Jan 18, 2026

You lie awake at 2am. Again.
The ceiling looks the same as it did at midnight. Your mind races through tomorrow's tasks, yesterday's mistakes, and anxieties that seem amplified in the dark. You've tried melatonin. You've tried magnesium. You've tried the sleep hygiene rules everyone recommends. Nothing delivers the deep, restorative sleep you remember having years ago.
Poor sleep doesn't just leave you tired. It accelerates aging. It impairs recovery from training. It elevates cortisol, storing fat around your midsection while breaking down muscle tissue. It clouds cognition, dampens mood, and undermines every other health intervention you attempt.
Delta sleep-inducing peptide, known as DSIP, represents a fundamentally different approach to sleep optimization. Rather than sedating you into unconsciousness like prescription sleep medications, DSIP works with your body's natural sleep architecture to promote the deep, restorative phases that actually regenerate tissue and balance hormones.
First isolated in 1974 from the brains of sleeping rabbits, DSIP has since been studied for effects extending far beyond sleep. Stress modulation. Pain relief. Hormonal balance. Cardiovascular support. The peptide appears to function as a broad regulatory molecule affecting multiple physiological systems.
This guide examines everything current research reveals about DSIP benefits. Not marketing claims, but documented effects from clinical studies and established mechanisms of action.
By the end, you'll understand exactly what DSIP can and cannot do, how to use it effectively if you choose to, and what realistic expectations look like.
SeekPeptides has compiled this comprehensive resource from peer-reviewed research, clinical documentation, and established peptide therapy protocols to give you evidence-based guidance on this intriguing compound.
What is DSIP and where does it come from
DSIP stands for delta sleep-inducing peptide. The name comes from its original discovery context, the compound was first isolated from the brains of rabbits during electrically induced delta wave sleep.
Swiss researchers Marcel Monnier and Guido Schoenenberger made the discovery in 1974. They were investigating the neurochemistry of sleep when they found that blood from sleeping rabbits, when transferred to awake rabbits, induced sleep-like EEG patterns. The active compound responsible turned out to be a small peptide.
Structurally, DSIP is remarkably simple. It consists of just nine amino acids in the sequence Trp-Ala-Gly-Gly-Asp-Ala-Ser-Gly-Glu. This makes it one of the smaller bioactive peptides, far shorter than compounds like BPC-157 (15 amino acids) or GHK-Cu (3 amino acids plus copper ion).
The peptide exists naturally in the human body. Researchers have found DSIP in both free and bound forms throughout the brain, particularly concentrated in the hypothalamus, limbic system, and pituitary gland. It also appears in peripheral organs and body fluids, suggesting systemic regulatory functions beyond the central nervous system.
In the pituitary gland, DSIP co-localizes with numerous other signaling molecules including ACTH, MSH, TSH, and melanin-concentrating hormone. This coexistence hints at DSIP's integration into broader hormonal regulatory networks.
Unlike many peptides that require injection to avoid degradation in the digestive system, DSIP demonstrates unusual stability. Research indicates it can cross the blood-brain barrier freely and survive intestinal passage with some retained activity. This unique property sets it apart from most therapeutic peptides and expands potential administration routes.
