Jan 23, 2026
Of the thousands of women who try peptide therapy for fat loss, fewer than one in four get the results they hoped for. The peptide itself is rarely the problem. The real issue? Wrong peptide selection. Wrong timing. Wrong expectations. And a fundamental misunderstanding of how female metabolism actually works.
This guide changes that.
Female physiology is uniquely sensitive to hormonal shifts that affect appetite, metabolism, cravings, sleep, and where the body stores fat. This is why many women see better results with peptides compared to traditional dieting alone. But the gap between mediocre and exceptional outcomes often comes down to details most guides completely ignore.
Here you will find everything that matters about peptides for weight loss as a woman. The mechanisms that make certain peptides work better for female bodies. The dosing protocols that clinical research actually supports. The stacking strategies that amplify results without amplifying risk. And the honest truth about what to expect, when to expect it, and what realistic fat loss looks like when you are doing everything right.
SeekPeptides has helped thousands of women navigate peptide protocols with evidence-based guidance. What follows represents the most comprehensive resource available for women serious about using peptides safely and effectively.
Why female fat loss is fundamentally different
The weight loss industry treats women like smaller men. It is a costly mistake. Female metabolism operates on entirely different rules, shaped by hormonal rhythms that influence everything from appetite to fat storage patterns to how efficiently calories convert to energy.
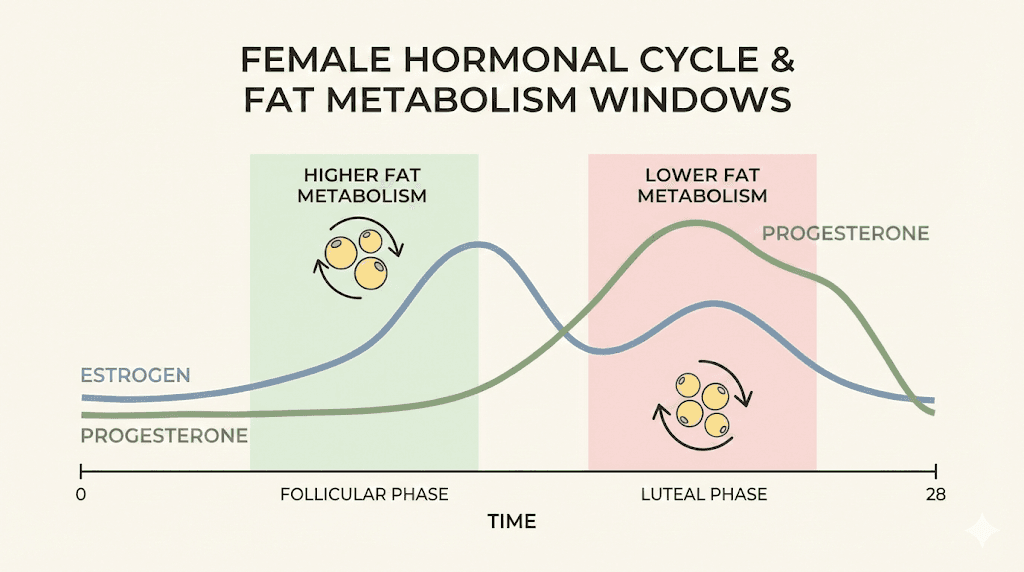
Estrogen and progesterone fluctuate throughout the menstrual cycle, creating predictable windows where fat loss becomes easier and others where the body resists letting go of stored energy. During the follicular phase, estrogen rises and insulin sensitivity improves. During the luteal phase, progesterone dominates and the body holds water, cravings intensify, and metabolic rate actually increases slightly, though this rarely translates to easier fat loss.
Then there is perimenopause and menopause. As estrogen declines, visceral fat accumulation increases. The protective effects that kept fat away from the midsection fade. Insulin resistance creeps in. Sleep quality deteriorates. And the metabolic changes during perimenopause make traditional dieting approaches progressively less effective.
This is where peptides become particularly valuable for women.
Peptide therapy works with female physiology rather than against it. The right peptides address the specific mechanisms that make female fat loss challenging: appetite regulation, insulin sensitivity, growth hormone production, and metabolic flexibility. They create hormonal environments conducive to fat burning without the muscle loss that accompanies most caloric deficits.
Understanding these differences is not optional. It is foundational to getting results.
The peptide categories that actually work for women
Not all peptides produce meaningful weight loss. Many promoted online have minimal clinical evidence. Others work but carry risks that outweigh benefits for most women. The peptides worth considering fall into distinct categories, each with different mechanisms, timelines, and expected outcomes.
