Jan 23, 2026
Your body knows how to heal. It has been doing it since you were born, knitting together cuts, rebuilding torn fibers, regenerating damaged cells. But sometimes healing takes too long. Sometimes the repair process stalls. Sometimes you need more than your body can naturally provide.
This is where tissue repair peptides enter the picture.
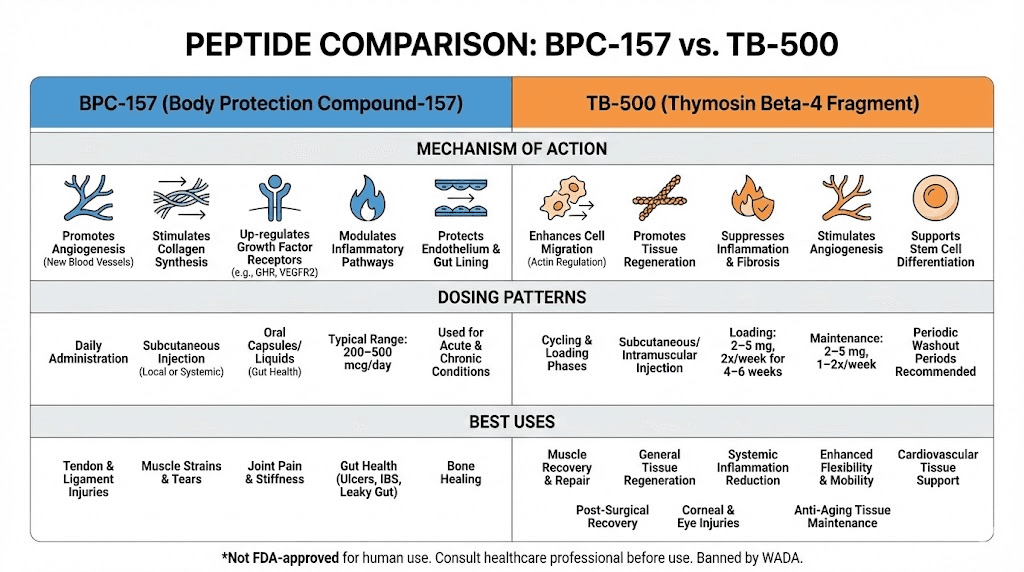
These short chains of amino acids act as signaling molecules that accelerate the healing cascade. They tell your cells to divide faster, migrate to injury sites quicker, and produce collagen more efficiently. BPC-157, TB-500, GHK-Cu, and other healing peptides have become essential tools for researchers exploring accelerated recovery from tendon tears, muscle strains, ligament damage, and chronic wounds.
The science behind these compounds is compelling. Studies show BPC-157 can increase growth hormone receptor expression in tendon fibroblasts by sevenfold within three days. TB-500 enhances cell migration to damaged areas by binding to actin and promoting cellular movement. GHK-Cu has demonstrated the ability to increase collagen production by up to 70% in laboratory studies. These are not subtle effects. These are measurable, documented changes in tissue repair speed and quality.
But here is what makes peptide therapy for tissue repair genuinely valuable. It is not just about speeding up the timeline. It is about improving the quality of repair. Faster healing means nothing if the tissue comes back weaker. Research suggests that certain peptides may actually improve the structural integrity of regenerated tissue, not just the speed at which it forms. That distinction matters enormously for anyone dealing with recurring injuries or chronic healing problems.
SeekPeptides has compiled the most comprehensive guide available on tissue repair peptides. You will learn which peptides work best for specific injury types, how to dose them properly, what stacking combinations researchers use, and what realistic timelines to expect. Whether you are researching recovery from a torn tendon, a muscle strain, or a chronic wound that refuses to close, this guide covers the science and application of every major healing peptide.
The information ahead is detailed. It is evidence-based. And it will fundamentally change how you understand the body's capacity for repair.
Understanding the science of tissue repair
Before examining specific peptides, you need to understand what happens when tissue gets damaged and how repair actually works at the cellular level. This foundation makes everything that follows more practical and applicable.
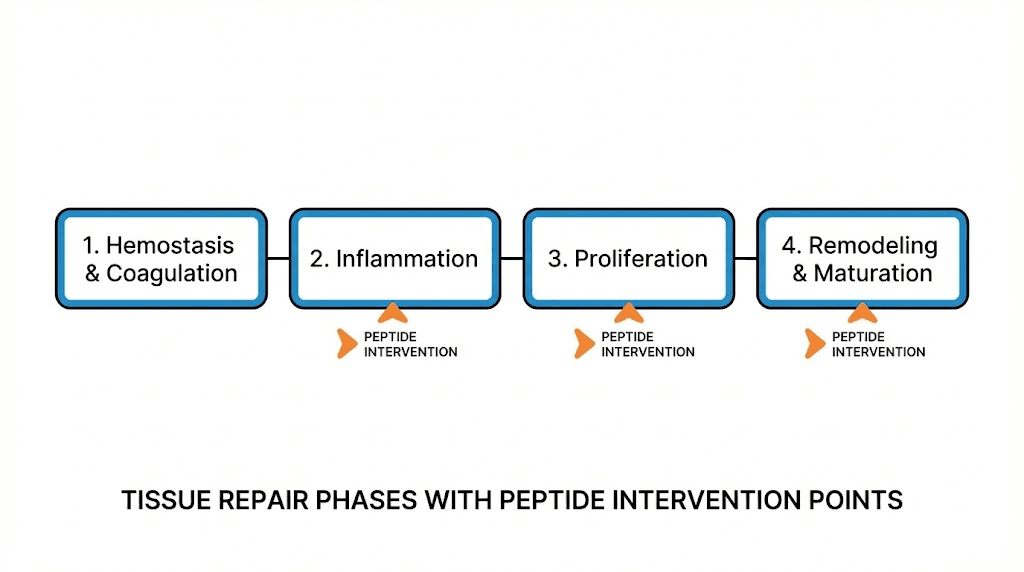
Tissue repair occurs in four overlapping phases. Hemostasis happens first, stopping bleeding through clot formation and platelet activation. Inflammation follows immediately, bringing immune cells to clear debris and fight infection. The proliferation phase comes next, where new tissue actually forms through cell division and matrix deposition. Finally, remodeling restructures and strengthens the new tissue over weeks to months.
Each phase presents opportunities for peptide intervention. Some peptides work primarily in the inflammatory phase, modulating the immune response to prevent excessive damage. Others shine during proliferation, accelerating cell division and migration. Still others improve remodeling, ensuring the new tissue has proper structure and strength.
Why natural healing sometimes fails
Your body has remarkable healing capacity. But several factors can slow or impair the repair process.
Age plays a significant role. The natural peptide GHK-Cu, which promotes tissue regeneration, exists at approximately 200ng/mL in serum at age 20. By age 60, that level drops to 80ng/mL. This decline correlates with reduced regenerative capacity across multiple tissue types. Older individuals simply have less of the signaling molecules that drive efficient repair.