How DSIP works in your body
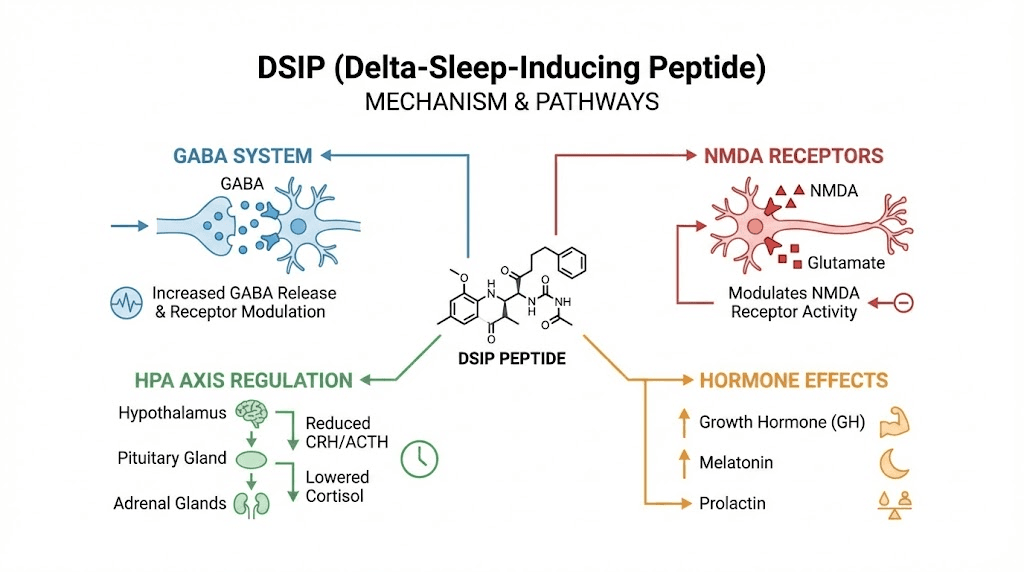
Understanding DSIP's mechanisms helps explain its diverse effects. The peptide appears to work through multiple pathways rather than a single receptor system.
Neurotransmitter modulation
DSIP interacts with two major neurotransmitter systems crucial for sleep and neural balance.
The peptide enhances GABA-activated currents in hippocampal and cerebellar neurons. GABA is your brain's primary inhibitory neurotransmitter, responsible for calming neural activity and promoting relaxation. By potentiating GABA signaling, DSIP supports the neural quieting necessary for sleep onset and maintenance.
Simultaneously, DSIP blocks NMDA-activated responses in cortical areas. NMDA receptors, when overactive, contribute to excitotoxicity and excessive neural firing. By dampening NMDA activity, DSIP reduces the mental hyperarousal that keeps you awake despite physical exhaustion.
This dual action, enhancing inhibitory GABA while reducing excitatory NMDA, creates conditions favorable for transitioning into and maintaining sleep.
Stress axis regulation
DSIP acts as what researchers call a "stress-limiting factor." It modulates the hypothalamic-pituitary-adrenal (HPA) axis, the hormonal cascade responsible for your body's stress response.
Specifically, DSIP decreases basal corticotropin (ACTH) levels and blocks its release under stress. Since ACTH signals the adrenal glands to produce cortisol, reducing ACTH translates to lower cortisol output.
In rat studies, DSIP administration decreased plasma corticosterone (the rodent equivalent of cortisol) by approximately 30%. For humans dealing with chronic stress, this cortisol-lowering effect could have significant implications for sleep quality, body composition, and overall health.
Chronic cortisol elevation interferes with sleep architecture, promotes visceral fat storage, accelerates muscle breakdown, and impairs immune function. By helping normalize cortisol, DSIP may address a root cause of poor sleep rather than merely masking symptoms.
Sleep architecture optimization
DSIP appears to specifically promote delta wave sleep, also called slow-wave sleep or deep sleep. This is the most restorative sleep phase, when your body releases growth hormone, repairs tissue, consolidates memory, and recharges for the next day.
Importantly, research suggests DSIP doesn't simply sedate you. Unlike conventional sleep medications that often suppress REM sleep and leave you groggy, DSIP modulates sleep architecture in ways that enhance quality rather than just quantity.
In one study, subjects immediately reported feeling "sleep pressure" after DSIP administration, and total sleep time increased by 59% within 130 minutes compared to placebo. Other research showed higher sleep efficiency and shorter sleep latency (time to fall asleep) with DSIP.
The peptide's effects appear context-dependent.
Research notes greater activity in circumstances where sleep is already disturbed, with minimal effects in healthy subjects without sleep complaints.
This suggests DSIP functions as a normalizing agent rather than a universal sedative.
Hormonal cascades
Beyond cortisol modulation, DSIP influences several other hormonal systems.
The peptide stimulates release of luteinizing hormone (LH), which in men signals testosterone production and in women supports ovulation and progesterone synthesis. It also stimulates growth hormone-releasing hormone (somatoliberin) and growth hormone itself while inhibiting somatostatin, which normally suppresses GH release.
