Feb 3, 2026
Tired of conflicting information about peptides for weight loss during menopause? One source says semaglutide is the answer. Another swears by growth hormone peptides. A third insists that nothing works without estrogen replacement first. You read five articles and end up with six different opinions, none of them backed by the kind of specific data that would actually help you make a decision.
Here is what nobody tells you. Menopause does not just make weight loss harder. It fundamentally rewires how your body stores fat, burns calories, and responds to the signals that regulate appetite. The metabolism you relied on for decades? It has shifted. The fat distribution patterns you understood? They have changed. And the strategies that worked in your thirties and forties are now fighting against hormonal biology that has rewritten the rules entirely.
This is not another vague overview telling you to "eat clean and exercise more." This guide breaks down the seven most researched peptides for menopause weight loss with specific protocols, real clinical data, and practical stacking strategies built for women over 40 navigating the metabolic chaos of perimenopause and postmenopause. You will find exact dosing ranges, week-by-week timelines, head-to-head comparisons, and the science behind why certain peptides work differently in menopausal bodies. SeekPeptides has compiled everything from clinical trials, endocrinology research, and real-world protocols into one comprehensive resource so you can stop guessing and start making informed decisions about your metabolic health.
Why menopause makes weight loss so difficult
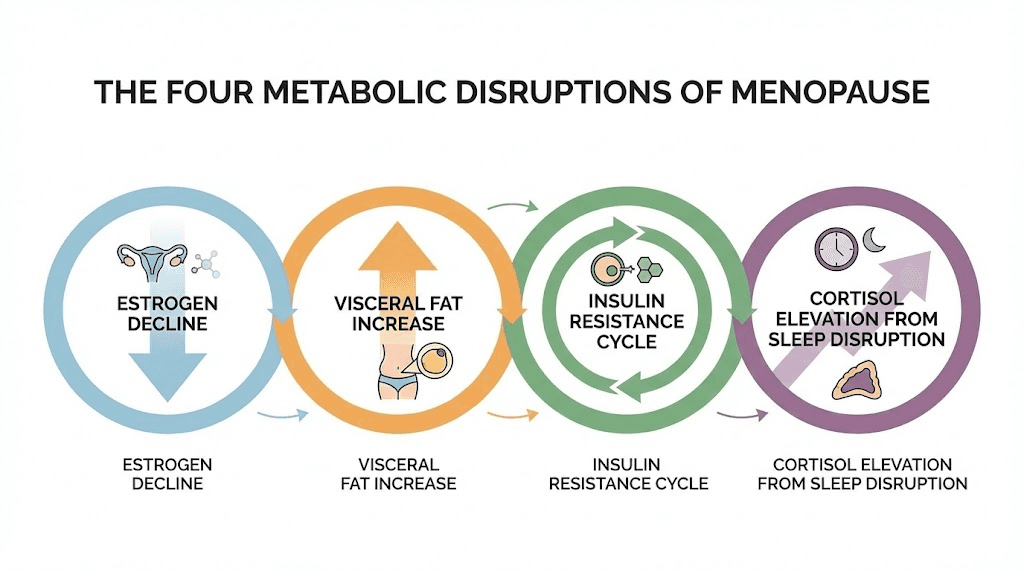
Before exploring which peptides can help, you need to understand exactly what menopause does to your metabolism. This is not a simple matter of eating less and moving more. The hormonal shifts that occur during perimenopause and postmenopause create a cascade of metabolic changes that make belly fat stubbornly resistant to conventional approaches. Women gain an average of 1.5 pounds per year during midlife, accumulating roughly 12 pounds within eight years of menopause. That number might sound manageable on paper. Living through it feels different entirely.
The weight gain is not random. It follows specific biological patterns driven by hormonal changes that affect everything from where fat gets deposited to how efficiently your mitochondria produce energy. Understanding these mechanisms is the first step toward choosing the right peptide protocol for women.
The estrogen-metabolism connection
Estrogen does far more than regulate your reproductive system. It is one of the most powerful metabolic regulators in the female body, influencing insulin sensitivity, fat oxidation, appetite signaling, and mitochondrial function. When estrogen levels decline during menopause, every single one of these metabolic processes takes a hit.
The numbers tell the story clearly. Metabolism drops approximately 200 to 250 calories per day during menopause. That is the equivalent of a small meal, gone from your daily energy expenditure without any change in activity or diet. Over a year, that deficit alone accounts for 20 to 25 pounds of potential weight gain if eating habits stay the same. And that is just the resting metabolic rate change, before factoring in the other hormonal disruptions happening simultaneously.
Estrogen also directly affects how your body partitions fuel. In premenopausal women, estrogen promotes fat oxidation, meaning your body preferentially burns fat for energy. When estrogen drops, the body shifts toward storing fat and burning glucose instead. This metabolic switch is why many women report that their bodies suddenly feel "different" during perimenopause, even before any visible weight changes occur. The internal fuel dynamics have already shifted.
This matters for peptide selection because different peptides target different aspects of this metabolic disruption. Some address appetite signaling. Others target fat mobilization directly. And some work on the growth hormone axis to restore the body composition regulation that estrogen used to support. Understanding how peptides work at the mechanistic level helps you choose the right approach for your specific situation.
Visceral fat redistribution explained
This is the change that frustrates women the most. Before menopause, estrogen directs fat storage primarily to the hips, thighs, and buttocks. Subcutaneous fat. The kind that sits under the skin and, while cosmetically bothersome to some, is metabolically relatively harmless.
Menopause flips this pattern entirely.
Without adequate estrogen, fat storage shifts dramatically to the abdominal cavity. Visceral fat, the deep fat that wraps around organs, increases from 5 to 8 percent of total body weight to 10 to 15 percent. This is not just a cosmetic issue. Visceral fat is metabolically active tissue that secretes inflammatory cytokines, disrupts insulin signaling, and increases cardiovascular risk. Menopausal women are three times more likely to develop obesity and metabolic syndrome compared to their premenopausal counterparts. The redistribution happens even in women whose total weight stays stable, meaning the scale might not change while the composition of body fat shifts in dangerous directions.
Peptides like tesamorelin specifically target visceral fat, which is why they deserve special attention in the context of menopause. The fat loss peptide category includes several compounds that address visceral fat through different mechanisms, and matching the right peptide to the right problem makes all the difference in outcomes.
Insulin resistance and blood sugar changes
Estrogen enhances insulin sensitivity. Without it, cells become more resistant to insulin signaling, creating a metabolic environment where blood sugar regulation deteriorates and the body becomes more efficient at converting excess glucose to stored fat. Research shows that postmenopausal women have significantly higher fasting insulin levels and reduced glucose tolerance compared to premenopausal women of similar age and body composition.
This insulin resistance creates a vicious cycle. Higher insulin levels promote fat storage. More visceral fat worsens insulin resistance. Worsening insulin resistance drives higher insulin levels. Breaking this cycle requires addressing the insulin signaling pathway directly, which is exactly where GLP-1 receptor agonists like semaglutide and tirzepatide show their most dramatic effects. These peptides do not just suppress appetite. They fundamentally improve insulin sensitivity and glucose metabolism, attacking the root metabolic dysfunction rather than just the symptom of weight gain.
Understanding this insulin connection also explains why MOTS-C has generated such interest in the menopause research space. As a mitochondrial-derived peptide that activates the AMPK pathway, MOTS-C addresses the cellular energy dysfunction that underlies menopausal insulin resistance. The research is still early, but the mechanistic rationale is compelling.
Sleep disruption and cortisol
Hot flashes. Night sweats. Anxiety. The sleep disruption during menopause is not just uncomfortable. It is metabolically destructive.
Poor sleep increases cortisol production. Elevated cortisol promotes visceral fat storage, breaks down muscle tissue, increases appetite, and impairs insulin sensitivity. Studies consistently show that sleeping fewer than six hours per night is associated with significantly higher body mass index and waist circumference, with the effect being even more pronounced in menopausal women. The combination of estrogen decline and chronic sleep disruption creates a hormonal environment that is almost perfectly designed for weight gain.
This is where sleep-supporting peptides can play an indirect but important role in weight management. Some women find that addressing sleep quality through peptides like ipamorelin, which promotes deeper sleep as a secondary benefit, actually accelerates their fat loss results more than adding another fat-burning compound would. The growth hormone pulse that occurs during deep sleep is one of the body most powerful fat-mobilizing signals, and restoring that sleep architecture is foundational to any effective peptide protocol.