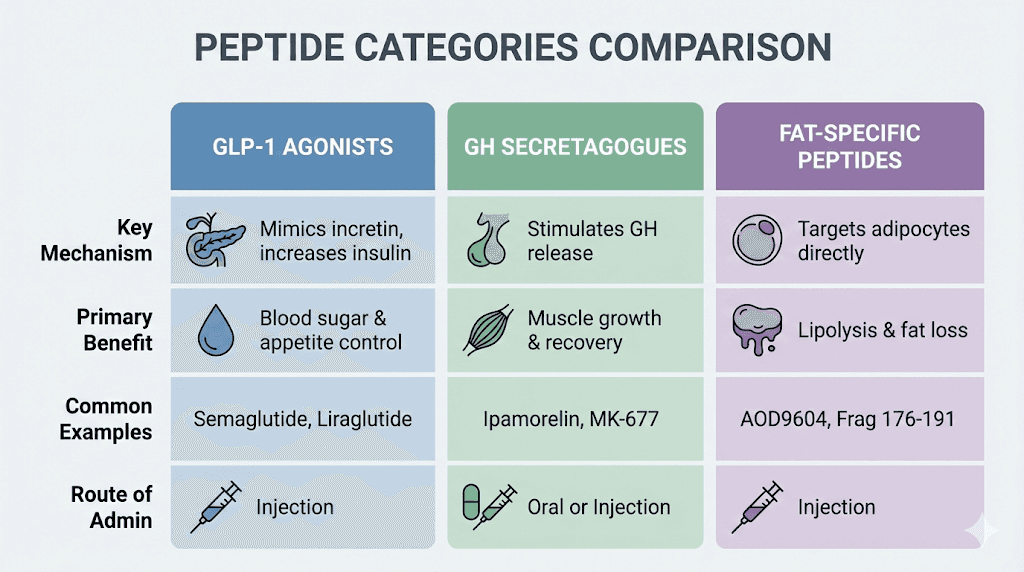
GLP-1 receptor agonists: the clinical heavyweights
Semaglutide and tirzepatide represent the most studied, most effective peptides for weight loss currently available. These are not research chemicals with uncertain outcomes. These are FDA-approved medications with extensive clinical trial data specifically in populations that include women.
The SURMOUNT-5 clinical trial published in the New England Journal of Medicine compared tirzepatide directly against semaglutide in adults with obesity but without type 2 diabetes. At 72 weeks, tirzepatide produced 20.2% mean weight loss compared to 13.7% with semaglutide. Both medications produced clinically meaningful results, but tirzepatide consistently outperformed across studies.
The SHAPE study, a real-world analysis of 9,916 patients with roughly 80% being female, found 14.1% weight loss with semaglutide and 16.5% with tirzepatide after one year. These numbers matter because they come from actual patients in clinical practice, not just controlled trial environments.
Semaglutide works by mimicking GLP-1, a hormone that regulates appetite and blood sugar. It reduces hunger, increases satiety, and slows gastric emptying. Women often report that the constant food noise in their heads simply quiets. Cravings diminish. The psychological battle with food becomes manageable.
Tirzepatide goes further. It activates both GLP-1 and GIP receptors, creating dual metabolic support. This dual mechanism appears to explain its superior weight loss results. Clinical trials show 16-22.5% body weight reduction after 72 weeks when combined with lifestyle changes, making it the most effective FDA-approved option available.
Both require weekly subcutaneous injections and medical supervision. Both carry gastrointestinal side effects, particularly during dose escalation.
And both require a prescription.
Growth hormone secretagogues: the metabolic optimizers
Growth hormone declines with age. By 40, most women produce significantly less than they did at 25. This decline contributes to increased body fat, reduced muscle mass, decreased energy, and slower recovery. Growth hormone secretagogues stimulate your own body to produce more GH rather than introducing synthetic growth hormone directly.
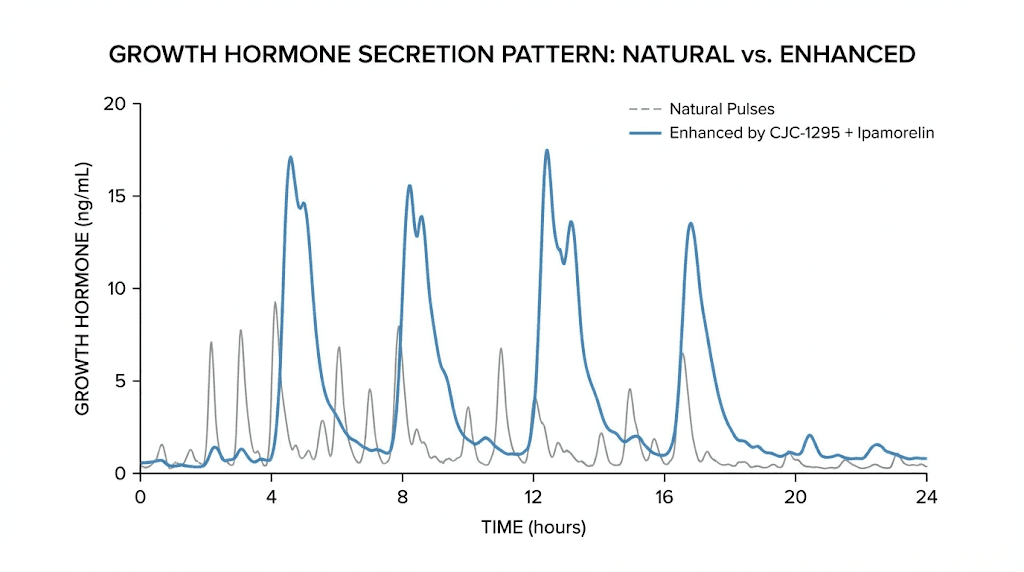
CJC-1295 combined with ipamorelin has become one of the most popular peptide protocols for women looking to enhance body composition. CJC-1295 stimulates the pituitary gland to release more growth hormone over an extended period. Ipamorelin works on the ghrelin receptor to increase GH release without significantly impacting cortisol or prolactin levels.
Together, they create a 3-5 fold increase in growth hormone release compared to ipamorelin alone. This translates to enhanced fat metabolism, particularly in stubborn areas like hips, thighs, and abdomen. It also means better sleep, improved recovery, and preserved muscle mass during caloric deficits.
The combination is particularly valuable for women entering perimenopause or menopause. It promotes physiological GH release that improves body composition, sleep quality, and skin health. It encourages gradual, natural fat loss rather than dramatic weight swings. And it supports collagen synthesis, which addresses multiple concerns simultaneously.