Blood supply matters enormously. Tendons and ligaments have notoriously poor vascularization compared to muscles. This means fewer nutrients reaching the injury site, slower removal of waste products, and reduced delivery of growth factors. Peptides that promote angiogenesis, the formation of new blood vessels, can address this limitation directly.
Chronic inflammation creates another obstacle. While acute inflammation is necessary for healing, prolonged inflammatory states actively degrade tissue faster than it can form. People with autoimmune conditions, metabolic disorders, or persistent infections often experience this problem. Anti-inflammatory peptides can break this cycle, allowing the proliferative phase to proceed normally.
Nutritional deficiencies matter too. Collagen synthesis requires adequate protein, vitamin C, copper, and zinc. Growth factor production needs sufficient calories and amino acids. Even the best peptide protocol will underperform if basic nutritional building blocks are missing.
How tissue repair peptides work
Peptides are short chains of amino acids, typically between 2 and 50 amino acids in length. They function as signaling molecules, binding to receptors on cell surfaces and triggering specific biological responses. This is different from simply providing building materials. Peptides tell your cells what to do. They upregulate genes involved in repair. They recruit immune cells and fibroblasts to injury sites. They modulate inflammation and promote angiogenesis.
The key mechanisms through which tissue repair peptides operate include:
Growth factor modulation: Many peptides increase the expression or activity of growth factors like IGF-1, VEGF, TGF-beta, and FGF. These growth factors drive cell proliferation, migration, and differentiation. BPC-157, for example, increases growth hormone receptor expression in tendon fibroblasts, amplifying the tissue response to circulating growth hormone.
Angiogenesis promotion: New blood vessel formation is critical for delivering nutrients and oxygen to healing tissue. Peptides like BPC-157 and TB-500 promote angiogenesis through multiple pathways, including VEGF upregulation and direct effects on endothelial cell migration.
Collagen synthesis enhancement: Collagen provides structural support to virtually all connective tissues. GHK-Cu directly stimulates collagen production while also modulating the enzymes that break down and reorganize collagen during remodeling. This dual action improves both the quantity and quality of new tissue.
Inflammation modulation: Controlled inflammation is necessary, but excessive inflammation impairs healing. Peptides like KPV block inflammatory pathways without completely suppressing the immune response, allowing healing to proceed while preventing tissue damage from prolonged inflammation.
Cell migration enhancement: Getting cells to the injury site is half the battle. TB-500 binds to actin, the protein that forms the cellular skeleton, and promotes the movement of fibroblasts, endothelial cells, and other repair cells to damaged areas.
BPC-157: the body protection compound
BPC-157, or Body Protection Compound-157, has become the most researched and widely used tissue repair peptide. This 15-amino acid sequence derived from human gastric juice demonstrates healing effects across virtually every tissue type studied.
The peptide was first isolated from protective proteins in the stomach lining. Researchers noted that despite constant exposure to harsh stomach acid, the gastric mucosa heals remarkably quickly from damage. They identified BPC-157 as a key factor in this rapid repair capability and began testing it on other tissue types.
Mechanisms of BPC-157
BPC-157 works through multiple interconnected pathways, which partly explains its broad effectiveness.
The peptide significantly enhances ERK1/2 phosphorylation in endothelial cells, leading to increased cellular proliferation, migration, and vascular tube formation. These effects are mediated through downstream activation of transcription factors including c-Fos, c-Jun, and EGR-1, which regulate genes involved in cell cycle progression and extracellular matrix remodeling.
Growth hormone receptor upregulation represents another major mechanism. A 2019 study using cDNA microarray analysis revealed that growth hormone receptor was one of the most abundantly upregulated genes in tendon fibroblasts treated with BPC-157. The peptide increased GH receptor expression in a dose and time-dependent manner at both mRNA and protein levels. This amplifies your tissue response to circulating growth hormone, potentially explaining the dramatic effects seen in tendon and muscle healing.
BPC-157 also interacts with the nitric oxide system, promoting vasodilation and blood flow to injured areas. It has been shown to counteract the negative effects of NSAIDs on healing, which is significant given how often these drugs are used for pain management during recovery.
The peptide demonstrates cytoprotective effects, protecting cells from oxidative stress and other damaging conditions. It modulates inflammatory cytokine production, reducing excessive inflammation without completely suppressing the immune response needed for healing.
BPC-157 for different tissue types
Tendon repair: This is arguably where BPC-157 shines brightest. Studies show it accelerates the healing of transected tendons, improves tensile strength of repaired tendons, and promotes better structural organization of collagen fibers. The sevenfold increase in growth hormone receptor expression within three days suggests why tendon repair responds so dramatically to this peptide.
Muscle healing: BPC-157 has demonstrated benefits for both acute muscle injuries and chronic muscle diseases. It promotes satellite cell activation, accelerates muscle fiber regeneration, and reduces fibrosis that can impair function after healing. If you are researching recovery from muscle strains or tears, BPC-157 deserves serious consideration.
Ligament repair: Similar to tendons, ligaments benefit from BPC-157's collagen-enhancing and angiogenic effects. The peptide has shown promise for both acute ligament injuries and chronic ligament laxity, though more research is needed on long-term structural outcomes.
Gut healing: Given its origins in the stomach, BPC-157 predictably excels at healing the gastrointestinal tract. It has shown benefits for inflammatory bowel disease, ulcers, and leaky gut in animal models. The peptide protects and repairs the gut lining while also modulating the microbiome-immune system interface.
Skin wounds: BPC-157 accelerates wound closure, improves collagen deposition, and enhances blood vessel formation in healing skin. It has potential applications for both acute wounds and chronic non-healing ulcers, though clinical data in humans remains limited.
BPC-157 dosing protocols
Research protocols typically use BPC-157 in the range of 200-500mcg per day, often split into twice-daily doses.
Using 100-150mcg is generally considered below the minimum effective threshold for significant tissue repair effects. Most researchers start with 250mcg minimum and increase to 500mcg for more serious injuries.
Administration routes include subcutaneous injection near the injury site, intramuscular injection, and oral administration. Subcutaneous injection near the injury appears to produce the most localized effects, though systemic benefits have been observed with all routes. Use the peptide reconstitution calculator to determine proper mixing ratios.
A common protocol mistake is stopping BPC-157 when pain subsides, usually around weeks 2-3. However, tissue is still healing internally at this point. Stopping early leads to incomplete repair and increased re-injury risk. Most protocols recommend a minimum of 6-8 weeks, continuing even when symptoms have resolved.
For chronic or severe injuries, some researchers extend protocols to 12 weeks or longer. There is limited data on potential diminishing returns with extended use, so monitoring response and adjusting accordingly is prudent.