This hormonal profile suggests DSIP may support anabolic processes, tissue repair, and metabolic health beyond its sleep effects. For individuals interested in testosterone support or muscle growth, DSIP's hormonal effects add additional dimensions of potential benefit.
Documented benefits of DSIP
Research has investigated DSIP for numerous applications. Here's what the evidence actually shows.
Sleep quality improvement
The most extensively studied application. Multiple trials have examined DSIP's effects on both healthy subjects and insomniacs.
A double-blind study in chronic insomniacs found that DSIP improved objective sleep quality metrics including higher sleep efficiency and shorter sleep latency. Subjective reports also showed decreased tiredness compared to placebo.
Research describes DSIP as a "sleep-promoting substance rather than a sedative." This distinction matters because sedatives often produce low-quality sleep that doesn't leave you feeling rested. DSIP appears to enhance the architecture of sleep itself.
One notable property is the delayed effect. DSIP doesn't need to be taken immediately before bed. A dose given during the day can improve sleep that night and for several nights afterward. This differs fundamentally from conventional sleep aids that work acutely and wear off.
Stress and anxiety reduction
DSIP's cortisol-lowering effects translate to measurable stress reduction. By dampening HPA axis activity, the peptide helps break the cycle where stress causes poor sleep which causes more stress.
Animal studies demonstrate reduced behavioral indicators of stress with DSIP administration. The mechanism involves both the direct cortisol reduction and the improved sleep quality that supports stress resilience.
For chronic stress sufferers, this dual action, lowering stress hormones while improving restorative sleep, addresses two interdependent problems simultaneously.
Pain modulation
Research reveals DSIP has analgesic properties. Studies in mice found potent antinociceptive (pain-reducing) effects when the peptide was administered directly to the central nervous system.
Interestingly, DSIP doesn't bind directly to opioid receptors like morphine or endorphins. Instead, it appears to work indirectly by stimulating release of met-enkephalin, one of the body's natural opioid peptides. This mechanism may provide pain relief without the tolerance and dependence issues associated with direct opioid receptor agonists.
For individuals dealing with chronic pain that interferes with sleep, DSIP's combined analgesic and sleep-promoting effects could be particularly relevant. Pain disrupts sleep, and poor sleep amplifies pain perception, creating a vicious cycle that DSIP may help break.
Substance dependence support
One of the more surprising research findings involves DSIP's effects on addiction. The peptide appears to act antagonistically on opiate receptors, significantly inhibiting the development of both opioid and alcohol dependence in animal studies.
Clinical reports suggest broader applications.
In one trial, DSIP administration alleviated withdrawal symptoms in 97% of opiate-dependent and 87% of alcohol-dependent patients. While these results require replication, they suggest DSIP may support recovery from substance dependence.
The mechanism likely involves both the opiate receptor effects and DSIP's normalization of stress hormones, which become dysregulated during addiction and withdrawal.
Cardiovascular effects
Research indicates DSIP can normalize blood pressure and myocardial (heart muscle) contraction. These cardiovascular benefits may relate to the peptide's stress-reducing effects, since chronic stress contributes to hypertension and cardiac dysfunction.
The specific mechanisms remain under investigation, but the finding adds another dimension to DSIP's systemic regulatory effects.
Neuroprotection and stroke recovery
Emerging research suggests DSIP may have neuroprotective properties. In rat models, the peptide accelerated recovery of motor function after focal stroke.
This finding aligns with DSIP's NMDA-blocking activity.
Excessive NMDA activation contributes to excitotoxicity during and after stroke, making NMDA modulation a potential therapeutic target.
By dampening this pathway while supporting restorative processes, DSIP may help protect and repair neural tissue.
Antioxidant activity
Studies show DSIP enhances the efficiency of oxidative phosphorylation in rat mitochondria. This suggests the peptide may support cellular energy production while reducing oxidative stress.
Mitochondrial dysfunction contributes to aging and numerous diseases. Any compound that supports mitochondrial efficiency has implications for longevity and metabolic health.
Anticonvulsant effects
In studies on rats with drug-induced epilepsy, DSIP acted as an anticonvulsant, significantly decreasing both the incidence and duration of seizures.