Tesamorelin deserves special attention. It is a synthetic analog of growth hormone-releasing hormone specifically designed to reduce deep visceral abdominal fat. In clinical trials, participants saw VAT reductions of roughly 15-20% over 26 weeks. It is FDA-approved for HIV-associated lipodystrophy, but specialty medicine settings increasingly use it off-label for women with significant visceral adiposity.
The catch? Most clinical research enrolled predominantly male participants. The results may not directly translate to female physiology. Medical supervision and regular monitoring become especially important.
Fat-specific peptides: targeted approaches
AOD-9604 is a synthetic peptide derived from a fragment of human growth hormone, specifically amino acids 177-191. It was designed to replicate the fat-burning effects of growth hormone without the other physiological impacts. The theory was sound. The reality proved more complicated.
In a 12-week randomized clinical trial, subjects receiving AOD-9604 at 1 mg daily lost an average of 2.6 kg compared to 0.8 kg in the placebo group. A 23-week trial showed 2.8 kg weight reduction. However, development was terminated in 2007 when a larger 24-week trial with 536 subjects failed to demonstrate statistically significant weight loss.
Does it work? Results vary among individuals. Lifestyle factors like diet, exercise, sleep quality, and stress levels play significant roles. If nutrition is unbalanced and activity levels are low, AOD-9604 likely will not deliver dramatic results. Combined with a structured, high-protein diet and consistent training, it may enhance fat-loss efforts, particularly during body recomposition phases.
Standard dosing ranges from 300-500 mcg daily, administered via subcutaneous injection. Research showed that higher doses did not produce additional benefits over the 1 mg daily dose, suggesting a ceiling effect.
MOTS-C operates through entirely different mechanisms. It is a mitochondrial-derived peptide that increases insulin sensitivity and promotes fatty acid oxidation. Unlike most peptides encoded in nuclear DNA, MOTS-C originates within mitochondria, offering unique metabolic effects at the cellular energy level.
For women specifically, MOTS-C shows promise. Research demonstrates that MOTS-C administration prevents ovariectomy-induced obesity and insulin resistance in mice via the AMPK pathway. This is particularly relevant for postmenopausal women who exhibit weight gain, changes in fat distribution, and deteriorating insulin sensitivity. The decline in MOTS-C may be blunted in premenopausal women due to estrogen's protective effects. The loss of this compensatory mechanism may contribute to fat accumulation and insulin resistance that commonly accompanies menopause.
MOTS-C also promotes osteoblast proliferation, differentiation, and mineralization. For women at high risk of developing osteoporosis, this represents a significant secondary benefit.
Semaglutide: the most studied option for female fat loss
Semaglutide deserves detailed examination because it has the most extensive clinical evidence supporting its use in women specifically. Understanding exactly how it works, what to expect, and how to use it optimally separates successful outcomes from disappointing ones.
Mechanism of action
Semaglutide is a glucagon-like peptide-1 receptor agonist. GLP-1 is a hormone your body naturally produces in response to food intake. It signals the brain to reduce appetite, tells the pancreas to release insulin, and slows how quickly food leaves your stomach.
Semaglutide amplifies these effects. It binds to GLP-1 receptors in the hypothalamus, the brain region controlling hunger and satiety. It reduces activity in reward centers that respond to food cues. The result is genuine reduction in appetite rather than white-knuckling through cravings.
For women specifically, this addresses a fundamental challenge. Female hormones create appetite fluctuations that make consistent caloric restriction difficult. The luteal phase brings increased cravings. Stress triggers emotional eating. Sleep deprivation amplifies hunger hormones. Semaglutide provides a buffer against these fluctuations, making adherence to nutrition plans dramatically easier.
Clinical evidence in women
The STEP trials established semaglutide's efficacy. In the STEP-1 trial, patients without type 2 diabetes achieved mean weight loss of 14.9% at 68 weeks. The SHAPE real-world study found that among 6,794 patients on semaglutide 2.4 mg, approximately 80% were female, with mean weight loss of 14.6 kg and 14.1% body weight reduction after one year.
These are not modest results.
A woman starting at 200 pounds could expect to lose roughly 28 pounds over a year, assuming typical response and adherence. Individual variation exists, of course. Some respond exceptionally well. Others see more modest results. But the average outcomes exceed what most achieve through diet and exercise alone.
A recent post hoc analysis of clinical trials found that female participants achieved composite endpoints (HbA1c below 6.5% and weight loss target of 10% or greater) at higher rates than male participants. Women may actually respond better to GLP-1 therapy than men.