TB-500: thymosin beta-4 for systemic healing
TB-500 refers to a synthetic fragment of Thymosin Beta-4, a naturally occurring 43-amino acid protein found in nearly all cell types and body fluids. Particularly high concentrations exist in platelets and wound fluid, suggesting an important role in natural healing processes.
Unlike BPC-157, which tends to work more locally around the injection site, TB-500 has pronounced systemic effects. This means it can promote healing throughout the body regardless of where it is administered. For researchers dealing with multiple injury sites or systemic healing impairment, this characteristic makes TB-500 particularly valuable.
Mechanisms of TB-500
The primary mechanism of TB-500 involves binding to actin, a key component of the cellular skeleton. This interaction promotes cell migration, allowing fibroblasts, endothelial cells, and other repair cells to move more efficiently toward damaged tissue.
Research published in The FASEB Journal identified a novel mechanism where Thymosin Beta-4 binds to F1-F0 ATP synthase with a binding affinity of 12 nanomolar. This interaction increases cell surface ATP levels, which then activates P2X4 purinergic receptors. The pathway drives endothelial cell migration during wound repair, providing a mechanistic explanation for TB-500's angiogenic effects.
TB-500 also modulates inflammation through effects on microRNA expression. Research has observed that TB-500 may increase the expression of microRNA-146a, which negatively regulates pro-inflammatory signaling pathways. This results in decreased expression of IRAK1 and TRAF6, two molecules involved in inflammatory cytokine production.
The peptide promotes hair follicle stem cell migration, has demonstrated cardioprotective effects, and appears to enhance blood vessel formation through multiple mechanisms beyond simple VEGF upregulation.
TB-500 for different tissue types
Muscle repair: TB-500 excels at muscle healing, promoting satellite cell activation and migration to damaged fibers. Its systemic action means it can support repair of both the primary injury and any compensatory strain on surrounding muscles. Research in muscle growth and repair consistently highlights TB-500 as a primary healing peptide.
Tendon and ligament healing: While BPC-157 may have more direct effects on tendon fibroblasts, TB-500 contributes through enhanced cell migration and blood vessel formation. The combination of both peptides often produces better outcomes than either alone for connective tissue injuries.
Cardiac repair: TB-500 has shown particular promise for heart tissue, reducing infarct size and improving function after ischemic damage in animal models. This application remains experimental but suggests broad regenerative potential.
Skin healing: Enhanced cell migration translates to faster wound closure, while improved blood vessel formation supports better tissue nutrition during repair. TB-500 has shown benefits for both acute wounds and chronic healing problems.
Hair regeneration: The peptide's effects on hair follicle stem cells have generated interest for hair loss applications, though this is secondary to its primary tissue repair uses.
TB-500 dosing protocols
TB-500 protocols typically use higher absolute doses than BPC-157, reflecting its different pharmacokinetics and systemic distribution.
A common approach involves a loading phase of 4-8mg per week for the first 4-6 weeks, followed by a maintenance dose of 2-4mg per week for another 4-6 weeks. The loading phase saturates tissue levels, while maintenance sustains the healing environment.
Unlike BPC-157, TB-500 does not require injection near the injury site. Its systemic action means subcutaneous injection anywhere convenient will produce similar effects throughout the body. This makes TB-500 particularly practical for researchers dealing with multiple injury locations.
The half-life of TB-500 is relatively long compared to BPC-157, allowing less frequent dosing. Many protocols use twice-weekly injections rather than daily administration.
GHK-Cu: the copper peptide for regeneration
GHK-Cu, glycyl-L-histidyl-L-lysine copper, is a naturally occurring tripeptide that declines significantly with age. Present in human plasma, saliva, and urine, this peptide plays crucial roles in wound healing, skin repair, and tissue regeneration.
The copper component is essential for GHK's activity. Copper ions participate in numerous enzymatic reactions involved in collagen synthesis, elastin production, and antioxidant defense. The peptide effectively delivers copper to cells in a biologically active form while also triggering signaling cascades independent of its metal content.
Mechanisms of GHK-Cu
GHK-Cu stimulates collagen synthesis through multiple pathways. Research shows the peptide increases Type I collagen, which provides structural support, and Type III collagen, which is essential for tissue flexibility and repair. Studies have documented collagen increases of up to 70% in laboratory studies, with human trials showing improvements in 70% of volunteers when compared to vitamin C and retinoic acid.
The peptide also modulates metalloproteinases and their inhibitors, the enzymes that break down and reorganize extracellular matrix. This dual action on both synthesis and breakdown allows for more organized collagen deposition rather than chaotic scar formation.
GHK-Cu demonstrates remarkable effects on gene expression. Studies using the Broad Institute Connectivity Map found that GHK significantly increased the expression of DNA repair genes, with 47 genes stimulated and 5 suppressed. The peptide appears capable of resetting the gene expression profile of aged cells to patterns more similar to younger cells, potentially explaining its broad regenerative benefits.
Blood vessel and nerve outgrowth are also enhanced by GHK-Cu. This improved vascularization and innervation supports better tissue nutrition and function during repair, contributing to more complete healing outcomes.
GHK-Cu for different tissue types
Skin healing: This is where GHK-Cu has the most documented benefits. The peptide accelerates wound closure, improves collagen deposition, and enhances overall skin quality. Studies have documented healing time reductions of 30-50% when GHK-Cu is applied to various wound types. Wound closure rates reached 96% by Day 11 with GHK-silver nanoparticle formulations, showing improved tissue regeneration, increased epidermal thickness, and reduced TNF-alpha expression.
Hair regeneration: GHK-Cu promotes hair follicle stem cell activity and may extend the growth phase of hair follicles. While not primarily a hair loss treatment, these effects make it useful as part of comprehensive hair health protocols.
Connective tissue repair: Though less studied than BPC-157 or TB-500 for tendons and ligaments, GHK-Cu's collagen-enhancing effects translate to benefits for these tissues as well. The peptide has been incorporated into surgical grafts to improve healing outcomes.
Anti-aging and skin quality: Beyond acute wound healing, GHK-Cu improves skin firmness by 20-30% after 12 weeks of topical treatment in clinical studies. Wrinkle reduction of over 55% compared to control has been documented, making it popular for aesthetic applications alongside tissue repair uses.
GHK-Cu dosing protocols
GHK-Cu administration varies significantly based on the target tissue and formulation.
For injectable protocols, typical doses range from 1-5mg administered subcutaneously once daily or every other day. Higher doses around 5mg are often used for acute injury healing, while lower doses support general tissue health and regeneration.
Topical GHK-Cu is available in various concentrations for skin applications. Effective serums typically contain 0.5-2% GHK-Cu. These can be applied 1-2 times daily to the face or specific wound sites. See our guide on copper peptide concentrations for more detail.