The seven best peptides for menopause weight loss
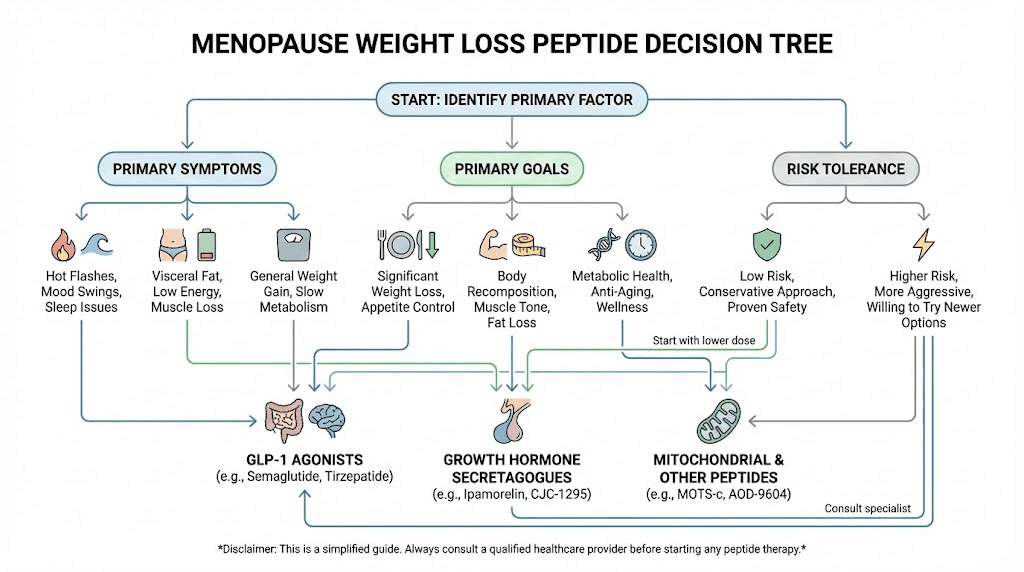
Not all peptides are created equal when it comes to menopausal weight loss. Some target appetite. Others address fat metabolism directly. And a few work on the growth hormone axis to restore the body composition regulation that declining hormones have disrupted. The best peptides for weight loss in a menopausal context need to address the specific metabolic changes outlined above, not just suppress appetite or boost metabolism in a generic way.
Each peptide below has been evaluated based on its mechanism of action, clinical evidence specifically relevant to menopausal women, practical considerations like dosing and side effects, and how well it integrates into a comprehensive protocol. Some have robust clinical trial data. Others have strong mechanistic evidence with clinical data still emerging. Understanding the difference matters when making informed decisions about your peptide journey.
Semaglutide (GLP-1 agonist)
Semaglutide is the most well-known weight loss peptide available, and for good reason. As a GLP-1 receptor agonist, it mimics the incretin hormone that regulates appetite, insulin secretion, and gastric emptying. The clinical data for weight loss is among the strongest of any pharmaceutical intervention, and recent research has specifically examined its effectiveness in menopausal and postmenopausal women.
The mechanism is straightforward but powerful. Semaglutide binds to GLP-1 receptors in the brain, particularly in the hypothalamus, reducing hunger signals and increasing satiety. It slows gastric emptying, meaning food stays in the stomach longer and you feel full sooner. But it also improves insulin sensitivity and promotes beta-cell function in the pancreas, addressing the insulin resistance that menopause creates.
Here is what the data shows for menopausal women specifically. A Mayo Clinic study published in a major medical journal found that postmenopausal women using semaglutide in combination with hormone replacement therapy achieved approximately 30 percent more weight loss compared to semaglutide alone. This is a significant finding because it suggests that addressing estrogen deficiency alongside GLP-1 agonist therapy produces synergistic effects. Use the semaglutide dosage calculator to determine appropriate starting doses based on individual factors.
Standard protocols start at 0.25mg weekly for the first four weeks, titrating up to 0.5mg, then 1.0mg, and potentially 1.7mg or 2.4mg depending on response and tolerance. The slow titration is essential for managing gastrointestinal side effects, which are the most common complaint. Nausea, typically mild to moderate, affects roughly 40 percent of users during the titration phase but usually resolves within two to four weeks at each dose level.
For menopausal women, semaglutide addresses multiple metabolic disruptions simultaneously: appetite dysregulation, insulin resistance, and the visceral fat accumulation pattern. The comparison with tirzepatide is worth examining carefully, as the dual-agonist approach of tirzepatide may offer additional benefits for some women.
Tirzepatide (dual GLP-1/GIP agonist)
Tirzepatide represents the next evolution in incretin-based therapies. Unlike semaglutide, which targets only GLP-1 receptors, tirzepatide is a dual agonist that activates both GLP-1 and GIP (glucose-dependent insulinotropic polypeptide) receptors. This dual mechanism produces weight loss results that consistently exceed those of semaglutide in head-to-head trials, and the data in menopausal women is particularly compelling.
The SURMOUNT trials enrolled 2,542 women and demonstrated approximately 20 percent total body weight reduction regardless of reproductive stage. That number is remarkable. Twenty percent weight loss means a 180-pound woman could expect to lose around 36 pounds over the treatment period. But the data gets more interesting when you look at the combination with hormone replacement therapy.
A Mayo Clinic study published in the Lancet Obstetrics found that women using tirzepatide alongside HRT achieved 17 percent weight loss compared to 14 percent with tirzepatide alone. That is 35 percent more weight loss from adding HRT. Perhaps more striking, 45 percent of women in the HRT plus tirzepatide group achieved 20 percent or greater weight loss, compared to only 18 percent without HRT. These numbers strongly suggest that estrogen replacement and GLP-1/GIP agonism work synergistically in menopausal women.
Dosing follows a similar titration pattern to semaglutide. Starting at 2.5mg weekly, increasing to 5mg after four weeks, then 7.5mg, 10mg, 12.5mg, and potentially 15mg based on response and tolerance. The gastrointestinal side effects are similar to semaglutide but may be slightly better tolerated due to the GIP receptor activation, which has some gastroprotective properties. You can explore the detailed tirzepatide dosing guide for comprehensive protocols and the semaglutide versus tirzepatide comparison for a thorough breakdown of how these two compounds differ in practice.
For menopausal women, tirzepatide may have an edge over semaglutide because GIP receptors are found in adipose tissue and may directly influence fat metabolism beyond what GLP-1 alone can achieve. The dual mechanism also appears to better preserve lean mass during weight loss, which is critically important during menopause when muscle preservation becomes increasingly challenging.
AOD-9604 (growth hormone fragment 176-191)
AOD-9604 takes a completely different approach to fat loss. Rather than targeting appetite or insulin signaling, this peptide is a modified fragment of human growth hormone, specifically amino acids 176 through 191, that directly stimulates fat metabolism without the broader effects of full growth hormone therapy. For menopausal women who cannot or prefer not to use GLP-1 agonists, AOD-9604 offers an alternative mechanism that targets fat cells directly.
The beauty of AOD-9604 is what it does not do. It does not raise IGF-1 levels. It does not increase insulin. It does not affect blood glucose. It does not carry the cancer risk concerns associated with elevated growth hormone. It specifically mimics the lipolytic (fat-burning) action of growth hormone while leaving the other effects behind. This selectivity makes it particularly attractive for menopausal women who may have other metabolic concerns that full GH therapy could complicate.
Clinical data from a 23-week trial showed that AOD-9604 produced 2.8 kilograms of fat loss compared to 0.8 kilograms in the placebo group. These numbers are more modest than GLP-1 agonists, which is an honest assessment. AOD-9604 is not going to produce 20 percent body weight reductions. But it offers a targeted approach to fat metabolism with an exceptionally clean side effect profile. The standard AOD-9604 dosage protocol runs 300 to 500 micrograms per day administered subcutaneously, typically on an empty stomach in the morning to maximize fat oxidation during fasting periods.