This effect likely relates to the peptide's GABAergic and anti-NMDA activities.
DSIP dosing protocols
Establishing optimal DSIP dosing requires understanding that human research is limited compared to many other peptides. The protocols below represent current best practices synthesized from available studies and clinical experience.
Conservative starting protocol
For those new to DSIP or peptide therapy generally.
Dose: 50-100mcg
Frequency: 1-2 times per week initially
Timing: 1-3 hours before intended bedtime
Duration: 2-4 week assessment period
This cautious approach allows you to gauge individual response before committing to more aggressive protocols. Some users respond well to very low doses, while others require more to notice effects.
Standard sleep protocol
The most commonly recommended approach for sleep optimization.
Dose: 100-250mcg
Frequency: Daily or every other day
Timing: 30-60 minutes before bed
Duration: 4-8 weeks, followed by 2-4 week break
At these doses, most users report noticeable improvements in sleep onset, depth, and morning alertness. The daily frequency maintains consistent peptide levels while the cycling prevents potential tolerance.
Intensive stress/recovery protocol
For periods of high stress, poor sleep, or recovery from illness/injury.
Dose: 250-300mcg
Frequency: Daily
Timing: 30-60 minutes before bed
Duration: 4 weeks maximum, then mandatory break
Higher doses may provide stronger stress-modulating and recovery effects. However, intensity should be balanced against the limited long-term safety data.
Dr. William Seeds protocol
From the peptide reference text "Peptide Protocols, Volume 1":
Dose: 100mcg subcutaneously
Timing: Approximately 3 hours before bedtime
Frequency: Can be done daily, every 3 days, or weekly depending on response
This flexible approach allows individualization based on how you respond. Some people need consistent dosing; others do well with periodic use.
Titration schedule
For systematic dose finding.
Week 1: 50mcg nightly
Week 2: 100mcg nightly (if Week 1 tolerated well)
Weeks 3-4: 150mcg nightly (if no adverse effects)
Weeks 5-8: 200-300mcg nightly (target maintenance dose)
Gradual titration helps identify your minimum effective dose while avoiding unnecessary exposure to higher amounts.
Protocol comparison table
Protocol | Dose | Frequency | Duration | Best for |
|---|---|---|---|---|
Conservative | 50-100mcg | 1-2x/week | 2-4 weeks | Beginners, assessment |
Standard | 100-250mcg | Daily/EOD | 4-8 weeks | Most users |
Intensive | 250-300mcg | Daily | 4 weeks max | High stress, recovery |
Seeds | 100mcg | Flexible | As needed | Periodic use |
Use the peptide calculator to determine exact syringe volumes based on your reconstitution concentration.
DSIP reconstitution and storage
Proper handling ensures your peptide remains potent throughout its use period.
What you need
Alcohol swabs
Insulin syringes (0.3mL or 0.5mL, 29-31 gauge)
DSIP vial (typically 2mg, 5mg, or 10mg)
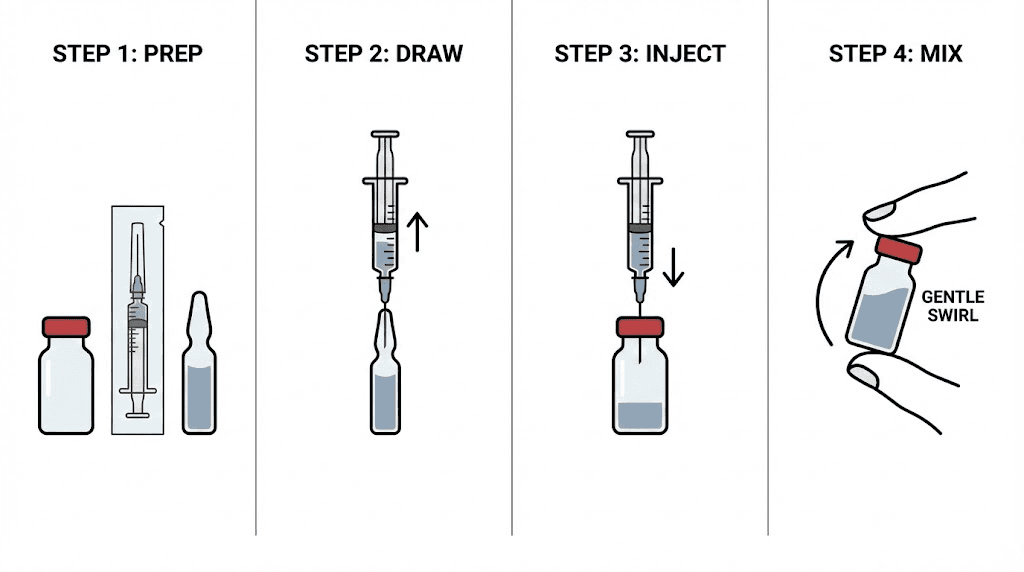
Reconstitution steps
For a 5mg vial:
Add 2.5mL bacteriostatic water to create a concentration of 2mg/mL (2000mcg/mL).