Dosing protocol
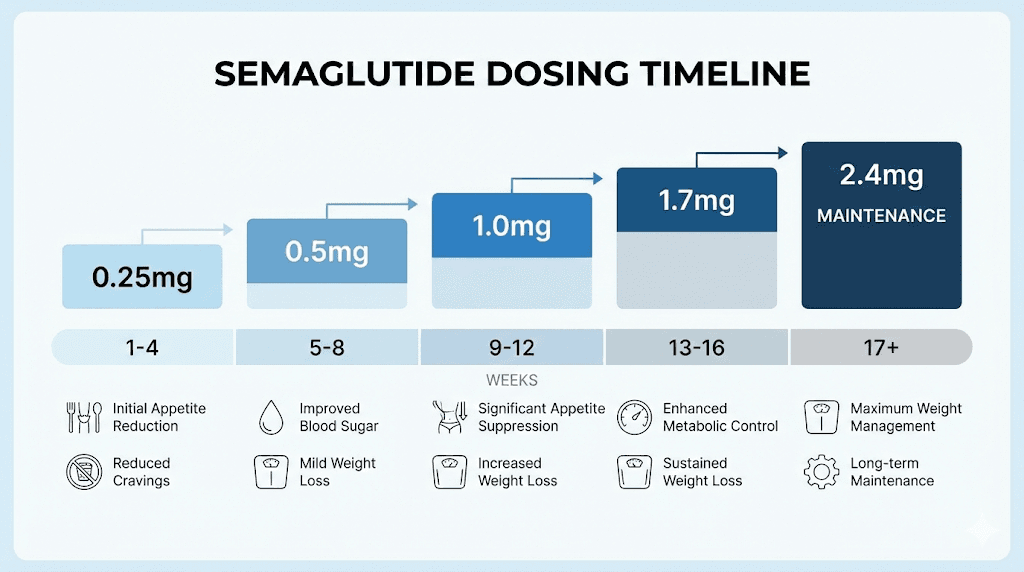
Semaglutide requires careful dose titration to minimize gastrointestinal side effects. Starting too high or escalating too quickly leads to nausea, vomiting, and premature discontinuation.
The standard approach begins at 0.25 mg weekly for four weeks. This dose typically produces minimal weight loss but allows the body to adjust. After four weeks, increase to 0.5 mg weekly. Continue monthly escalations through 1 mg, 1.7 mg, and finally 2.4 mg as tolerated.
Many women find their optimal dose before reaching 2.4 mg. If appetite suppression is adequate and weight loss progresses at 1 mg or 1.7 mg, forcing higher doses serves no purpose and may increase side effects.
The semaglutide dosage calculator can help determine appropriate starting points based on your specific situation.
What to expect and when
Week one through four: minimal changes. You may notice slightly reduced appetite, particularly in the evenings. Some women report food simply being less interesting. Mild nausea is common but usually manageable.
Weeks four through eight: appetite suppression becomes more noticeable. Portions that previously seemed normal now feel excessive. Cravings, particularly for high-carbohydrate foods, diminish. The scale typically starts moving.
Weeks eight through sixteen: weight loss accelerates for most. Energy levels often improve despite lower caloric intake. Sleep may improve. Body composition changes become visible, though the scale remains the primary measure.
Months four through twelve: weight loss continues but may slow as the body adapts. This is normal and expected. Total weight loss depends on starting weight, dose reached, and lifestyle factors.
Managing side effects
Gastrointestinal effects are the primary concern. Nausea affects roughly 40% of users, particularly during dose escalation. It typically resolves within days to weeks at each dose level. Eating smaller meals, avoiding fatty foods, and staying hydrated help.
Constipation affects some women. Adequate fiber intake and hydration address this for most. Proper hydration becomes especially important on GLP-1 therapy.
Delayed gastric emptying can reduce absorption of oral medications. If you take other medications, discuss timing with your healthcare provider.
The FDA cautions that semaglutide may not be suitable during pregnancy. Women of reproductive age should discontinue use at least two months before a planned pregnancy.
Tirzepatide: the dual-action powerhouse
Tirzepatide represents the next evolution in peptide therapy for weight loss. It consistently outperforms semaglutide in head-to-head trials, producing the highest average weight loss of any FDA-approved medication to date.
Dual mechanism explained
Unlike semaglutide, which targets only GLP-1 receptors, tirzepatide activates both GLP-1 and GIP receptors simultaneously. GIP stands for glucose-dependent insulinotropic polypeptide, another incretin hormone that influences metabolism.
This dual action creates enhanced effects on appetite, glucose control, and fat metabolism. The synergy appears to explain the superior weight loss results. Two metabolic pathways working together produce outcomes neither achieves alone.
For women, this dual mechanism may be particularly advantageous. Female metabolism involves complex hormonal interplay. Having multiple metabolic levers to pull creates more opportunities for the body to shift into fat-burning mode.
Clinical results women should know
The SURMOUNT-1 trial established tirzepatide's remarkable efficacy. Patients without type 2 diabetes achieved mean weight loss of 15.0% with the 5 mg dose, 19.5% with 10 mg, and 20.9% with 15 mg at 72 weeks.
These numbers exceed what most bariatric surgeries achieve.
The SURMOUNT-5 trial directly compared tirzepatide against semaglutide. At 72 weeks, tirzepatide produced 20.2% weight loss versus 13.7% with semaglutide. The difference was statistically significant and clinically meaningful.
A remote weight management program study found even more dramatic results in real-world settings. Among 339 participants (82% women), those using tirzepatide achieved mean weight loss of 22.9 kg (22.1% of baseline weight) at 12 months. Achievement of 10% or greater weight loss occurred in 95.2% of tirzepatide users.
For a 180-pound woman, that translates to roughly 40 pounds of weight loss over a year. These are transformative results that fundamentally change body composition, health markers, and quality of life.
Dosing protocol for women
Tirzepatide dosing follows a similar escalation pattern but uses different increments. Start at 2.5 mg weekly for four weeks. After four weeks, increase to 5 mg. Continue increasing in 2.5 mg increments every four weeks until reaching the target dose of 5 mg, 10 mg, or 15 mg weekly.
Most women find their effective dose between 7.5 mg and 15 mg. The highest doses produce the greatest weight loss but also carry more side effects. Finding the optimal balance for your body and goals matters more than reaching the maximum dose.
The tirzepatide dosing guide provides detailed protocols for different scenarios.