Expect initial changes around weeks four to six, with more significant results becoming apparent by weeks eight to ten. The side effect profile is remarkably mild, with injection site reactions being the most commonly reported issue. For women looking to address the visceral fat shift of menopause without the appetite suppression and gastrointestinal effects of GLP-1 agonists, AOD-9604 deserves serious consideration. Calculate exact dosing with the HGH fragment 176-191 calculator.
CJC-1295 with ipamorelin
The combination of CJC-1295 and ipamorelin is arguably the most popular growth hormone secretagogue stack in the peptide space, and it has specific relevance for menopausal weight management. Rather than providing exogenous growth hormone, this combination stimulates your own pituitary gland to produce and release more growth hormone in natural pulsatile patterns. For menopausal women experiencing the age-related decline in GH production that compounds the effects of estrogen loss, this approach addresses a fundamental hormonal deficiency.
CJC-1295 is a growth hormone releasing hormone (GHRH) analog with an extended half-life of 5.8 to 8.1 days. A single injection can increase growth hormone levels 2 to 10 times above baseline for six or more days and elevate IGF-I levels 1.5 to 3 times for 9 to 11 days. When combined with ipamorelin, a growth hormone releasing peptide (GHRP) that works through the ghrelin receptor, the two compounds produce a synergistic amplification of GH release that neither achieves alone.
Why does this matter for menopause? Growth hormone is a powerful regulator of body composition. It promotes lipolysis (fat breakdown), preserves lean muscle mass, improves sleep quality, enhances skin elasticity, and supports bone density. All of these functions decline during menopause. The CJC-1295 complete guide covers the full spectrum of benefits, but for weight loss specifically, the growth hormone elevation promotes preferential fat oxidation and muscle preservation during caloric deficit.
One of the most valuable secondary benefits for menopausal women is improved sleep architecture. The growth hormone pulse that this stack promotes occurs primarily during deep sleep, and many users report significantly better sleep quality within the first two weeks. Given that sleep disruption is both a symptom of menopause and a driver of weight gain, this dual benefit is clinically meaningful.
Dosing protocols typically involve 100 to 300 micrograms of CJC-1295 combined with 100 to 300 micrograms of ipamorelin, administered subcutaneously before bed. The nighttime dosing takes advantage of the natural growth hormone pulse during sleep. Use the CJC-1295 dosage calculator for precise calculations based on body weight. Body composition changes typically become measurable at 8 to 12 weeks, with improvements continuing over 4 to 6 months. One important note: this combination does not affect cortisol or prolactin levels, which is relevant for menopausal women who may already be dealing with cortisol dysregulation. Explore the ipamorelin versus CJC-1295 comparison and the ipamorelin side effects profile for additional context.
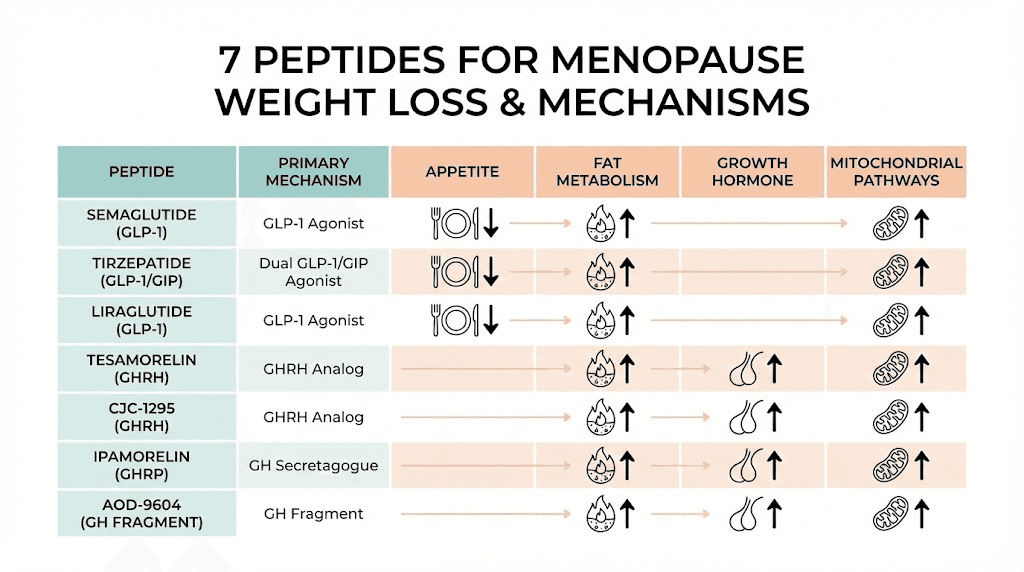
Tesamorelin (GHRH analog)
Tesamorelin holds a unique position in this list. It is the only peptide here with FDA approval specifically for reducing visceral adipose tissue, albeit in the context of HIV-associated lipodystrophy. That FDA approval means it has undergone rigorous clinical testing with robust data on visceral fat reduction, and the mechanistic basis for its effects applies equally to menopausal visceral fat accumulation.
The clinical numbers are compelling. Over 26 weeks, tesamorelin reduced visceral adipose tissue by a mean of 34 square centimeters compared to an increase of 8 square centimeters in the placebo group. That is a net difference of 42 square centimeters. In percentage terms, VAT reduction averaged 15 to 20 percent over the study period. Additionally, 69 percent of tesamorelin users achieved at least 8 percent VAT reduction compared to only 33 percent in the placebo group. Perhaps most intriguingly for menopausal women concerned about metabolic health, tesamorelin also reduced hepatic (liver) fat by 37 percent.
Tesamorelin works by stimulating the pituitary to release growth hormone, similar to CJC-1295 but through a different receptor interaction pattern. The studies showed similar efficacy in men and women, which is important to note because many growth hormone-related compounds show sex-dependent responses. For menopausal women specifically battling the estrogen-driven shift toward visceral fat accumulation, tesamorelin directly addresses the most metabolically dangerous component of menopausal weight gain.
Standard dosing is 2mg administered subcutaneously once daily. The side effect profile includes injection site reactions, joint pain, and peripheral edema in some users. Safety monitoring should include periodic IGF-1 levels and fasting glucose checks, as growth hormone stimulation can affect glucose metabolism. The peptide dosage chart provides reference ranges for tesamorelin alongside other growth hormone secretagogues.
MOTS-C (mitochondrial peptide)
MOTS-C is the most scientifically intriguing peptide on this list, and it represents a fundamentally different approach to metabolic regulation. Unlike the other compounds discussed, MOTS-C is a mitochondrial-derived peptide, a 16-amino-acid sequence encoded within the mitochondrial genome itself. It acts as a retrograde signal from mitochondria to the cell nucleus, activating the AMPK pathway, which is the master regulator of cellular energy balance.
Why is this relevant to menopause? Estrogen protects mitochondrial function. When estrogen declines, mitochondrial efficiency drops, contributing to the metabolic slowdown that characterizes menopause. MOTS-C essentially mimics one of the protective signals that estrogen used to help maintain. In ovariectomized mice, a standard model for studying menopausal metabolic changes, MOTS-C administration reduced fat accumulation and improved insulin sensitivity. Exercise, which is known to improve menopausal metabolic health, increases MOTS-C levels by 11.9 times in muscle tissue, suggesting that some of the metabolic benefits of exercise during menopause may be mediated through MOTS-C pathways.
The MOTS-C complete guide covers the full spectrum of this peptide research. The MOTS-C dosage chart outlines the protocols used in preclinical research, though it is critical to note that MOTS-C is still in the preclinical phase for therapeutic use. No human therapeutic trials have been completed yet. The animal data and mechanistic understanding are compelling, but this peptide should be approached with the understanding that human clinical validation is still forthcoming. Review the MOTS-C side effects profile for safety information based on available research.
For menopausal women interested in cutting-edge metabolic support, MOTS-C represents a fascinating research direction that addresses the mitochondrial dysfunction underlying menopausal metabolic changes. It is not a first-line weight loss peptide, but for those already using other approaches and looking for complementary metabolic support, the AMPK activation mechanism offers something that the other peptides on this list do not provide.
Sermorelin
Sermorelin is the original growth hormone releasing hormone analog, and it remains relevant for menopausal weight management despite being overshadowed by newer compounds. As a 29-amino-acid peptide that corresponds to the first 29 amino acids of natural GHRH, sermorelin stimulates natural growth hormone production without the supraphysiological peaks associated with exogenous GH administration.