When using injectable GHK-Cu for tissue repair, many researchers combine it with BPC-157 or TB-500 to address different aspects of the healing process simultaneously. GHK-Cu provides the collagen-enhancing and gene-modulating effects while the other peptides handle cell migration, growth factor modulation, and angiogenesis.
The peptide can also be used in microneedling protocols, where tiny punctures in the skin allow deeper penetration of topically applied GHK-Cu. This approach is particularly popular for facial rejuvenation but can be applied to scar revision and chronic wound treatment as well.
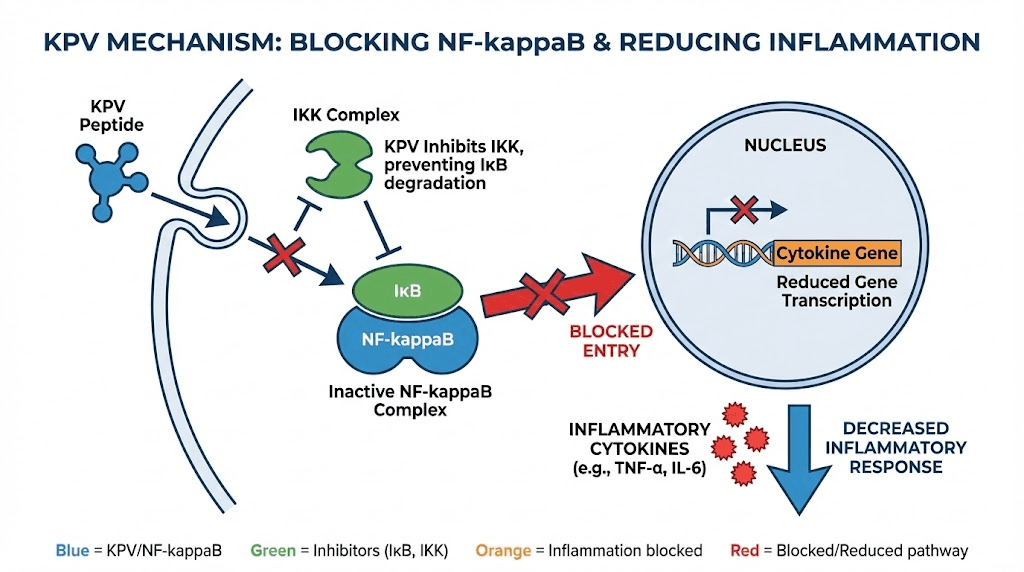
KPV: the anti-inflammatory healing peptide
KPV (lysine-proline-valine) is an ultra-short tripeptide derived from alpha-melanocyte stimulating hormone. Despite consisting of just three amino acids, KPV retains powerful anti-inflammatory properties from its parent hormone while eliminating effects like pigmentation changes.
This peptide addresses a specific limitation in tissue repair: excessive inflammation. While acute inflammation is necessary for healing, chronic or prolonged inflammation actively degrades tissue faster than it can form. KPV breaks this cycle by targeting inflammatory pathways without suppressing immune function entirely.
Mechanisms of KPV
KPV works primarily by blocking the NF-kappaB inflammatory pathway. This master regulator controls the expression of numerous pro-inflammatory genes. By inhibiting NF-kappaB, KPV reduces production of inflammatory cytokines like TNF-alpha and IL-6 that would otherwise impair tissue repair.
Interestingly, KPV's anti-inflammatory effect is not melanocortin receptor-mediated like its parent hormone. Instead, it works through PepT1, a transporter normally expressed in the small intestine and induced in the colon during inflammatory bowel disease. This unique mechanism allows KPV to exert anti-inflammatory effects without activating melanocortin pathways.
Research demonstrates that orally delivered KPV decreases the severity of chemically-induced colitis in mice. The peptide was found to exert an even stronger anti-inflammatory effect than full-length alpha-MSH while being able to attenuate inflammatory responses in both epithelial and immune cells.
KPV also exhibits antimicrobial properties, effectively combating pathogens like S. aureus and C. albicans. This dual anti-inflammatory and antimicrobial action makes it particularly valuable for healing wounds that may be complicated by infection.
KPV for different tissue types
Gut healing: This is KPV's primary application. The peptide reduces inflammation in intestinal cells, preserves the gut lining, and helps restore microbiome balance. Hyaluronic acid-functionalized nanoparticles loaded with KPV have demonstrated combined effects against ulcerative colitis by both accelerating mucosal healing and alleviating inflammation.
Skin repair: KPV accelerates wound healing in skin while dampening post-trauma inflammation. This makes it useful for inflammatory skin conditions as well as acute wounds. The peptide promotes wound repair by boosting neutrophil antimicrobial activity and tissue regeneration.
Inflammatory conditions: Beyond specific tissue repair, KPV may benefit any healing situation complicated by excessive inflammation. This includes autoimmune-related tissue damage, chronic wounds, and post-surgical inflammation that impairs recovery.
KPV dosing protocols
KPV can be administered through multiple routes depending on the target tissue.
For gut healing, oral administration is commonly used at doses of 500mcg to 1mg daily. The PepT1 transporter mechanism allows effective absorption and action in the intestinal tract. Some formulations use nanoparticle delivery systems to enhance stability and targeting.
Subcutaneous injection is also effective, particularly for systemic anti-inflammatory effects or skin healing. Typical doses range from 200-500mcg daily.
For gut-related conditions, noticeable improvements in digestive symptoms often occur within 2-4 weeks. Measurable changes in inflammatory markers typically appear within 4-6 weeks. Long-term benefits, including sustained inflammation reduction and tissue healing, develop over 8-12 weeks of therapy.
KPV pairs well with BPC-157 for gut healing protocols. BPC-157 provides direct tissue repair effects while KPV addresses the inflammatory component that often perpetuates gut damage.
Other tissue repair peptides
Beyond the primary four peptides discussed above, several others demonstrate tissue repair potential and deserve consideration for specific applications.
MGF (Mechano Growth Factor)
MGF is a splice variant of the IGF-1 gene produced in skeletal muscle tissue in response to mechanical stress or overload. It is expressed as a pulse following muscle damage and appears involved in activating muscle satellite stem cells.
Research suggests that after muscle injury, the IGF-1 gene is first spliced toward the MGF variant. The MGF peptide then activates quiescent satellite cells to enter the cell cycle and develop into myoblasts, promoting proliferation of these precursor cells. At later time points, the IGF-1Ea splice variant takes over, driving differentiation into mature muscle fibers.
PEG-MGF, a pegylated form with longer half-life, has shown promise in animal studies. It has been demonstrated to modulate muscle inflammation, improve recruitment of macrophages and neutrophils to injury sites, accelerate bone regeneration in rabbits, and improve articular cartilage repair.
However, significant scientific controversy exists around MGF. Some researchers have been unable to reproduce the claimed effects of synthetic MGF peptides on myoblast proliferation, with concentrations up to 500ng/mL failing to increase proliferation in C2C12 cells or primary human myoblasts. The full-length IGF-1 molecule produced similar effects to what was attributed to isolated MGF peptide in some studies.