At this concentration:
100mcg = 0.05mL = 5 units on insulin syringe
200mcg = 0.10mL = 10 units
250mcg = 0.125mL = 12.5 units
Alternative concentration:
Add 1mL water to 5mg vial for 5mg/mL (5000mcg/mL).
100mcg = 0.02mL = 2 units
250mcg = 0.05mL = 5 units
The second concentration requires smaller volumes but makes precise measurement more difficult. Choose based on your syringe precision and dose requirements.
Reconstitution technique
Clean both vial stoppers with alcohol swabs
Draw bacteriostatic water into syringe
Insert needle through DSIP vial stopper
Inject water slowly down the vial wall (never directly at the powder)
Allow peptide to dissolve naturally (5-10 minutes)
Swirl gently if needed; never shake vigorously
Solution should become clear
Storage requirements
Before reconstitution:
Store at -20°C (-4°F) for long-term stability
Refrigeration at 2-8°C acceptable for shorter periods
Protect from light
After reconstitution:
Refrigerate at 2-8°C (36-46°F)
Never freeze reconstituted peptide
Use within 4 weeks for optimal potency
Protect from light
Review our complete peptide storage guide for detailed shelf life information.
Administration technique
DSIP is typically administered subcutaneously, though other routes have been studied.
Subcutaneous injection
The standard method. Inject into fatty tissue using a fine-gauge insulin needle.
Preferred sites:
Abdomen (avoid 2 inches around navel)
Front or outer thigh
Upper arm (posterior)
Technique:
Clean injection site with alcohol swab
Let alcohol dry completely
Pinch fold of skin
Insert needle at 45-90 degree angle
Inject slowly over 5-10 seconds
Release skin, withdraw needle
Light pressure if any bleeding
Rotate sites to prevent tissue irritation. Never use the same exact spot on consecutive days.
Timing considerations
Most protocols recommend evening administration, 30-60 minutes before intended sleep. However, DSIP's effects are not strictly acute.
Research shows that a dose given during the day still improves sleep that night and potentially subsequent nights. If evening dosing causes any issues (some users report vivid dreams when taking DSIP too close to bedtime), experimenting with afternoon administration is reasonable.
The key is consistency. Whatever timing you choose, maintain it throughout your protocol to establish stable effects.
Nasal administration
Some research and commercial products explore nasal DSIP delivery. The peptide's ability to cross the blood-brain barrier and its stability may make this route viable.
However, most established protocols use subcutaneous injection. If considering nasal administration, recognize that absorption and dosing precision may differ from injection.
Results timeline: what to expect
Understanding realistic timelines prevents premature conclusions about DSIP's effectiveness.
First dose to first week
Some users notice effects from the very first dose. Research shows subjects reporting "sleep pressure" within about 2 hours of administration, with sleep time increasing significantly that same night.
Others experience more gradual onset. Don't conclude DSIP isn't working if effects aren't dramatic immediately. The peptide often requires several days to a week of consistent use before benefits become obvious.
During this initial period, you might notice:
Easier time falling asleep
Feeling of calm or reduced anxiety
More vivid dreams (a common early effect)
Slightly deeper sleep (even if not dramatic yet)
Weeks 2-4
This is when most users experience clearer benefits. Sleep architecture improvements become more established, and the cumulative effect of better rest manifests in daytime function.