The benefits of sermorelin for menopausal women extend beyond fat loss. Improved sleep quality, enhanced skin elasticity, better mood, and increased energy are commonly reported. The before and after results typically show gradual improvements in body composition over 3 to 6 months, with fat loss concentrated in the visceral compartment and lean mass preserved or slightly increased.
Sermorelin is often considered a gentler alternative to CJC-1295 with ipamorelin, with a shorter duration of action that more closely mimics natural GHRH release patterns. For menopausal women who are new to peptide protocols and prefer a conservative starting point, sermorelin offers a well-established option with decades of clinical use behind it. The sermorelin cost guide provides practical information about treatment expenses, and the compound integrates well into broader peptide stacking protocols designed for menopausal metabolic support.
Dosing typically ranges from 200 to 500 micrograms administered subcutaneously at bedtime. Like CJC-1295 with ipamorelin, the nighttime administration capitalizes on the natural sleep-associated GH pulse. Results are gradual, with initial improvements in sleep and energy often noticed within two to three weeks, and measurable body composition changes emerging over two to four months. The sermorelin and ipamorelin blend is worth reviewing for understanding how these compounds complement each other, though the protocols discussed in that article can be adapted for women with appropriate dose adjustments.
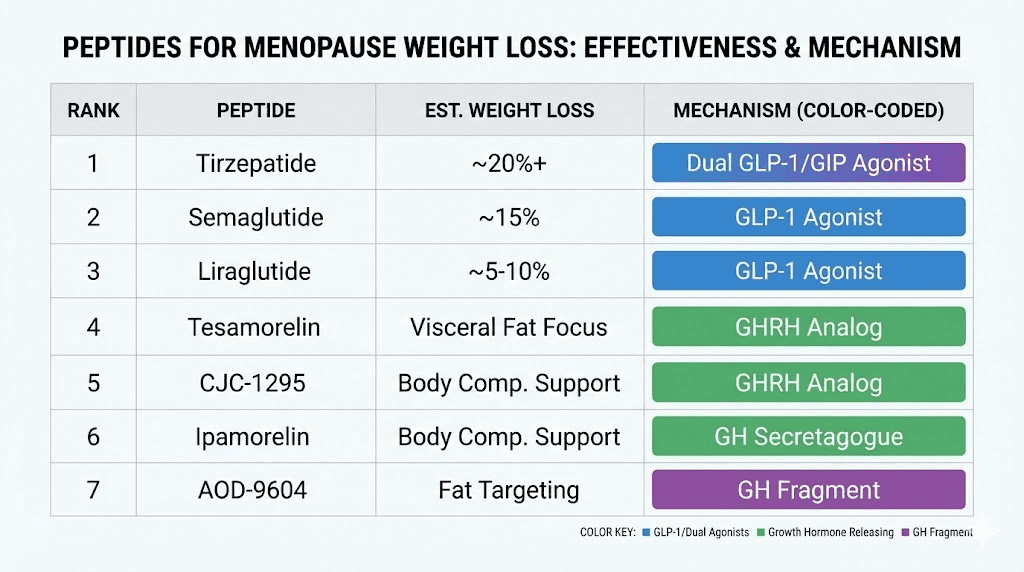
Head-to-head comparison table
Choosing between these peptides requires understanding how they compare across the factors that matter most: effectiveness, speed of results, side effects, and suitability for the specific metabolic challenges of menopause. This comparison of fat burning peptides should be read alongside the detailed profiles above, as the table provides a quick reference but not the full context needed for informed decision-making.
Peptide | Primary mechanism | Weight loss potential | Visceral fat targeting | Time to results | Side effect burden | Menopause relevance |
|---|---|---|---|---|---|---|
Semaglutide | GLP-1 appetite/insulin | High (15-20%) | Moderate | 4-8 weeks | Moderate (GI) | 9/10 |
Tirzepatide | GLP-1/GIP dual agonist | Very high (20%+) | Moderate-high | 4-8 weeks | Moderate (GI) | 10/10 |
AOD-9604 | Direct fat metabolism | Moderate (5-8%) | Moderate | 6-10 weeks | Low | 7/10 |
CJC-1295/Ipamorelin | GH secretion | Moderate (8-12%) | Moderate-high | 8-12 weeks | Low | 8/10 |
Tesamorelin | GHRH/visceral fat | Moderate (8-15%) | Very high | 8-12 weeks | Low-moderate | 9/10 |
MOTS-C | AMPK/mitochondrial | Emerging data | Moderate (animal) | Unknown (preclinical) | Low (limited data) | 7/10 (potential) |
Sermorelin | Natural GH release | Moderate (5-10%) | Moderate | 8-16 weeks | Low | 7/10 |
Several patterns emerge from this comparison. The GLP-1 based peptides (semaglutide and tirzepatide) produce the most dramatic weight loss results but come with notable gastrointestinal side effects during titration. Growth hormone secretagogues offer a broader range of benefits beyond weight loss, making them attractive for women dealing with multiple menopausal symptoms simultaneously. And targeted approaches like AOD-9604 and tesamorelin provide focused fat reduction with minimal systemic effects. The peptide calculator for weight loss can help translate these general ranges into individualized dosing plans.
Your optimal choice depends on your primary goals, tolerance for side effects, existing health conditions, and whether you are using hormone replacement therapy concurrently. Many women ultimately find that a combination approach, using compounds from different mechanism categories, produces the best results. This leads us to the stacking strategies section.
Peptide stacking strategies for menopausal women
Single peptides work. Strategically combined peptides work better. The principle behind peptide stacking is straightforward: by targeting multiple metabolic pathways simultaneously, you create a synergistic effect that exceeds what any individual compound can achieve. For menopausal women dealing with disruptions across appetite regulation, fat metabolism, growth hormone production, and insulin sensitivity, a multi-pathway approach makes biological sense.
That said, more is not always better. Each peptide added to a stack increases complexity, potential interactions, and cost. The goal is to find the minimum effective combination that addresses your specific metabolic challenges.
The best peptide stack for weight loss depends entirely on individual circumstances, and the stacks below should be considered starting frameworks rather than rigid prescriptions. Use the peptide stack calculator to plan dosing for multi-compound protocols, and review the guide on combining multiple peptides for safety considerations.
Stack 1: GLP-1 foundation stack
This is the most straightforward and evidence-backed approach for menopausal weight loss. It combines the powerful appetite and insulin regulation of a GLP-1 agonist with growth hormone support for body composition optimization.
Components:
Tirzepatide (or semaglutide): Primary weight loss driver targeting appetite, insulin, and glucose metabolism
CJC-1295 with ipamorelin: Growth hormone support for lean mass preservation, sleep improvement, and additional fat oxidation
Rationale for menopausal women: The GLP-1 component addresses the insulin resistance and appetite dysregulation caused by estrogen decline, while the GH secretagogue preserves muscle mass that would otherwise be lost during caloric restriction. This is critical during menopause because muscle loss accelerates metabolically, creating a downward spiral of reduced metabolic rate and increased fat storage. The sleep-improving effects of the CJC-1295/ipamorelin component also help address the cortisol-weight gain cycle driven by menopausal sleep disruption.
Protocol overview: Tirzepatide is administered once weekly with standard titration starting at 2.5mg. CJC-1295 at 100 to 200 micrograms combined with ipamorelin at 100 to 200 micrograms is administered subcutaneously before bed, five days per week with two days off. The peptide dosing guide provides detailed instructions for managing multi-compound protocols, and the cycling guide covers how to structure on and off periods.
Expected timeline: Appetite suppression from tirzepatide begins within the first two weeks. Sleep improvements from CJC-1295/ipamorelin often appear within one to two weeks. Visible fat loss typically starts at weeks four to six, with significant body composition changes measurable by week ten to twelve.
Stack 2: Growth hormone optimization
This stack is designed for women who prefer to avoid GLP-1 agonists, whether due to gastrointestinal sensitivity, personal preference, or contraindications. It takes a different path to weight loss by optimizing the growth hormone axis and directly targeting fat metabolism.