For researchers interested in MGF, the evidence suggests that while the natural splice variant clearly plays a role in muscle repair, the isolated synthetic peptide may not replicate those effects reliably. More cautious approaches might favor peptides with stronger evidence bases.
SS-31 (Elamipretide)
SS-31 is a mitochondria-targeted antioxidant peptide that addresses a specific aspect of tissue repair: oxidative stress. During injury and healing, mitochondrial dysfunction and reactive oxygen species production can impair repair processes and damage newly forming tissue.
The peptide selectively concentrates in mitochondria and inhibits intracellular ROS generation. By protecting mitochondrial function and reducing oxidative stress, SS-31 creates a more favorable environment for tissue regeneration.
Applications include cardiac repair after ischemic injury, skeletal muscle recovery, and potentially any tissue repair situation complicated by mitochondrial dysfunction or excessive oxidative stress. The peptide is particularly relevant for older individuals whose mitochondrial function may already be compromised.
Pentosan Polysulfate
While not technically a peptide, pentosan polysulfate deserves mention as it is often discussed alongside tissue repair peptides. This semi-synthetic polysaccharide has FDA approval for interstitial cystitis and has shown benefits for osteoarthritis and cartilage repair.
The compound works through multiple mechanisms including anti-inflammatory effects, enhanced proteoglycan synthesis, and inhibition of enzymes that degrade cartilage matrix. It is typically administered as intramuscular injections or oral capsules.
Collagen peptides
Collagen peptides represent a different approach to tissue repair. Rather than signaling molecules that modify cell behavior, these are hydrolyzed collagen proteins that provide building blocks for new collagen synthesis.
Research has demonstrated that collagen peptide supplementation can improve skin hydration, elasticity, and wound healing. A 12-week study with 55 men found that 15g daily collagen peptides led to significantly faster recovery of maximum strength and explosive power after muscle-damaging exercise.
Collagen peptides work synergistically with signaling peptides like BPC-157 or GHK-Cu. The signaling peptides increase collagen synthesis capacity while the collagen peptides provide raw materials for that enhanced production.
PEDF-derived peptides
Pigment epithelium-derived factor (PEDF) peptides have shown promise specifically for tendon regeneration. Research demonstrates these peptides have mitogenic effects on tendon stem and progenitor cells, increasing their proliferation and potentially accelerating tendon repair.
This remains an emerging area with limited human data, but the specific targeting of tendon stem cells makes PEDF-derived peptides interesting for researchers focused on tendon healing optimization.
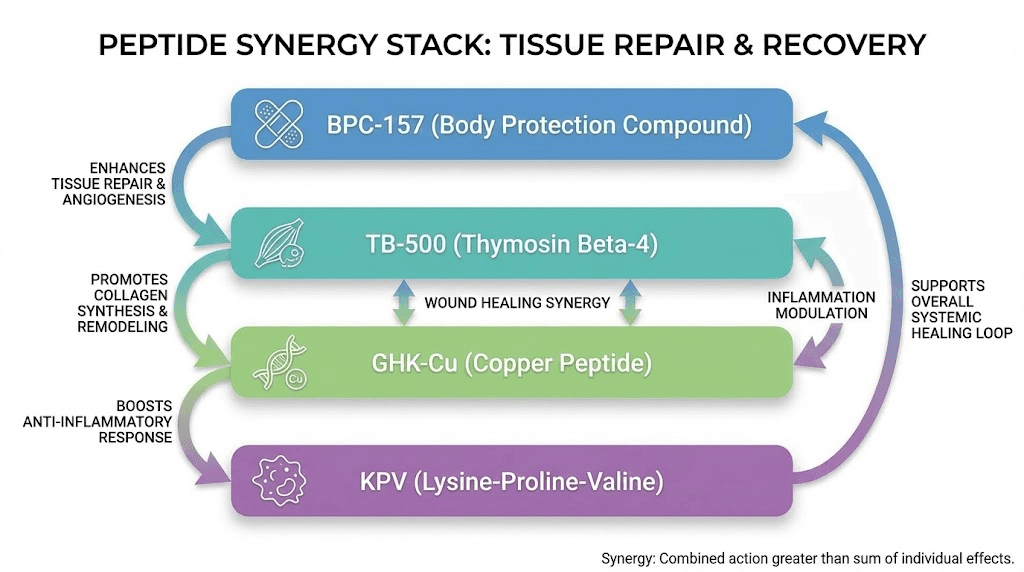
Stacking strategies for tissue repair
Single peptides can produce meaningful results. But the complexity of tissue repair, with its multiple overlapping phases and pathways, often responds better to strategic combinations. Different peptides address different aspects of healing, and thoughtful stacking can produce outcomes superior to any single agent.
The BPC-157 and TB-500 stack
This is the most common tissue repair stack, and for good reason. BPC-157 and TB-500 work through complementary mechanisms that together address most aspects of tissue healing.
BPC-157 enhances angiogenesis and fibroblast activation while promoting collagen production. TB-500 promotes actin polymerization and cell migration, getting repair cells to the injury site faster. Together, they support faster restoration of tissue integrity and biomechanical strength.
TB-500 affects cellular migration, accelerating the transport of fibroblasts to wounds. BPC-157 has positive effects on these fibroblasts once they arrive, resulting in increased collagen production. The combination addresses both recruitment and activation of repair cells.
For this stack, typical protocols use BPC-157 at 250-500mcg daily (or twice daily for serious injuries) combined with TB-500 at 2-4mg twice weekly. The BPC-157 is often injected near the injury site while TB-500 can be administered anywhere due to its systemic action.
Duration for the stack typically extends 8-12 weeks minimum. The loading phase for TB-500 usually runs 4-6 weeks at higher doses before transitioning to maintenance, while BPC-157 is maintained at consistent levels throughout.
Adding GHK-Cu to the stack
For injuries requiring significant collagen rebuilding, adding GHK-Cu to the BPC-157/TB-500 stack can enhance outcomes. GHK-Cu provides additional collagen synthesis stimulation and the gene-modulating effects that may improve tissue quality long-term.
The triple stack is particularly relevant for tendon and ligament injuries where collagen organization determines functional outcomes. It is also valuable for older researchers whose declining natural GHK-Cu levels may limit baseline repair capacity.
Protocol: Add GHK-Cu at 1-3mg daily to the standard BPC-157/TB-500 combination. Some researchers inject GHK-Cu separately from the other peptides, though combining in the same syringe is also practiced.
Including KPV for inflammatory conditions
When excessive inflammation complicates tissue repair, adding KPV to the stack addresses this limiting factor. This is particularly relevant for autoimmune-related injuries, gut healing, and chronic wounds with persistent inflammatory states.