Comparing results: what the research shows
The JAMA Internal Medicine cohort study analyzed 41,222 adults meeting study criteria. After propensity score matching, 18,386 remained. The mean age was 52.0 years, and 12,970 participants (70.5%) were female. This large-scale real-world data confirmed that tirzepatide produces significantly greater weight loss than semaglutide.
However, greater weight loss does not automatically mean better choice. Cost, availability, side effect profiles, and individual response all factor into the decision. Some women respond excellently to semaglutide and see no reason to switch. Others hit plateaus on semaglutide and find tirzepatide breaks through.
The best peptide is the one that works for your body, fits your circumstances, and you can sustain long-term.
CJC-1295 and ipamorelin: the growth hormone approach
GLP-1 agonists work primarily through appetite suppression. Growth hormone secretagogues work differently, enhancing the metabolic machinery that burns fat while preserving muscle. For women seeking body recomposition rather than just weight loss, this distinction matters enormously.
Why growth hormone matters for female fat loss
Growth hormone influences metabolism in multiple ways. It increases lipolysis, the breakdown of stored fat for energy.
It preserves lean muscle mass during caloric deficits. It improves sleep quality, which impacts every other metabolic process. It enhances recovery, allowing more intensive training. And it supports collagen synthesis, maintaining skin elasticity as fat is lost.
Women particularly benefit because female physiology tends toward muscle loss during dieting. The combination of caloric restriction and hormonal fluctuations makes preserving muscle challenging. Losing muscle slows metabolism, making continued fat loss harder and regain easier.
Growth hormone secretagogues address this directly. They create hormonal conditions that favor fat loss while protecting muscle. The result is improved body composition, not just lower numbers on the scale.
The CJC-1295/ipamorelin combination
CJC-1295 is a growth hormone-releasing hormone analog. It stimulates pulsatile GH release over extended periods, mimicking natural secretion patterns. Ipamorelin is a selective GH secretagogue that works through different mechanisms. Combined, they produce synergistic effects greater than either alone.
Key benefits for women include increased fat metabolism especially in stubborn areas, improved sleep and recovery, muscle preservation during dieting, more energy and mental clarity, and hormonal rebalancing particularly valuable during perimenopause and postmenopause.
This combination is one of the most popular peptide protocols for women looking to enhance body composition and slow aging safely and without masculinizing effects.
Dosing and administration
Typical dosing ranges from 100-300 mcg of the combination per day. Injections are administered subcutaneously, usually once daily in the evening to support natural GH cycles that peak during deep sleep.
Some protocols recommend injections five days per week with a two-day break. Others use daily administration. Noticeable improvements typically begin around four to six weeks, with more significant changes over three to six months.
Fat loss takes time with this approach. Trust the process and stay consistent for 16-24 weeks minimum. This is not a quick fix. It is a strategy for sustainable body composition improvement.
Cycling every three to six months is recommended to prevent desensitization. Taking breaks allows the body to reset and maintain sensitivity to the peptides.
Stacking with other protocols
CJC-1295/ipamorelin stacks well with other approaches. Some women use it alongside semaglutide or tirzepatide to enhance muscle preservation during aggressive weight loss. Others combine it with other peptide stacks targeting different goals.
Tesamorelin can be combined for enhanced visceral fat reduction. BPC-157 and TB-500 can be added for recovery support if training intensity is high.
Any stacking protocol requires careful consideration of interactions, monitoring, and medical supervision. More is not automatically better, and complexity increases risk.
MOTS-C: the metabolic reset peptide
MOTS-C occupies a unique space in peptide therapy. It is not primarily a weight loss peptide. It is a metabolic optimization peptide that happens to support fat loss as a downstream effect. For women, particularly those experiencing metabolic dysfunction related to aging, this distinction has significant implications.
Understanding mitochondrial peptides
Most peptides are encoded in nuclear DNA. MOTS-C is different. It is a 16-amino acid peptide encoded within mitochondrial DNA, the genetic material inside the energy-producing organelles of every cell. This origin gives it unique properties affecting cellular energy production directly.
MOTS-C activates AMPK, often called the metabolic master switch. AMPK activation promotes glucose uptake, stimulates fat oxidation, inhibits new fatty acid synthesis, and triggers creation of new mitochondria. The cumulative effect is enhanced metabolic flexibility, the ability to efficiently switch between fuel sources.
For women with metabolic dysfunction, insulin resistance, or difficulty losing weight despite appropriate nutrition and exercise, MOTS-C addresses root causes rather than just symptoms.
Specific benefits for women
Research demonstrates particular relevance for postmenopausal women. Studies show that MOTS-C administration prevents ovariectomy-induced obesity and insulin resistance in mice via the AMPK pathway. This model parallels what happens in menopause when estrogen decline leads to metabolic changes.
The decline in endogenous MOTS-C may be blunted in premenopausal women due to estrogen's protective effects on mitochondrial function. As estrogen falls during menopause, this protection diminishes, potentially contributing to the fat accumulation and insulin resistance that commonly accompany this transition.
MOTS-C also promotes bone health, increasing osteoblast activity. For women at elevated osteoporosis risk, this secondary benefit adds value beyond metabolic effects.
Breast cancer survivor research shows MOTS-C correlates positively with increases in lean mass and decreases in fat mass following exercise. As lean mass increases and fat mass decreases, MOTS-C levels rise. This suggests a bidirectional relationship where both supplementation and lifestyle factors influence outcomes.
Dosing and expectations
MOTS-C is typically administered twice weekly via subcutaneous injection. Morning injections allow taking advantage of potential energizing effects. Injections are given in fatty areas such as thigh, upper arm, or abdomen.