Components:
Tesamorelin: Targeted visceral fat reduction through GHRH stimulation
AOD-9604: Direct fat metabolism stimulation without IGF-1 elevation
MOTS-C (optional): AMPK activation for mitochondrial metabolic support
Rationale for menopausal women: This combination attacks the fat storage problem from multiple angles without affecting appetite signaling. Tesamorelin specifically targets the visceral fat that accumulates during menopause, while AOD-9604 provides additional lipolytic support without the concerns of full growth hormone elevation. The optional addition of MOTS-C addresses the mitochondrial dysfunction that underlies menopausal metabolic slowdown. This stack is particularly well-suited for women whose primary concern is body composition rather than total scale weight, and who want to address the simultaneous goals of fat loss and muscle preservation.
Protocol overview: Tesamorelin at 2mg once daily in the morning. AOD-9604 at 300 to 500 micrograms once daily on an empty stomach, ideally 30 minutes before morning exercise. MOTS-C, if included, at 10mg injected subcutaneously two to three times per week. The peptide calculator helps determine precise dosing, and the injection guide covers proper administration techniques for multi-injection protocols.
Expected timeline: This stack works more gradually than GLP-1 based approaches. Initial changes in body composition may appear at weeks six to eight, with significant visceral fat reduction measurable by weeks twelve to sixteen. The results tend to build progressively over four to six months.
Stack 3: Comprehensive metabolic support
This is the most thorough approach, designed for women who want to address every aspect of menopausal metabolic disruption simultaneously. It is more complex and requires careful management, but the multi-pathway coverage offers the most comprehensive support available.
Components:
Semaglutide (or tirzepatide): Appetite regulation, insulin sensitivity, glucose metabolism
Tesamorelin: Targeted visceral fat reduction
MOTS-C: Mitochondrial function and AMPK activation
Rationale for menopausal women: This stack covers three distinct metabolic pathways. The GLP-1 component handles appetite and insulin signaling. Tesamorelin specifically targets the visceral fat compartment that menopause expands. And MOTS-C supports the mitochondrial energy production that estrogen decline impairs. Together, they address the metabolic trifecta of menopausal weight gain: disrupted appetite signaling, visceral fat accumulation, and cellular energy dysfunction.
This is not a beginner protocol. Women considering this stack should have experience with at least one peptide compound, understand proper reconstitution and storage procedures, and ideally work with a healthcare provider familiar with peptide protocols. Review the common peptide mistakes before beginning any advanced stack.
Protocols and dosing considerations
Getting the protocol right matters as much as choosing the right peptide. The precision approach to peptide dosing for weight loss requires attention to timing, titration, cycling, and individual response monitoring. This section covers the practical details that turn a good peptide selection into an effective weight loss protocol.
Starting your first peptide protocol
If you have never used peptides before, the preparation phase matters. Before your first injection, you need to understand reconstitution, bacteriostatic water preparation, proper injection technique, and storage requirements. These are not optional details. They directly affect whether your peptide works.
Start with one compound. Only one. The temptation to jump straight into a multi-peptide stack is understandable but counterproductive. Starting with a single peptide allows you to assess your individual response, identify any side effects, and establish a baseline before adding complexity. If you start three peptides simultaneously and develop a side effect, you have no way to identify which compound is responsible.
For most menopausal women, the recommended starting peptide depends on your primary goal. If total weight loss is the priority, begin with semaglutide or tirzepatide. If visceral fat is the specific concern, start with tesamorelin or AOD-9604. If you want broad metabolic and body composition support with sleep improvement, begin with CJC-1295 and ipamorelin. The getting started guide walks through the complete preparation process, and the injectable peptides overview helps you understand the landscape of available options.
Timing and administration
Timing affects results more than most people realize.
GLP-1 agonists like semaglutide and tirzepatide are administered once weekly, and the day of the week does not significantly matter. However, many users prefer to inject on a day when they can manage potential gastrointestinal effects, such as a weekend when nausea would be less disruptive. Some women find that taking their GLP-1 dose in the evening reduces next-day nausea compared to morning administration.
Growth hormone secretagogues, including CJC-1295 with ipamorelin and sermorelin, should be administered at bedtime on an empty stomach. Growth hormone release is suppressed by food intake, particularly carbohydrates and fats. Eating within 60 to 90 minutes of a GH secretagogue injection significantly blunts the growth hormone response. The nighttime dosing also capitalizes on the natural GH pulse that occurs during deep sleep stages.
AOD-9604 is most effective when administered in the morning, fasted, approximately 30 minutes before exercise. The fasted state and subsequent physical activity create a metabolic environment that maximizes the lipolytic effect of the peptide. If morning exercise is not feasible, administering on an empty stomach at any time of day still provides benefit, though the effect may be somewhat reduced.
The mixing guide covers preparation details, and understanding bacteriostatic water ratios ensures accurate dosing. The reconstitution calculator eliminates guesswork from the preparation process, and the injection pen guide offers an alternative to traditional syringe administration for those who prefer it.
Cycling strategies
Should you cycle your peptides? The answer depends on the compound.
GLP-1 agonists are typically used continuously rather than cycled. Stopping semaglutide or tirzepatide generally results in weight regain as appetite suppression is removed and metabolic adaptations reverse. Most medical protocols treat these as long-term medications rather than cyclical interventions. However, some practitioners recommend periodic dose reductions or "drug holidays" after reaching target weight to assess the body natural appetite regulation.
Growth hormone secretagogues are more commonly cycled. Standard cycles run 8 to 12 weeks on, followed by 4 to 6 weeks off. This cycling approach prevents pituitary desensitization, where the gland becomes less responsive to repeated stimulation. The cycle planning guide covers the rationale and logistics of different cycling approaches. Some protocols use a five-days-on, two-days-off weekly pattern within each cycle to maintain pituitary sensitivity.
AOD-9604 is typically run in 12-week cycles with 4-week breaks. Tesamorelin clinical trials used continuous 26-week protocols, but longer-term use may benefit from periodic reassessment. The cycling different peptides guide addresses the specific considerations for rotating between compounds and managing transitions between cycles.
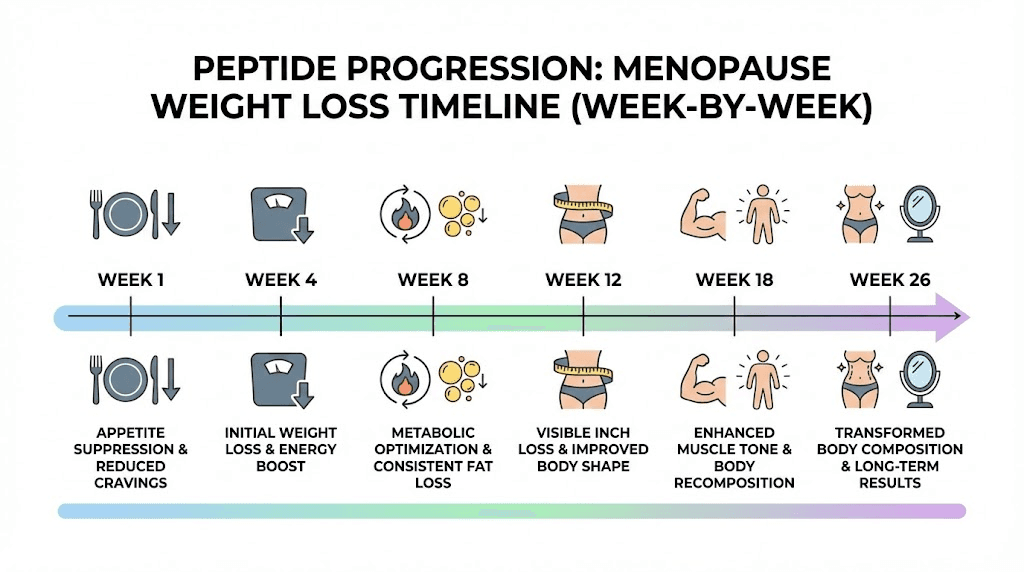
What to expect week by week
Setting realistic expectations prevents frustration and premature discontinuation. Here is a general timeline for the most common peptide approaches to menopausal weight loss, based on clinical data and consistent user reporting.
Weeks 1 to 2: With GLP-1 agonists, appetite reduction is usually noticeable within the first week. Food thoughts decrease. Portion sizes naturally shrink. Some gastrointestinal adjustment occurs, particularly nausea, which is usually mild and transient. With GH secretagogues, improved sleep quality is often the first noticeable effect, sometimes within three to five days. Weight may not change yet. This is normal.