The anti-inflammatory effect of KPV allows the proliferative and remodeling phases to proceed without constant interference from inflammatory cytokines. This can break the cycle of damage and incomplete repair that characterizes many chronic healing problems.
For gut healing specifically, the BPC-157/KPV combination has become popular among researchers. BPC-157 directly repairs gut tissue while KPV modulates the inflammation that often perpetuates intestinal damage.
Stack timing and administration
When using multiple peptides, timing and administration logistics become important.
Twice daily dosing: BPC-157 and GHK-Cu are often dosed twice daily (morning and evening) for optimal levels. TB-500 and KPV can be dosed once daily or even less frequently.
Injection sites: BPC-157 works best when injected near the injury site. TB-500 works systemically and can be injected anywhere. GHK-Cu can be targeted or systemic depending on goals.
Reconstitution: Each peptide should typically be reconstituted in its own vial. While some researchers mix peptides in the same syringe for injection, this should be done immediately before use rather than storing mixed solutions. Use the reconstitution calculator for proper dilutions.
Storage: Reconstituted peptides should be refrigerated and used within 4-6 weeks. Check our guide on peptide storage and stability for detailed information.
Protocols by injury type
Different tissues have different healing characteristics and respond differently to peptide interventions. Here are evidence-informed approaches for common injury types.
Tendon injuries
Tendons have notoriously poor blood supply and heal slowly compared to other tissues. Peptide protocols for tendons should prioritize angiogenesis and collagen synthesis.
Primary peptides: BPC-157 is the clear first choice given its dramatic effects on tendon fibroblasts and growth hormone receptor expression. TB-500 adds systemic healing support and enhanced cell migration.
Protocol example:
BPC-157: 500mcg twice daily, injected subcutaneously 1-2 inches from the injury site
TB-500: 5mg twice weekly during loading (weeks 1-4), then 2.5mg twice weekly maintenance
Duration: 10-12 weeks minimum, extending if improvement continues
Considerations: Do not stop when pain resolves. Tendons continue healing internally for weeks after symptoms improve. Stopping early significantly increases re-injury risk. The loading phase of TB-500 is particularly important for tendon healing.
Muscle strains and tears
Muscles have better blood supply than tendons and generally heal faster. However, optimizing healing speed and preventing fibrosis (scar tissue formation) improves functional outcomes.
Primary peptides: TB-500 excels at muscle repair due to its effects on satellite cell activation and migration. BPC-157 provides complementary growth factor support.
Protocol example:
TB-500: 4-6mg twice weekly during acute phase (weeks 1-4), then 2mg twice weekly
BPC-157: 250-500mcg daily, injection site not critical for muscles due to good vascularization
Duration: 6-8 weeks for moderate strains, 10-12 weeks for significant tears
Considerations: Resume activity gradually even when feeling recovered. Newly healed muscle tissue may not yet have full strength or flexibility. Use strength-focused protocols during later recovery stages.
Ligament injuries
Ligaments share many characteristics with tendons and respond similarly to peptide protocols. The emphasis is on collagen quality and structural integrity.
Primary peptides: BPC-157 and TB-500 stack is considered ideal for ligament tears based on their complementary mechanisms. Adding GHK-Cu may improve long-term collagen organization.
Protocol example:
BPC-157: 500mcg twice daily near the injured ligament
TB-500: 5mg twice weekly loading phase, then 2-3mg twice weekly
GHK-Cu: 2-3mg daily (optional addition)
Duration: 12 weeks minimum for significant ligament injuries
Considerations: Ligament healing is slow. Even with peptide support, expect 3-6 months before full structural recovery. Peptides accelerate the process but cannot eliminate it entirely.
Gut healing
The gastrointestinal tract presents unique challenges due to constant exposure to stomach acid, bacteria, and dietary irritants. Protocols must address both repair and the inflammatory drivers that perpetuate damage.
Primary peptides: BPC-157 is the cornerstone given its gastric origin and demonstrated gut healing effects. KPV addresses the inflammatory component that often prevents complete recovery.
Protocol example:
BPC-157: 250-500mcg twice daily, can be taken orally for gut targets
KPV: 500mcg-1mg daily, oral administration
Duration: 8-12 weeks, with reassessment of symptoms and inflammatory markers
Considerations: Address underlying causes of gut damage alongside peptide therapy. Dietary modifications, stress reduction, and elimination of triggering foods often necessary for lasting results. See our complete guide on peptides for gut health.
Chronic wounds
Wounds that fail to heal after 4-6 weeks are considered chronic and often require addressing underlying factors like poor circulation, infection, or systemic inflammation.
Primary peptides: GHK-Cu is particularly effective for skin wounds given its collagen-enhancing and gene-modulating effects. BPC-157 adds angiogenic support to improve blood supply to the wound bed.
Protocol example:
GHK-Cu: 2-3mg daily, subcutaneous near wound margins
BPC-157: 250mcg twice daily, subcutaneous near wound
Topical GHK-Cu: 0.5-2% serum applied directly to wound bed 1-2x daily
Duration: Until wound closure, then 2-4 additional weeks to optimize tissue quality
Considerations: Chronic wounds often have underlying causes that must be addressed. Infection, diabetes, venous insufficiency, and nutritional deficiencies can prevent healing despite peptide support. Comprehensive wound care protocols remain essential.
Post-surgical recovery
Surgery creates controlled tissue damage that requires healing. Peptide protocols can accelerate recovery, reduce complications, and improve functional outcomes.
Primary peptides: BPC-157 and TB-500 provide broad healing support. GHK-Cu can be added for surgeries involving significant connective tissue repair. KPV may help if excessive post-surgical inflammation occurs.
Protocol example:
Pre-surgery: Some researchers begin BPC-157 3-5 days before surgery
Post-surgery: BPC-157 500mcg twice daily + TB-500 4mg twice weekly
Duration: 6-8 weeks for minor procedures, 12+ weeks for major surgeries
Considerations: Discuss any peptide use with your surgical team. Some peptides may theoretically affect bleeding or other surgical concerns, though evidence for significant interactions is limited. Wait for appropriate wound closure before injecting near surgical sites.
Expected timelines for tissue repair
Understanding realistic timelines helps set appropriate expectations and guides protocol duration decisions. Peptides accelerate healing but cannot eliminate the biological time requirements of tissue regeneration.
Initial response phase (Days 1-7)
During the first week, peptides begin modulating the inflammatory response and preparing the healing environment. Measurable molecular changes occur, such as the sevenfold increase in growth hormone receptor expression seen with BPC-157 by day three.
Symptom improvement during this phase is typically modest. Pain may decrease somewhat due to reduced inflammation, but structural repair has just begun. This is not the time to increase activity based on feeling better.
Early proliferation phase (Weeks 1-3)
Cell migration and proliferation accelerate during this period. New blood vessels begin forming, and collagen production increases. Researchers often report meaningful symptom improvement starting around week 2.