Common reports include:
Waking fewer times during the night
Feeling more refreshed upon waking
Improved daytime energy and mood
Reduced stress reactivity
Better recovery from exercise
The stress-modulating effects often become noticeable during this window as cortisol patterns normalize.
Weeks 4-8
Full benefits typically manifest by week 4-6 of consistent use. Sleep quality improvements plateau at their maximum, and systemic effects from better rest and lower stress become apparent.
Users often report:
Significantly improved sleep consistency
Notable mood improvements
Better stress tolerance
Enhanced cognitive function
Improved body composition (from normalized cortisol)
Factors affecting response
Baseline sleep quality: Those with significantly disrupted sleep tend to notice more dramatic improvements. People with already decent sleep may experience subtler effects.
Stress levels: High-stress individuals often respond well to DSIP's cortisol-modulating effects. Lower-stress individuals may benefit more from the direct sleep-promoting mechanisms.
Age: Older adults, who naturally produce less DSIP, may be particularly responsive to supplementation.
Dose consistency: Irregular dosing produces irregular results. Consistent administration allows proper assessment.
Side effects and safety considerations
DSIP demonstrates a favorable safety profile in available research, but important considerations exist.
Reported side effects
Most commonly documented effects are mild and transient.
Daytime drowsiness: Some users experience grogginess if dosing is too high or poorly timed. Adjusting dose or administration time usually resolves this.
Headaches: Occasionally reported, particularly during initial use. Usually mild and diminishing with continued use.
Vivid dreams: A common effect related to DSIP's influence on sleep architecture. Some users find this pleasant; others find it disruptive initially.
Injection site reactions: Mild redness or irritation possible, as with any injection. Proper technique and site rotation minimize this.
Hormonal fluctuations: Given DSIP's effects on LH and GH, some hormonal variability is possible, though rarely problematic in documented use.
Nausea: Uncommonly reported, usually with higher doses.
FDA safety concerns
The FDA includes DSIP on its list of bulk drug substances with potential safety risks. The primary concern is immunogenicity, the possibility that the body might mount an immune response against the peptide.
It's important to contextualize this concern. The FDA flags many research compounds with limited human safety data.
This doesn't necessarily mean DSIP is dangerous, but it does mean comprehensive safety evaluation hasn't been completed.
Research perspective
A 2001 editorial in the European Journal of Anaesthesiology described DSIP as "incredibly safe" based on the lack of lethal doses in animal studies and absence of significant side effects in human trials beyond transient symptoms.
However, this assessment comes from limited data. Long-term safety with chronic use hasn't been established in rigorous clinical trials.
Contraindications and precautions
Consider avoiding DSIP or consulting a physician if:
Pregnant or breastfeeding (insufficient safety data)
Taking naloxone or other opioid antagonists (may block effects)
Using medications metabolized by peptidases (potential interactions)
History of immune disorders (theoretical immunogenicity concern)
Already using multiple sleep medications
Drug interactions
Because DSIP degrades via amino-peptidases in blood, medications affecting these enzymes (like the ACE inhibitor captopril) could theoretically alter DSIP metabolism. Clinical significance is unknown, but caution is reasonable.
Combining DSIP with other sleep medications isn't well-studied. If you're currently using prescription sleep aids, discuss any changes with your prescriber.