Weeks 3 to 4: GLP-1 users typically see the first scale changes, usually 3 to 5 pounds, though individual variation is significant. GH secretagogue users may notice improved energy and skin quality. AOD-9604 users generally do not see visible changes yet but may notice subtle shifts in how clothes fit.
Weeks 5 to 8: This is where momentum builds. GLP-1 users are often down 8 to 15 pounds. GH secretagogue users start seeing measurable body composition changes, with waist circumference typically decreasing before scale weight changes significantly. Fat loss and lean mass preservation create a recomposition effect where the mirror shows changes that the scale may not fully reflect. The timeline guide provides detailed benchmarks across different peptide categories.
Weeks 9 to 12: GLP-1 users reach significant weight loss milestones. GH secretagogue users see cumulative body composition improvements. AOD-9604 users typically achieve noticeable visceral fat reduction. This is a good checkpoint for assessing whether to continue the current protocol, adjust doses, or add complementary compounds.
Weeks 13 to 26: Long-term results consolidate. GLP-1 users approach the 15 to 20 percent body weight reduction range. GH secretagogue users see continued improvements in body composition, sleep, and metabolic markers. The before and after results page showcases the kind of outcomes that become possible with sustained, well-managed protocols.
Why hormone therapy may enhance peptide results
The research on combining hormone replacement therapy with weight loss peptides in menopausal women is some of the most exciting data to emerge in recent studies. The synergy between estrogen replacement and peptide therapy is not just additive. It appears to be multiplicative, with each intervention amplifying the effectiveness of the other.
The Mayo Clinic data tells a powerful story. Women using tirzepatide combined with HRT achieved 17 percent weight loss compared to 14 percent with tirzepatide alone. That three percentage point difference might seem modest on paper. But translate it into practical terms: for a 180-pound woman, the HRT combination produces an additional 5.4 pounds of weight loss. More strikingly, 45 percent of women in the combination group achieved the 20 percent weight loss threshold compared to only 18 percent without HRT. That is a 2.5-fold increase in the likelihood of achieving a transformative weight loss outcome.
Similar patterns emerged with semaglutide. Postmenopausal women combining HRT with semaglutide achieved approximately 30 percent more weight loss than those using semaglutide alone.
The mechanism behind this synergy makes biological sense. Estrogen replacement partially restores the metabolic infrastructure, including insulin sensitivity, fat oxidation capacity, and mitochondrial function, that allows peptides to work more effectively. Think of it like upgrading the operating system before running new software. The software (peptide) works either way, but the upgraded operating system (restored estrogen) allows it to perform at a higher level.
This does not mean that HRT is required for peptides to work. The clinical trials clearly show significant weight loss with peptides alone. But for women who are candidates for HRT and are considering peptide therapy for weight loss, the combination data strongly favors using both. The menopause peptide guide and the perimenopause peptide guide provide additional context on how hormone-balancing peptides interact with HRT protocols.
One important caveat. HRT decisions should be made with a qualified healthcare provider who can assess individual risk factors, including breast cancer history, cardiovascular risk, and clotting disorders. The weight loss benefits of combining HRT with peptides are compelling, but they must be weighed against the individual risk profile that every menopausal woman carries.
Lifestyle factors that amplify peptide effectiveness
Peptides are not magic. They are powerful tools that work best within a supportive metabolic environment. The lifestyle factors discussed below do not just "help a little." They can multiply the effectiveness of any peptide protocol by two to three times, or they can undermine even the best peptide stack if neglected. SeekPeptides consistently emphasizes that peptide protocols produce their best results when integrated into a comprehensive approach to metabolic health.
Exercise strategies during menopause
Exercise during menopause requires a different approach than what worked before. The two most important adaptations are increased emphasis on resistance training and strategic use of high-intensity intervals.
Resistance training is non-negotiable. Menopausal women lose muscle mass at an accelerated rate, and muscle tissue is the primary driver of resting metabolic rate. Every pound of muscle lost means approximately 6 to 10 fewer calories burned per day at rest. Over years, that adds up. Resistance training three to four times per week, focusing on compound movements like squats, deadlifts, rows, and presses, preserves and builds the metabolic tissue that keeps your calorie burn elevated. This is especially important when using GLP-1 agonists, which can cause lean mass loss alongside fat loss if exercise is not incorporated.
High-intensity interval training (HIIT) two to three times per week provides metabolic benefits that steady-state cardio cannot match. HIIT increases MOTS-C production by up to 11.9 times in muscle tissue, activates AMPK pathways, and creates an "afterburn" effect that elevates metabolism for hours after the session. For women using MOTS-C as part of their peptide protocol, exercise essentially amplifies the same pathway the peptide targets. The synergy between exercise-induced and supplemental MOTS-C activation is a compelling reason to incorporate HIIT into any menopausal performance protocol.
Walking remains underrated. A daily 30 to 45 minute walk, particularly after meals, improves glucose disposal and insulin sensitivity in ways that complement GLP-1 agonist therapy. Post-meal walking can reduce blood sugar spikes by 30 to 50 percent, enhancing the glucose-regulating effects of semaglutide or tirzepatide.
Nutrition and macronutrient balance
Protein intake becomes critically important during menopause, and even more so when using peptides for weight loss. The standard recommendation of 0.8 grams per kilogram of body weight is inadequate for menopausal women trying to preserve lean mass during fat loss. Research supports 1.2 to 1.6 grams per kilogram, with some experts recommending up to 2.0 grams per kilogram during active weight loss phases.
Why this matters with peptides: GLP-1 agonists reduce appetite significantly. If total food intake drops but protein intake is not deliberately maintained, the body will catabolize muscle tissue for amino acids. This defeats the metabolic purpose of the entire protocol. Prioritizing protein at every meal ensures that the caloric deficit created by appetite suppression comes primarily from fat stores rather than lean tissue.
The question of collagen peptides for weight loss comes up frequently. Collagen peptides provide protein but lack certain essential amino acids that complete proteins contain. They can supplement total protein intake but should not replace complete protein sources like meat, fish, eggs, and dairy. For menopausal women, collagen does offer additional benefits for skin, joint, and bone health, making it a reasonable addition rather than a replacement for standard protein sources.
Carbohydrate timing also matters, particularly for women using growth hormone secretagogues. Avoiding carbohydrates for 60 to 90 minutes before and after GH secretagogue administration prevents the insulin spike that suppresses growth hormone release. Some women find that a moderate-carbohydrate approach, with total carbohydrate intake around 100 to 150 grams daily timed primarily around exercise, optimizes both peptide effectiveness and menopausal symptom management.
Sleep optimization
Sleep is not just recovery time. It is an active metabolic process that directly determines how effectively your peptides work.
Growth hormone secretagogues specifically require quality sleep to deliver their full benefit. The primary GH pulse occurs during stage 3 deep sleep, and if sleep architecture is disrupted by hot flashes, night sweats, or anxiety, the GH response to secretagogues is blunted. Addressing sleep quality is not a bonus strategy. It is a prerequisite for getting the most from your investment in GH-based peptides.
Practical sleep optimization for menopausal women includes keeping the bedroom temperature at 65 to 68 degrees Fahrenheit, using moisture-wicking bedding, maintaining consistent sleep and wake times even on weekends, limiting screen exposure for 60 minutes before bed, and considering sleep-supporting peptides if menopausal sleep disruption is severe. The relationship between sleep quality and weight loss is bidirectional: better sleep improves weight loss outcomes, and weight loss (particularly visceral fat reduction) often improves sleep quality.
Stress management
Cortisol is the silent saboteur of menopausal weight loss. Chronic stress elevates cortisol, which promotes visceral fat storage, breaks down muscle tissue, increases appetite for high-calorie foods, and impairs insulin sensitivity. Every one of these effects directly counteracts what weight loss peptides are trying to accomplish.
The stress management strategies that matter most for menopausal metabolic health are those that reduce cortisol output consistently rather than episodically. Daily practices like 10 to 15 minutes of meditation, regular social connection, nature exposure, and deliberate breathing exercises produce measurable cortisol reductions over time. The anxiety management peptides and mood support peptides offer additional pharmacological options for women whose stress response is significantly impacting their metabolic health and weight loss efforts.
