load?
Blood testing for inflammatory markers, CRP, ESR, homocysteine, and specific cytokines if available, provides objective data about inflammatory status. These markers can track progress over time, though symptomatic improvement may precede marker changes.
The getting started with peptides guide provides a framework for entering the peptide world safely and systematically.
Selecting your peptides
Match peptides to your specific type of inflammation. Gut inflammation responds best to BPC-157 and KPV. Joint inflammation benefits from BPC-157 and TB-500. Autoimmune conditions often require thymosin alpha-1. Skin inflammation improves with GHK-Cu and KPV.
Starting with a single peptide allows assessment of individual response before adding complexity. Once you understand how your body responds, adding complementary peptides can enhance results.
The peptide calculator helps determine appropriate doses based on body weight and goals. The peptide stack calculator assists with planning multi-peptide protocols.
Implementation and monitoring
Start with conservative doses and increase gradually if needed. Keep notes on symptoms, energy, sleep quality, and any side effects. This documentation helps identify what works and what requires adjustment.
Allow adequate time for peptides to work. While some notice improvements within days, full benefits often take 4-8 weeks to manifest. Patience and consistency produce better results than frequently changing protocols.
Reassess periodically. Once inflammation resolves, maintenance protocols may suffice. Some conditions require ongoing treatment while others resolve and stay resolved.
Working with healthcare providers
Ideally, peptide therapy occurs under medical supervision. The peptide therapy clinics guide helps locate providers who understand peptide therapy. The peptide therapy near me resource provides location-specific information.
Many physicians remain unfamiliar with peptide therapy. Bringing research literature and explaining your goals may help educate open-minded providers. The guide to doctors prescribing peptides addresses common questions about the prescribing landscape.
For those who cannot access medical supervision, education and caution become even more critical. Understanding common peptide mistakes helps avoid problems that education can prevent.
Frequently asked questions
What is the most powerful anti-inflammatory peptide?
BPC-157 demonstrates the broadest anti-inflammatory effects across multiple tissue types. For gut-specific inflammation, KPV may be more potent. For immune-driven inflammation, thymosin alpha-1 addresses root causes others cannot. The most powerful choice depends on your specific type of inflammation.
How quickly do anti-inflammatory peptides work?
Some users notice improvements within days, particularly with gut inflammation and KPV. Most protocols require 2-4 weeks before significant benefits become apparent. Tissue regeneration effects from TB-500 may take 6-8 weeks. The peptide timeline guide provides specific expectations by condition.
Can I take anti-inflammatory peptides with NSAIDs?
Limited interaction data exists. BPC-157 may help protect against NSAID-induced gut damage, but this does not eliminate all concerns. Theoretically, combining anti-inflammatory peptides with NSAIDs could increase bleeding risk. Consulting a healthcare provider is advisable.
Are inflammation peptides legal?
Research peptides exist in a regulatory gray area in most jurisdictions. They are typically legal to purchase for research purposes but not approved for human therapeutic use. The peptide legality guide covers regulatory considerations in detail.
Do I need a prescription for inflammation peptides?
Research peptides do not require prescriptions. Some compounding pharmacies produce peptides that do require prescriptions. The peptide therapy cost guide compares research and prescription options.
Can peptides cure autoimmune diseases?
No peptide has been proven to cure autoimmune conditions. However, immunomodulatory peptides like thymosin alpha-1 can help rebalance immune function, potentially reducing autoimmune activity. Managing expectations realistically while exploring potential benefits is appropriate.
What happens when I stop taking anti-inflammatory peptides?
This depends on whether underlying causes of inflammation have been addressed. If lifestyle and root causes are managed, benefits may persist. If inflammatory triggers remain, symptoms may gradually return. Some users maintain benefits long-term while others require periodic or ongoing treatment.
Can I take multiple anti-inflammatory peptides together?
Yes, strategic combinations often enhance results. The BPC-157 and TB-500 stacking guide covers one popular combination. Understanding how many peptides to combine helps design effective stacks.
External resources
Peptides as Therapeutic Agents for Inflammatory-Related Diseases - PubMed Central
Discovery of anti-inflammatory physiological peptides that promote tissue repair - Science Advances
For researchers serious about mastering anti-inflammatory peptide protocols, SeekPeptides provides the most comprehensive resource available. Members access evidence-based guides, proven protocols, and a community of thousands who have navigated these exact questions. The detailed protocol libraries and expert guidance help you implement anti-inflammatory strategies with confidence.