Most patients report improvements in energy, stamina, and mood within two to four weeks. Gradual improvements in body composition and glucose regulation occur over two to three months. This is not a rapid fat loss solution. It is a metabolic optimization strategy that supports sustainable improvement.
Limitations and considerations
The vast majority of compelling MOTS-C data comes from preclinical animal models, primarily mice. Human research remains limited. While proposed mechanisms are promising, ongoing clinical trials will clarify the full range of applications.
MOTS-C works best as part of a comprehensive approach including proper nutrition, regular exercise, and lifestyle optimization. It enhances the metabolic environment for fat loss. It does not replace fundamental lifestyle factors.
AOD-9604: the targeted fat loss peptide
AOD-9604 deserves honest assessment. It promised targeted fat loss without broader hormonal effects. The reality is more nuanced, with clinical trial history that tempers enthusiasm while still suggesting potential utility for specific situations.
What AOD-9604 actually does
AOD-9604 is a 16-amino acid fragment of human growth hormone, specifically the portion involved in fat metabolism without the portions affecting growth, blood sugar, or other physiological parameters. The theory was elegant: extract the fat-burning component, eliminate the side effects.
In the body, AOD-9604 stimulates lipolysis (fat breakdown) and inhibits lipogenesis (fat creation). It does this without affecting blood sugar, appetite, or causing the cellular proliferation associated with full growth hormone.
Early animal studies showed promise. AOD-9604 reduced body weight in genetically obese rats and mice. Human trials followed, producing modest but measurable results: 2.6 kg average weight loss at 1 mg daily over 12 weeks compared to 0.8 kg with placebo.
Why development stopped
In 2007, Metabolic Pharmaceuticals terminated AOD-9604 development after a larger 24-week trial with 536 subjects failed to demonstrate statistically significant weight loss. The smaller benefits seen in earlier trials did not replicate at scale.
This does not mean AOD-9604 is useless. It means expectations must be calibrated appropriately. This is not a primary weight loss solution comparable to semaglutide or tirzepatide. It may be a supportive tool for specific situations when combined with appropriate lifestyle factors.
When AOD-9604 might make sense
Body recomposition phases where the goal is subtle fat reduction while maintaining muscle may benefit from AOD-9604. Women already at relatively low body fat percentages trying to address stubborn areas might find value. Those seeking modest enhancement to diet and exercise efforts without aggressive pharmaceutical intervention could consider it.
Dosing typically ranges from 300-500 mcg daily via subcutaneous injection. Research showed no additional benefit from doses higher than 1 mg daily, suggesting a ceiling effect. Cycles of 12-16 weeks with breaks are common protocols.
Realistic expectations
If your nutrition is unbalanced and activity levels are low, AOD-9604 likely will not deliver dramatic results. Combined with structured, high-protein nutrition and consistent training, it may enhance fat-loss efforts during recomposition phases.
Do not choose AOD-9604 expecting semaglutide-level results. The mechanisms are entirely different and the magnitude of effect does not compare. Choose it when the gentler, more targeted approach fits your situation and goals.
Tesamorelin: targeting visceral fat specifically
Visceral fat, the deep abdominal fat surrounding organs, poses particular health risks and resists conventional weight loss approaches. Tesamorelin specifically targets this stubborn fat depot with FDA-approved efficacy.
Understanding visceral fat and why it matters
Not all fat is equal. Subcutaneous fat, the fat you can pinch, is relatively metabolically benign. Visceral fat, accumulated around abdominal organs, actively secretes inflammatory compounds and hormones that increase risk of heart disease, type 2 diabetes, and other conditions.
Women experience increased visceral fat accumulation with menopause. As estrogen declines, fat distribution shifts from hips and thighs toward the midsection.
This is not vanity. Increased visceral fat correlates directly with increased health risk.
Traditional dieting reduces overall fat but does not preferentially target visceral stores. Exercise helps but often cannot fully address established visceral accumulation. Tesamorelin offers a more direct approach.
Clinical evidence for visceral fat reduction
Tesamorelin is FDA-approved for reducing excess abdominal fat in HIV-infected patients with lipodystrophy. In two pivotal randomized, double-blind, placebo-controlled trials, participants receiving tesamorelin saw visceral adipose tissue reductions of roughly 15-20% over 26 weeks, improvements far greater than placebo.
Off-label use for non-HIV patients with significant visceral adiposity is increasingly common in specialty and functional medicine settings. Ideal candidates usually have stubborn central fat, evidence of increased visceral adipose tissue, and willingness to combine peptide therapy with nutrition, exercise, and lifestyle changes.
Administration and dosing
Standard dosing is 2 mg daily via subcutaneous injection in the abdomen, rotating sites regularly. Treatment protocols typically involve injections five to seven days per week in multi-month cycles with programmed breaks under medical supervision.
Most patients notice changes within six to eight weeks, but peak results occur at 12-26 weeks. Visceral fat is stubborn. It accumulates slowly and leaves slowly. Clinical studies show maximum reduction at 26 weeks of consistent daily use.
Considerations for women
Clinical research enrolled predominantly male participants. Results may not directly translate to female physiology. This is not reason to avoid tesamorelin but reason for careful monitoring and realistic expectations.
Potential side effects include injection-site reactions, muscle or joint aches, nausea, fluid retention, and changes in blood sugar or IGF-1 levels requiring monitoring and possible dose adjustments.
Pregnancy, active cancer, uncontrolled diabetes, and specific endocrine conditions may contraindicate use. Medical evaluation before starting is essential.