Safety considerations and side effects
No responsible discussion of peptide safety glosses over side effects. Every compound on this list carries potential adverse effects that deserve honest assessment. Understanding the side effect profile of each peptide helps you make informed decisions, recognize problems early, and manage issues effectively if they arise. SeekPeptides prioritizes safety information because informed researchers make better decisions and achieve better outcomes.
Common side effects by peptide
Semaglutide and tirzepatide: Gastrointestinal effects dominate the side effect profile. Nausea is the most common, affecting 30 to 50 percent of users, particularly during dose titration. Vomiting, diarrhea, constipation, and abdominal discomfort are also reported. Most GI side effects are dose-dependent and improve with time at each dose level. Slow titration, eating smaller meals, and avoiding high-fat foods can significantly reduce GI symptoms. Less common but more serious concerns include pancreatitis (rare but reportable), gallbladder issues, and potential thyroid C-cell tumor risk seen in rodent studies. The benefits and risks guide provides a comprehensive overview.
AOD-9604: The side effect profile is remarkably mild. Injection site reactions are the primary complaint. Headache and mild flu-like symptoms are occasionally reported during initial use but typically resolve within the first week. No significant metabolic, hormonal, or cardiovascular side effects have been identified in clinical studies.
CJC-1295 with ipamorelin: Water retention and mild joint stiffness can occur, particularly at higher doses, reflecting the growth hormone elevation. These effects are usually dose-dependent and resolve with dose reduction. Tingling or numbness in extremities (carpal tunnel-like symptoms) has been reported. Flushing and head rush immediately after injection of ipamorelin occur in some users but are transient, lasting minutes. The ipamorelin side effects guide covers management strategies in detail.
Tesamorelin: Injection site reactions, including redness, itching, and pain, are common. Joint pain (arthralgia) affects approximately 10 to 15 percent of users. Peripheral edema (swelling in hands and feet) can occur. Glucose metabolism may be affected, making regular blood sugar monitoring important, particularly for menopausal women already dealing with insulin resistance changes.
MOTS-C: Limited safety data exists from human studies. Based on available research, the compound appears well-tolerated. Injection site reactions are the primary reported side effect. However, the preclinical status means the full human side effect profile is not yet established. Review the MOTS-C side effects page for the most current safety information available.
Sermorelin: Generally well-tolerated. Injection site pain or redness is the most common complaint. Facial flushing and headache can occur initially. At higher doses, the same GH-related effects seen with CJC-1295 (water retention, joint stiffness) may appear but are typically mild.
Contraindications
Several conditions require careful consideration or may preclude peptide use entirely.
Active cancer or history of certain cancers is a contraindication for growth hormone secretagogues (CJC-1295, ipamorelin, tesamorelin, sermorelin), as elevated GH and IGF-1 can promote tumor growth. GLP-1 agonists carry a specific warning regarding medullary thyroid carcinoma risk based on rodent data, and personal or family history of this cancer type is a contraindication.
Type 1 diabetes requires extreme caution with GLP-1 agonists due to hypoglycemia risk. Active pancreatitis or history of recurrent pancreatitis is a contraindication for semaglutide and tirzepatide. Pregnancy is a contraindication for all compounds on this list. The legal status and regulatory landscape of these compounds varies by jurisdiction and should be understood before beginning any protocol.
For menopausal women specifically, interactions with hormone replacement therapy should be discussed with a healthcare provider, as both HRT and certain peptides affect metabolic and hormonal pathways. While the combination data is encouraging, individual risk factors need professional assessment.
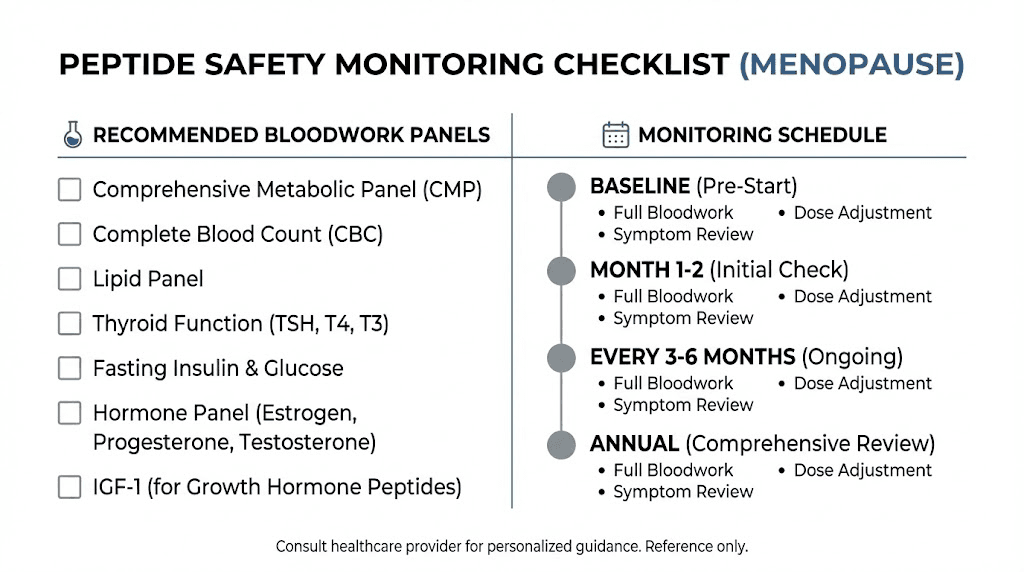
Monitoring and bloodwork
Baseline bloodwork before starting any peptide protocol is not optional. It is essential for safety monitoring and for measuring progress objectively.
The recommended baseline panel for menopausal women considering weight loss peptides includes: fasting glucose and HbA1c (metabolic baseline), fasting insulin (insulin resistance assessment), lipid panel including triglycerides (cardiovascular risk), complete metabolic panel (liver and kidney function), IGF-1 (baseline for GH secretagogue monitoring), thyroid panel including TSH and free T4, estradiol and FSH (menopausal status confirmation), and DEXA scan if available (body composition baseline).
Follow-up bloodwork should occur at 8 to 12 weeks after starting therapy, then quarterly during ongoing use. For GH secretagogues specifically, IGF-1 levels should be monitored to ensure they remain within the physiological range. For GLP-1 agonists, periodic pancreatic enzyme levels (lipase, amylase) provide early warning of potential pancreatic issues. The testing labs guide helps you find appropriate testing facilities, and understanding therapy costs includes budgeting for regular monitoring.
Additional compounds worth considering
Beyond the seven primary peptides discussed above, several other compounds deserve mention in the context of menopausal metabolic support. While they may not be primary weight loss agents, they address related aspects of menopausal health that influence body composition and metabolic function.
5-Amino-1MQ is a small molecule that inhibits NNMT (nicotinamide N-methyltransferase), an enzyme involved in fat cell metabolism. By blocking NNMT, it promotes fat cell energy expenditure and reduces fat accumulation. Research suggests it may be particularly relevant for visceral fat, making it a potential complementary agent for menopausal weight management.
Tesofensine works through a different mechanism entirely, inhibiting the reuptake of serotonin, dopamine, and noradrenaline. This triple-reuptake inhibition produces appetite suppression and increased metabolic rate. Clinical trials showed significant weight loss, though cardiovascular effects require careful monitoring.
The lipotropic peptides guide and the Lipo-C peptide overview cover additional fat metabolism support compounds that some women incorporate into comprehensive protocols. And for those interested in the newest generation of weight management peptides, cagrilintide and retatrutide represent emerging options with promising early data. The cagrilintide dosing protocols are still being established, but the mechanism of action, targeting amylin receptors for appetite regulation, offers a novel pathway distinct from GLP-1 agonism.
Women exploring these options should also understand the broader context of peptide applications and how weight management fits into the larger picture of menopausal health optimization. Compounds like energy-supporting peptides and endurance peptides can indirectly support weight loss by enabling more consistent exercise programs. And energy and focus peptides help address the brain fog and fatigue that often accompany menopause and sabotage diet compliance.
Peptide quality and sourcing
The effectiveness of any peptide protocol depends on starting with a quality product. This section deserves attention because the peptide market includes products of vastly varying quality, and using a degraded, contaminated, or underdosed peptide will produce poor results regardless of how perfect your protocol is.