However, the newly forming tissue is fragile. It has not yet organized into strong, functional structures. Continuing peptide support and limiting stress on healing tissue remains critical.
Active repair phase (Weeks 3-8)
This is when most visible and functional improvement occurs. Collagen fibers organize, tissue strength increases, and pain typically decreases substantially. Many researchers make the mistake of stopping peptides during this phase because they feel recovered.
Internal healing continues well after symptoms resolve. Stopping peptides prematurely often leads to incomplete repair and elevated re-injury risk. Protocols should continue through the full duration even when feeling recovered.
Remodeling phase (Weeks 8-24)
The final phase involves restructuring and strengthening newly formed tissue. Collagen fibers realign along stress lines, cross-linking increases, and tissue approaches full functional strength.
Peptides can support this phase, particularly those that affect collagen organization like GHK-Cu. However, appropriate mechanical loading and gradual return to activity also play important roles in optimizing tissue remodeling.
Factors affecting healing timeline
Several factors influence how quickly individuals respond to tissue repair peptides:
Age: Older individuals typically heal more slowly, both due to declining endogenous peptide levels and reduced cellular proliferation capacity. They may need longer protocols and higher doses.
Injury severity: Partial tears heal faster than complete ruptures. Acute injuries generally respond better than chronic degeneration. Severity should guide protocol intensity and duration.
Blood supply: Well-vascularized tissues (muscles) heal faster than poorly vascularized ones (tendons, cartilage). Protocols for poorly vascularized tissues should emphasize angiogenesis and extend duration.
Nutrition: Adequate protein, vitamin C, zinc, and copper are essential for tissue repair. Caloric deficits can impair healing even with optimal peptide support. Ensure nutritional needs are met alongside peptide protocols.
Concurrent conditions: Diabetes, autoimmune diseases, and chronic infections impair healing capacity. These conditions may require longer protocols, additional peptides like KPV for inflammation, and treatment of the underlying condition.
Safety considerations and side effects
Tissue repair peptides have generally favorable safety profiles in the available research, but understanding potential risks enables informed decision-making.
BPC-157 safety
BPC-157 has been well-tolerated in preclinical studies with no significant adverse effects reported at therapeutic doses. It has a wide safety margin in animal studies, with doses many times the therapeutic level not producing obvious toxicity.
Limited human clinical data exists, primarily from studies on inflammatory bowel disease. These studies have not revealed significant safety concerns at the doses tested.
Theoretical concerns include potential effects on tumor growth due to angiogenic properties. While no evidence suggests BPC-157 promotes cancer, researchers with active malignancies or significant cancer risk factors may want to exercise caution.
TB-500 safety
Thymosin Beta-4, the parent molecule of TB-500, has been extensively studied and has a favorable safety profile. It exists naturally in high concentrations in platelets and wound fluid, suggesting biological tolerance.
TB-500 has been used in veterinary applications, particularly horse racing, with limited reports of adverse effects. Human data is more limited but has not revealed significant safety issues.
Similar theoretical concerns about angiogenesis and potential tumor effects apply to TB-500 as with BPC-157.
GHK-Cu safety
As a naturally occurring human peptide that declines with age, GHK-Cu has an inherently favorable safety profile. The body is adapted to this molecule and its copper-bound form.
Topical GHK-Cu is widely used in cosmetics with an excellent safety record. Injectable use has fewer data but has not revealed significant safety concerns at typical doses.
Copper toxicity is theoretically possible with very high doses, but the amounts used in GHK-Cu protocols are far below toxicity thresholds. Normal kidney function easily handles excretion of the copper load from typical protocols.
KPV safety
KPV has been well-tolerated in preclinical studies, with no significant adverse effects reported at therapeutic doses. Unlike many anti-inflammatory agents, KPV does not appear to suppress immune function, increase infection risk, or cause tissue thinning associated with corticosteroids.
The peptide's derivation from alpha-MSH means it lacks the melanocortin receptor effects that could cause pigmentation changes or other hormonal effects seen with the parent molecule.
General peptide safety considerations
Source quality: The unregulated nature of research peptide markets means quality varies significantly between suppliers. Contamination, incorrect dosing, and degraded products represent real risks. Choose reputable suppliers with third-party testing. See our guide on peptide testing labs.
Reconstitution and storage: Improper handling can degrade peptides or introduce contamination. Use bacteriostatic water, maintain sterile technique, and refrigerate reconstituted peptides. Review proper bacteriostatic water protocols before beginning.
Injection site reactions: Mild redness, itching, or swelling at injection sites occurs occasionally. These typically resolve quickly and rarely require protocol modification.
Lack of long-term data: While short-term safety appears favorable, long-term effects of extended peptide use are not well-characterized. Taking breaks between extended protocols is a reasonable precaution.
Contraindications and precautions
Individuals with the following conditions should exercise particular caution and ideally consult healthcare providers before using tissue repair peptides:
Active cancer or history of malignancy (due to theoretical concerns about angiogenesis)
Pregnancy or breastfeeding (inadequate safety data)
Autoimmune conditions (may affect immune modulation)
Kidney or liver disease (may affect metabolism and excretion)
Currently taking blood thinners or about to undergo surgery
Note that due to the necessity for additional clinical trials and the predominant use of small animal models in existing studies, the FDA has not granted approval for BPC-157 or most other tissue repair peptides for medical treatment. They remain research compounds with promising but incompletely characterized safety profiles.
Practical implementation guide
Moving from theory to practice requires attention to logistics, supplies, and proper technique. Here is what you need to know to implement tissue repair peptide protocols effectively.
Obtaining peptides
Research peptides are available from various suppliers serving the scientific research community. Quality varies significantly, so selecting reputable sources is critical.
Look for suppliers that provide certificates of analysis from independent third-party laboratories. These should verify identity, purity, and absence of contamination. Peptide purity of 98% or higher is generally expected for research applications.
Avoid sources that make medical claims, sell to individuals without research purposes stated, or lack quality documentation. These red flags often correlate with quality issues.
Peptides typically arrive as lyophilized (freeze-dried) powder in sterile vials. This form is stable for extended periods when stored properly. Reconstitution happens immediately before beginning use.
Reconstitution procedure
Proper reconstitution is essential for maintaining peptide integrity and ensuring accurate dosing.
Supplies needed:
Bacteriostatic water (sterile water with 0.9% benzyl alcohol preservative)
Alcohol swabs
Insulin syringes (typically 1mL with 29-31 gauge needles)
Clean work surface
Procedure:
Allow the peptide vial to reach room temperature if refrigerated
Clean the vial stopper with an alcohol swab
Draw the desired amount of bacteriostatic water into the syringe
Insert the needle through the stopper and release water slowly down the side of the vial
Do not shake. Gently swirl to dissolve the peptide cake
Wait until fully dissolved (usually 1-2 minutes)
Label the vial with reconstitution date and concentration
Use the peptide reconstitution calculator to determine how much bacteriostatic water to add for your desired concentration. Common concentrations allow for convenient dosing with standard insulin syringes.