Complete dosing protocols for women
Understanding general mechanisms matters. Having specific protocols to follow matters more. The following protocols represent evidence-based approaches adapted for female physiology, but they require medical supervision and individual adjustment.
Semaglutide protocol for women
Goal: Significant weight loss with appetite suppression
Starting dose: 0.25 mg subcutaneous injection weekly
Escalation schedule:
Weeks 1-4: 0.25 mg weekly
Weeks 5-8: 0.5 mg weekly
Weeks 9-12: 1.0 mg weekly
Weeks 13-16: 1.7 mg weekly
Weeks 17+: 2.4 mg weekly (if tolerated and needed)
Timing: Same day each week, any time of day
Duration: 6-18 months for lasting improvements
Expected results: 12-18% body weight reduction over one year for typical responders
Key notes: Stay at lower doses longer if side effects are significant. Many women achieve excellent results at 1.0 or 1.7 mg without reaching maximum dose.
Tirzepatide protocol for women
Goal: Maximum weight loss with dual metabolic support
Starting dose: 2.5 mg subcutaneous injection weekly
Escalation schedule:
Weeks 1-4: 2.5 mg weekly
Weeks 5-8: 5 mg weekly
Weeks 9-12: 7.5 mg weekly
Weeks 13-16: 10 mg weekly
Weeks 17+: 12.5-15 mg weekly (if tolerated and needed)
Timing: Same day each week, any time of day
Duration: 6-18 months for lasting improvements
Expected results: 18-25% body weight reduction over one year for typical responders
Key notes: More aggressive escalation increases side effects. Slower titration improves tolerability.
CJC-1295/Ipamorelin protocol for women
Goal: Body recomposition with muscle preservation and fat loss
Dose: 175-300 mcg combined peptide subcutaneous injection daily
Timing: Evening before bed to support natural GH cycles
Schedule: 5-6 days per week with 1-2 rest days
Duration: 16-24 weeks, then 4-8 week break before repeating
Expected results: Improved body composition, better sleep, enhanced recovery, modest fat loss (5-10 lbs typical), preserved or increased lean mass
Key notes: Results build gradually. Maintain caloric deficit for fat loss. High protein intake (1g per pound body weight) supports muscle preservation.
MOTS-C protocol for women
Goal: Metabolic optimization and insulin sensitivity
Dose: 5-10 mg subcutaneous injection
Timing: Morning, twice weekly
Duration: 8-12 weeks, assess and continue as needed
Expected results: Improved energy and stamina within 2-4 weeks, gradual body composition and glucose improvements over 2-3 months
Key notes: Best for metabolic dysfunction rather than primary weight loss. Combine with exercise for enhanced effect.
AOD-9604 protocol for women
Goal: Targeted fat reduction during recomposition
Dose: 300-500 mcg subcutaneous injection daily
Timing: Morning, fasted if possible
Duration: 12-16 weeks with 4-week break between cycles
Expected results: Modest fat reduction (2-5 lbs) when combined with structured nutrition and training
Key notes: Realistic expectations essential. Works as enhancement, not replacement, for lifestyle factors.
Tesamorelin protocol for women
Goal: Visceral fat reduction
Dose: 2 mg subcutaneous injection daily
Timing: Morning, rotating abdominal injection sites
Duration: 26 weeks for maximum VAT reduction, then assess continuation
Expected results: 15-20% visceral fat reduction at 26 weeks
Key notes: Requires monitoring of IGF-1, glucose, and lipid profiles. Medical supervision essential.
Combining peptides: stacking strategies for enhanced results
Strategic combination of complementary peptides can enhance results beyond what any single peptide achieves. However, stacking introduces complexity, cost, and potential for interactions. Understanding when and how to stack matters as much as understanding the individual peptides.
Principles of effective stacking
Stack peptides with different mechanisms. Combining two GLP-1 agonists makes no sense. Combining a GLP-1 agonist with a growth hormone secretagogue combines appetite suppression with metabolic enhancement, two different but complementary approaches.
Start single, then add. Establish baseline response to one peptide before adding another. This allows identifying what works, what causes side effects, and what to adjust.
Less is often more. The most effective stacks are usually two or three peptides, not five or six. Complexity increases risk without proportional benefit increase.
Effective stacking combinations for women
Weight loss with muscle preservation:
Semaglutide or tirzepatide for appetite suppression combined with CJC-1295/ipamorelin for muscle preservation and metabolic support. This combination addresses the common problem of losing muscle along with fat during aggressive dieting. The GLP-1 agonist enables caloric deficit. The GH secretagogue preserves lean mass.
Visceral fat focus:
Tesamorelin for direct visceral fat targeting combined with MOTS-C for metabolic optimization. This combination addresses stubborn abdominal fat from multiple angles. Tesamorelin directly promotes visceral fat breakdown. MOTS-C enhances cellular energy metabolism and insulin sensitivity.
Body recomposition stack:
CJC-1295/ipamorelin for GH support combined with additional peptides based on specific goals. Add BPC-157 if training hard and recovery is limiting progress. Add MOTS-C if metabolic dysfunction is present.
Stacks to approach carefully
Multiple GLP-1 agonists together provide no additional benefit and increase side effect risk.
High-dose growth hormone secretagogues combined with additional GH-affecting peptides can push IGF-1 levels higher than desired, requiring close monitoring.
Any stack involving more than three peptides becomes difficult to manage, expensive, and provides diminishing returns.
Monitoring stacked protocols
Stacking requires more intensive monitoring than single peptide use. Baseline bloodwork before starting. Follow-up labs at 6-8 weeks and periodically thereafter. IGF-1, fasting glucose, HbA1c, lipid panel, and liver function at minimum.