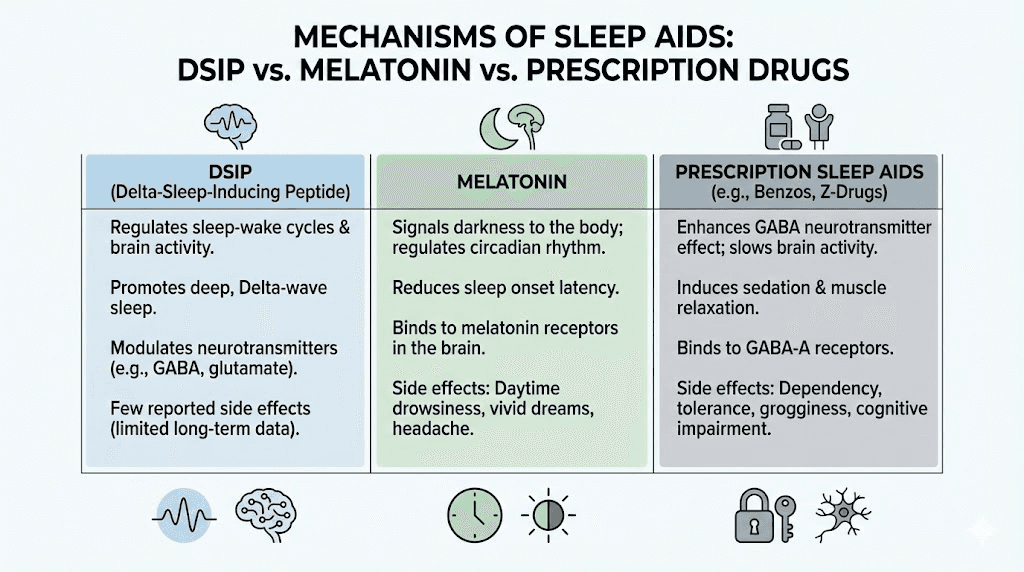
DSIP compared to other sleep solutions
Understanding how DSIP differs from alternatives helps inform appropriate use.
DSIP vs melatonin
Melatonin regulates sleep timing by signaling to your body that it's time to sleep. It's most useful for circadian rhythm issues, jet lag, or getting your body clock synchronized.
DSIP appears to affect sleep depth and quality rather than timing. It promotes delta wave sleep and modulates stress hormones.
They work through different mechanisms and may be complementary. Someone with both timing and quality issues might benefit from both: melatonin to get the clock set, DSIP to deepen the sleep itself.
DSIP vs prescription sleep medications
Benzodiazepines and Z-drugs (like Ambien) work by potentiating GABA receptors, producing sedation. They're effective at inducing sleep but often suppress beneficial sleep stages and can cause dependence.
DSIP also has GABAergic activity but appears to modulate sleep architecture rather than simply sedating. Research suggests it promotes natural sleep patterns rather than chemically overriding them.
For chronic sleep issues, DSIP's approach of normalizing sleep may be more sustainable than sedatives that mask symptoms without addressing underlying dysfunction.
DSIP vs other sleep peptides
Other peptides affect sleep through various mechanisms.
Sermorelin and growth hormone secretagogues can improve sleep quality indirectly by boosting GH release, which naturally occurs during deep sleep.
Epitalon affects the pineal gland and may support melatonin production and circadian function.
DSIP stands out for its direct effects on sleep architecture and its unique combination of sleep-promoting and stress-modulating properties.
DSIP vs supplements
Common sleep supplements like magnesium, L-theanine, and glycine support sleep through various mechanisms. They're generally safe and can be helpful.
DSIP offers more targeted effects on specific sleep and stress pathways. For someone who hasn't responded adequately to supplements, DSIP represents a more potent intervention.
Stacking DSIP with other compounds
Some users incorporate DSIP into broader peptide or supplement stacks.
Compatible combinations
Melatonin: Can be used together. Melatonin for timing, DSIP for depth. Start with low doses of both when combining.
Magnesium: Supports GABA function and muscle relaxation. Complementary mechanism without concerning interactions.
GH secretagogues: Compounds like CJC-1295 or ipamorelin are often taken before bed to capitalize on natural GH release during sleep. DSIP's enhancement of deep sleep could synergize with GH secretagogue effects.
Energy-supporting peptides: Compounds used for daytime energy don't conflict with DSIP's nighttime effects.
Potentially redundant combinations
Multiple high-dose sedating compounds together could cause excessive drowsiness. If combining DSIP with other sleep-promoting substances, use lower doses of each and assess carefully.
Approach to stacking
Start DSIP alone to understand your individual response before adding other compounds. This allows you to identify what's working and troubleshoot any issues without confounding variables.
SeekPeptides members get access to detailed stacking protocols and guidance for combining multiple peptides safely.
Who should consider DSIP
DSIP may be appropriate for certain profiles while less suitable for others.