The vendor evaluation guide covers the criteria for assessing peptide suppliers, including third-party testing, purity standards, and transparent certificate of analysis documentation. The testing labs guide explains how to verify the quality and purity of peptides you receive. Understanding the difference between research grade and pharmaceutical grade peptides is essential for setting appropriate expectations about purity, potency, and consistency.
Proper storage is equally important. Peptides are fragile molecules that degrade when exposed to heat, light, moisture, and contamination. The storage guide covers requirements for both lyophilized powder and reconstituted solutions. Knowing refrigerator shelf life and reconstituted stability timelines prevents potency loss. And understanding peptide expiration helps you avoid using degraded product. The difference between lyophilized and liquid peptides and between injectable and oral forms also affects how you handle storage and administration. For some women, nasal spray peptides or peptide capsules may offer more convenient administration routes, though bioavailability differs from injectable forms.
The broader picture of menopausal health
Weight loss does not happen in isolation. Menopausal women often deal with a constellation of symptoms that interact with and influence body composition outcomes. Addressing these related concerns can indirectly but meaningfully improve weight loss results.
Bone health is a critical consideration, particularly when combining caloric restriction with menopause. Weight-bearing exercise and adequate calcium and vitamin D intake become even more important when using weight loss peptides. Some growth hormone secretagogues may support bone density, providing an additional benefit beyond fat loss. Joint health is also relevant, as excess weight compounds the joint pain that many menopausal women experience. Joint-supporting peptides like BPC-157 can help women maintain the exercise program needed to support weight loss when joint issues threaten to sideline them.
Skin changes during menopause, including loss of collagen, elasticity, and hydration, can be exacerbated by rapid weight loss. Skin-supporting peptides and skin tightening compounds like GHK-Cu can address the cosmetic concerns that sometimes accompany significant weight loss during menopause. Collagen peptides offer additional dermatological support.
Inflammation plays a role in both menopausal symptoms and weight management. Visceral fat itself is an inflammatory tissue, and reducing it through peptide therapy can decrease systemic inflammation markers. Conversely, anti-inflammatory peptides like KPV may support the metabolic environment by reducing the inflammatory burden that contributes to insulin resistance. The inflammation peptides guide provides a thorough overview of this interconnection.
For women dealing with the libido changes and mood shifts that often accompany menopause, addressing these symptoms can indirectly support weight loss adherence and overall quality of life. The libido peptides guide covers options that some women find helpful. Similarly, the longevity peptide and anti-aging peptide categories overlap significantly with menopausal health optimization, as many of the same compounds that support healthy aging also address menopausal metabolic disruption. The anti-aging peptide category page provides an organized overview of these options.
Even hair health and hair growth peptides intersect with menopausal weight management, as both hair thinning and weight gain share underlying hormonal drivers. Addressing the root hormonal imbalances often improves multiple symptoms simultaneously. The safe peptides for women guide and the best peptides for women overview help navigate the full spectrum of options with female-specific considerations front and center.
Accessing peptide therapy
The practical question of how to access these treatments deserves honest discussion. Peptide therapy online has expanded access significantly, with telemedicine platforms offering consultations, prescriptions, and delivery for compounds like semaglutide, tirzepatide, and various growth hormone secretagogues. The cost of peptide therapy varies widely depending on the specific compound, source, and whether insurance coverage applies. The peptide cost calculator helps estimate expenses across different protocols and durations.
Understanding the legal landscape for each compound is important. Semaglutide and tirzepatide are FDA-approved prescription medications. Tesamorelin is FDA-approved for a specific indication. Other compounds on this list fall under the research peptide category and have different regulatory frameworks. The regulation updates page tracks changes in the legal landscape that affect access and availability.
For women serious about optimizing their menopause weight loss peptide protocols, SeekPeptides provides comprehensive resources including protocol builders, dosing calculators, safety databases, and an engaged community of researchers who have navigated these exact decisions. Making informed choices about peptide therapy requires access to accurate, up-to-date information, and that is precisely what SeekPeptides was built to provide.
Frequently asked questions
What is the best peptide for menopause belly fat specifically?
Tesamorelin has the strongest clinical evidence for visceral fat reduction specifically, with FDA-approved data showing 15 to 20 percent reduction over 26 weeks. Tirzepatide produces the most dramatic total weight loss, which includes abdominal fat. For targeted belly fat without appetite effects, the combination of tesamorelin with AOD-9604 addresses visceral fat through dual mechanisms. The belly fat peptide guide covers this topic in depth.
Can I use weight loss peptides if I am on hormone replacement therapy?
Not only can you, the research suggests you may want to. Mayo Clinic data shows that combining HRT with GLP-1 agonists produces 30 to 35 percent more weight loss than GLP-1 agonists alone. The combination of tirzepatide with HRT showed 45 percent of women achieving 20 percent weight loss versus only 18 percent without HRT. Discuss the specific combination with your healthcare provider to ensure compatibility with your HRT formulation and individual health profile. The menopause peptide resource covers this interaction extensively.
How long do I need to stay on peptides for weight loss?
GLP-1 agonists typically require ongoing use to maintain weight loss, as stopping usually results in gradual weight regain over 6 to 12 months. Growth hormone secretagogues are typically cycled in 8 to 12 week blocks with breaks. AOD-9604 runs in 12-week cycles. The cycle planning guide and results timeline guide provide specific protocols for each compound. Ultimately, the goal should be to establish lifestyle habits that support weight maintenance if or when peptide use is discontinued.
Are peptides safe for women over 50?
The safety data for most peptides discussed here does not show age-dependent increases in adverse effects for women over 50. Semaglutide and tirzepatide clinical trials included significant numbers of postmenopausal women with acceptable safety profiles. However, older women may need more conservative dose titration, more frequent monitoring, and careful attention to drug interactions with other medications. The safe peptides for women guide addresses age-specific safety considerations.
Will peptides cause muscle loss during menopause weight loss?
GLP-1 agonists can contribute to lean mass loss alongside fat loss if resistance training and adequate protein intake are not maintained. This risk is heightened during menopause when muscle preservation is already challenged by hormonal changes. Growth hormone secretagogues actually help preserve lean mass, which is why combining a GLP-1 agonist with CJC-1295/ipamorelin is a strategic approach. The weight loss and muscle gain guide covers strategies for maintaining muscle during peptide-assisted fat loss. Resistance training three to four times weekly and protein intake of 1.2 to 1.6 grams per kilogram are essential protective measures.
What is the most cost-effective peptide for menopause weight loss?
AOD-9604 and sermorelin tend to be the most affordable options on a per-month basis. GLP-1 agonists (semaglutide, tirzepatide) are the most expensive but also produce the most dramatic results, making the cost-per-pound-lost ratio competitive. Use the peptide cost calculator to compare monthly expenses across different compounds and protocols. The sermorelin cost analysis provides a detailed breakdown of expenses for that specific compound.
Can I combine peptides with other supplements for menopause?
Many women successfully combine weight loss peptides with supplements like vitamin D, omega-3 fatty acids, magnesium, and adaptogenic herbs. However, some supplements can interact with peptide mechanisms. For example, high-dose biotin supplementation can interfere with certain lab tests used to monitor peptide therapy. And some herbal supplements affect liver metabolism in ways that could influence peptide clearance. Discuss your full supplement regimen with your healthcare provider. The immune support peptide guide covers compounds that complement weight management protocols.
Do I need a prescription for these peptides?
Semaglutide, tirzepatide, and tesamorelin are prescription medications in most jurisdictions and require a healthcare provider consultation. Other compounds like AOD-9604, CJC-1295, ipamorelin, and MOTS-C fall into the research peptide category in many countries, with varying regulatory requirements. The legal status guide and regulation update tracker provide current information on the legal landscape for each compound.
External resources
For women navigating the complex intersection of menopause and weight management, SeekPeptides offers the most comprehensive resource available. Evidence-based guides, proven protocols, community support from thousands of experienced researchers, and tools like the peptide calculator and stack calculator make the difference between guessing and knowing. The right peptide, at the right dose, with the right protocol, can transform the menopausal weight loss experience from frustrating to manageable.
In case I do not see you, good afternoon, good evening, and good night. May your metabolism stay resilient, your protocols stay precise, and your midlife transformation stay exactly on track.