Injection technique
Subcutaneous injection is the most common administration route for tissue repair peptides.
Site selection: For BPC-157, inject within 1-2 inches of the injury when possible. This may not be practical for all injuries. Abdomen (avoiding 2 inches around the navel) and thigh are convenient alternative sites. For TB-500, site selection does not affect outcomes due to systemic distribution.
Procedure:
Clean the injection site with an alcohol swab
Pinch a fold of skin between thumb and forefinger
Insert the needle at 45-90 degree angle
Inject slowly and steadily
Remove the needle and apply light pressure if needed
Rotate injection sites to prevent tissue irritation
Dispose of used syringes properly in a sharps container. Never reuse syringes.
Storage and stability
Proper storage maintains peptide potency throughout the protocol.
Lyophilized peptides: Store in a cool, dark place. Refrigeration extends shelf life but is not required for short-term storage. Avoid freeze-thaw cycles.
Reconstituted peptides: Must be refrigerated at 2-8 degrees Celsius. Use within 4-6 weeks of reconstitution. Never freeze reconstituted peptides. Check our detailed guide on how long peptides last.
If a reconstituted peptide solution becomes cloudy, changes color, or develops particles, discard it and use a fresh vial.
Tracking progress
Documenting response to peptide protocols helps optimize outcomes and informs future decisions.
Baseline assessment: Before starting, document current pain levels (using a 0-10 scale), range of motion limitations, functional restrictions, and any objective measurements available.
Regular check-ins: Weekly assessments track trends over time. Note changes in pain, function, and any side effects experienced. Photos can document visible healing progress for wounds or skin applications.
Milestones: Note when significant improvements occur, when symptoms resolve, and when full function returns. This information guides decisions about protocol duration and future use.
Combining with other therapies
Peptides work best as part of comprehensive healing protocols, not as standalone treatments.
Physical therapy: Appropriate movement and loading are essential for optimal tissue remodeling. Work with qualified professionals to develop rehabilitation programs that complement peptide healing.
Nutrition: Ensure adequate protein intake (1.2-1.6g/kg bodyweight for healing), vitamin C, zinc, and copper. Consider collagen supplementation to provide building blocks for tissue repair.
Sleep: Growth hormone release peaks during deep sleep. Adequate sleep duration and quality support the hormonal environment peptides optimize.
Stress management: Chronic stress elevates cortisol, which impairs healing. Address stress factors as part of comprehensive recovery.
Frequently asked questions
Which peptide is best for tendon repair?
BPC-157 is generally considered the best single peptide for tendon repair due to its dramatic effects on tendon fibroblasts and growth hormone receptor expression. However, combining BPC-157 with TB-500 often produces better outcomes than either alone, as TB-500 enhances cell migration while BPC-157 activates repair processes once cells arrive at the injury site.
How long does it take for tissue repair peptides to work?
Initial molecular changes occur within days, but meaningful symptom improvement typically begins around week 2-3 of consistent use. Full healing of significant injuries requires 8-12 weeks or longer depending on injury severity and tissue type. Tendons and ligaments heal more slowly than muscles. Continue protocols through full recommended duration even when symptoms resolve, as internal healing continues after pain disappears.
Can I use multiple peptides at the same time?
Yes, stacking multiple peptides is common practice. The most popular combination for tissue repair is BPC-157 plus TB-500, which address complementary mechanisms. GHK-Cu can be added for enhanced collagen synthesis. KPV can be added when inflammation is a significant factor. Each peptide should be reconstituted in its own vial but can be combined in the same syringe for injection.
Do I need to inject near the injury site?
For BPC-157, injecting within 1-2 inches of the injury appears to enhance local effects and is recommended when practical. TB-500 works systemically regardless of injection site, so convenience can guide site selection. For systemic benefits or when injury site injection is impractical, subcutaneous injection in the abdomen or thigh is effective for both peptides.
Are tissue repair peptides safe?
Available research suggests favorable safety profiles for BPC-157, TB-500, GHK-Cu, and KPV at typical doses. They have been well-tolerated in preclinical studies with no significant adverse effects reported. However, these peptides are not FDA-approved for medical use, and long-term safety data is limited. Source quality is important, as unregulated manufacturing introduces risks of contamination or incorrect dosing. Individuals with active cancer, pregnancy, or serious medical conditions should exercise particular caution.
Should I continue peptides after symptoms resolve?
Yes. A common mistake is stopping peptides when pain subsides around weeks 2-3. At this point, tissue is still healing internally. Stopping early leads to incomplete repair and significantly elevated re-injury risk. Complete the full recommended protocol duration of 6-8 weeks minimum for mild injuries and 10-12 weeks for significant injuries, continuing even when feeling recovered.
Do tissue repair peptides show up on drug tests?
Some peptides are banned by athletic organizations. TB-500 (Thymosin Beta-4) is specifically listed on the World Anti-Doping Agency prohibited list. BPC-157 is not currently on standard testing panels but is banned by some organizations. If athletic competition drug testing is a concern, verify the status of specific peptides with relevant governing bodies before use. See our article on BPC-157 and drug testing.
Can peptides help with chronic injuries that have not healed?
Peptides show particular promise for chronic healing problems. They can help break cycles of incomplete repair by enhancing the biological signals that drive tissue regeneration. Chronic injuries often benefit from stacks that include both repair peptides like BPC-157 and anti-inflammatory peptides like KPV to address the persistent inflammation that often prevents chronic wound resolution.
What dosage should I use for severe versus mild injuries?
For BPC-157, mild injuries typically respond to 250mcg once or twice daily. Severe injuries may benefit from 500mcg twice daily. For TB-500, the loading phase dose of 4-6mg twice weekly is more important than the maintenance dose, which can be reduced to 2mg twice weekly after the first 4-6 weeks. Always err on the side of longer protocols rather than shorter ones.
Can I take tissue repair peptides orally?
BPC-157 has shown effectiveness with oral administration in some studies, particularly for gut healing applications. Its stability in gastric acid, unusual for a peptide, allows for oral bioavailability. KPV can also be taken orally for gut targets. TB-500 and GHK-Cu are typically administered by injection, as oral bioavailability is limited for these peptides. Use the peptide dosage calculator regardless of administration route.
For researchers serious about optimizing tissue repair protocols, SeekPeptides provides the most comprehensive resource available.
Members access evidence-based guides, proven protocols, dosage calculators, and a community of experienced researchers who have navigated these exact questions. Whether you are dealing with a stubborn tendon injury, a muscle strain that will not heal, or chronic wounds that resist conventional treatment, the tools and knowledge within SeekPeptides can transform your approach to recovery.