Potentially good candidates
Chronic poor sleepers: Those who've struggled with sleep quality despite trying conventional approaches. DSIP offers a different mechanism than typical interventions.
High-stress individuals: The cortisol-modulating effects address a common underlying cause of poor sleep. If stress is clearly affecting your rest, DSIP may help on multiple levels.
Athletes and recovery-focused individuals: Deep sleep is crucial for physical recovery. DSIP's promotion of delta wave sleep supports tissue repair and GH release.
Those with pain-related sleep issues: DSIP's analgesic properties combined with sleep enhancement could break the pain-sleep disruption cycle.
Aging individuals: Natural DSIP levels decline with age. Supplementation may restore youthful sleep architecture more effectively in this population.
Less suitable candidates
Those requiring immediate results: While some notice first-dose effects, DSIP works best with consistent use over weeks.
People satisfied with current sleep aids: If your current approach works well, no compelling reason to switch.
Those unable to inject: While other routes exist, subcutaneous injection remains the standard and most reliable method.
Individuals with significant contraindications: Pregnancy, certain medications, immune issues, etc.
Frequently asked questions
How quickly does DSIP work for sleep?
Effects can begin within hours of the first dose, with research showing sleep pressure reported within about 2 hours. However, optimal benefits typically develop over 2-4 weeks of consistent use. Some users notice immediate improvements; others require patience as effects accumulate. The peptide appears to work by normalizing sleep architecture rather than acutely sedating, which explains the variable onset.
Can I take DSIP every night?
Daily use is common in research protocols, typically for 4-8 week cycles. However, taking periodic breaks (2-4 weeks off after each cycle) may help maintain effectiveness and prevent potential tolerance. Some users prefer every-other-day dosing or even weekly administration with good results. Experiment to find your optimal frequency while respecting cycling recommendations.
What time should I take DSIP?
Most protocols recommend 30-60 minutes before intended sleep. However, DSIP has delayed effects, with some research administering doses hours before bed or even during the day with benefits extending to that night's sleep. If nighttime dosing causes vivid dreams or grogginess, try earlier evening administration. The key is consistency in whatever timing you choose.
Is DSIP addictive?
Available research suggests DSIP doesn't cause dependence. Unlike benzodiazepines or other sedatives, it doesn't appear to create tolerance requiring escalating doses or produce withdrawal symptoms upon cessation.
In fact, DSIP has been studied as a potential treatment for opioid and alcohol dependence.
Standard cycling protocols (4-8 weeks on, 2-4 weeks off) further minimize any theoretical dependence risk.
Can I combine DSIP with melatonin?
Yes, they work through different mechanisms and may be complementary. Melatonin regulates sleep timing while DSIP affects sleep depth and quality. If combining, start with lower doses of each to assess the combination. Many users find melatonin helps with falling asleep while DSIP improves the quality of sleep once achieved. See our guide on combining peptides for more stacking guidance.
Does DSIP affect dreams?
Yes, vivid dreams are commonly reported with DSIP use. The peptide appears to influence sleep stages in ways that alter dream intensity and recall. Some users enjoy this effect; others find it initially disruptive. The phenomenon typically becomes less pronounced with continued use. Adjusting timing (taking DSIP earlier in the evening) may also moderate dream effects.
Is DSIP legal?
DSIP is not FDA-approved for human therapeutic use in the United States and is typically sold as a research peptide. Possession and personal use are generally not regulated, but sale for human consumption is not permitted. Legal status varies by country. DSIP is not included on WADA's prohibited list for athletes, unlike some other peptides.
How do I know if DSIP is working?
Signs of effective DSIP use include: easier time falling asleep, fewer nighttime awakenings, feeling more refreshed upon waking, improved daytime energy and mood, better stress tolerance, and enhanced recovery from physical activity. Track these metrics for several weeks to assess response accurately. Some users don't notice dramatic changes but find their baseline sleep quality has improved when they look back objectively.
External resources
For researchers serious about optimizing their sleep and recovery, SeekPeptides offers the best resource available, with evidence-based guides, proven protocols, and a community of thousands who've navigated these exact questions.