Track response to each component. If results plateau or side effects emerge, identify which peptide to adjust. Without careful tracking, stacking becomes guesswork.
Nutrition strategies that amplify peptide results
Peptides create hormonal environments conducive to fat loss. They do not eliminate the need for appropriate nutrition. In fact, nutrition becomes even more important because it determines whether you are losing fat, muscle, or both.
Protein requirements during peptide therapy
Higher protein intake is essential. Aim for 0.8-1.0 grams per pound of body weight daily, or 1.6-2.2 grams per kilogram. A 150-pound woman should target 120-150 grams of protein daily.
This may seem high, but it serves multiple purposes. Protein preserves muscle during caloric deficit. It increases satiety, supporting appetite control beyond peptide effects. It provides amino acids for recovery and tissue maintenance. And it has the highest thermic effect of any macronutrient, meaning you burn calories just digesting it.
GLP-1 agonists reduce appetite significantly. Ensuring adequate protein means prioritizing it at every meal before filling up on lower-priority foods.
Caloric considerations
Peptides create the optimal hormonal environment for fat loss, but you still need caloric deficit to lose weight. With CJC-1295/ipamorelin, you can use a larger deficit than typical without losing muscle. A moderate deficit of 500-750 calories below maintenance is recommended.
With GLP-1 agonists, the challenge often becomes eating enough. Severe undereating leads to muscle loss, nutrient deficiencies, and eventual metabolic adaptation. Track intake initially to ensure you are hitting minimum protein and calorie targets even as appetite decreases.
Meal timing and frequency
No single meal timing pattern works for everyone. Some women do well with intermittent fasting approaches, using GLP-1 effects to comfortably extend fasted periods. Others find that maintaining regular smaller meals works better.
With CJC-1295/ipamorelin, avoiding food for 1-2 hours before injection and 30-60 minutes after optimizes GH release. Food, particularly carbohydrates, can blunt the GH response.
For tesamorelin, morning administration on an empty stomach may optimize effect, though evidence for this is limited.
Hydration priorities
GLP-1 agonists slow gastric emptying and can cause constipation. Adequate hydration becomes more important than usual. Aim for at least half your body weight in ounces of water daily. A 160-pound woman should target at least 80 ounces.
Electrolyte balance also matters, particularly if eating less overall. Sodium, potassium, and magnesium intake may need attention.
Exercise optimization during peptide protocols
Exercise is not required for peptide-assisted weight loss. But exercise dramatically improves outcomes, body composition, and long-term maintenance. Understanding how to optimize training during peptide protocols maximizes results.
Resistance training priorities
Resistance training preserves and builds muscle during fat loss. This is critical because muscle mass determines metabolic rate. Lose muscle and your maintenance calories drop, making weight regain more likely.
Aim for resistance training 2-4 times weekly. Compound movements that work multiple muscle groups provide the most benefit per time invested. Squats, deadlifts, presses, rows, and lunges form the foundation.
Progressive overload matters. Gradually increasing weight, reps, or sets over time signals the body to maintain or build muscle despite caloric deficit.
Cardiovascular exercise
Moderate cardio supports cardiovascular health and creates additional caloric deficit. However, excessive cardio during aggressive weight loss can contribute to muscle loss and increase stress hormones.
Two to four moderate cardio sessions weekly of 20-40 minutes provides benefit without excess. Walking is underrated. Daily walking of 7,000-10,000 steps contributes significantly to energy expenditure without adding training stress.
Exercise with GLP-1 agonists
GLP-1 agonists can affect exercise capacity initially. Reduced food intake may temporarily reduce training energy. Some women experience nausea during exercise, particularly early in treatment.
Adjust training intensity as needed during dose escalation. Once stable on dose, energy typically normalizes and training can progress.
Exercise with growth hormone secretagogues
GH secretagogues enhance recovery, potentially allowing more training volume. Monitor for overtraining if significantly increasing exercise while on these peptides.
Intense exercise itself stimulates GH release. The combination of training and peptides creates additive effect on body composition.
Managing expectations: realistic timelines and outcomes
Unrealistic expectations lead to premature discontinuation. Understanding what to actually expect, and when, helps maintain commitment through the process.
What the research actually shows
Semaglutide produces average weight loss of 12-15% of body weight over one year for typical responders. Some lose more, some less. About 30% of users achieve 20% or greater weight loss. About 10-15% are relative non-responders with minimal effect.
Tirzepatide produces average weight loss of 18-22% of body weight over one year. Up to 40% achieve 25% or greater weight loss. Non-response rates are lower than semaglutide.
CJC-1295/ipamorelin produces modest weight loss of 5-15 pounds typical, but significant body recomposition with improved muscle-to-fat ratio even when scale changes are minimal.
Timeline expectations
Week 1-2: Minimal visible changes. Adjustment period. Possible side effects during dose titration.
Week 3-6: Appetite effects noticeable with GLP-1 agonists. Possible energy and sleep improvements with GH secretagogues. Scale may start moving.
Week 6-12: Weight loss accelerates for most. Body composition changes become visible. Energy stabilizes.
Month 3-6: Continued progress. May need dose adjustment. Body adapts to new patterns.
Month 6-12: Approaching maximum effect for most peptides. Maintenance considerations become relevant.
Factors affecting individual response
Starting weight matters. Those with more to lose often see larger percentage losses. Women starting at higher weights may see dramatic initial results that slow over time.
Metabolic health influences response. Insulin resistance, hormonal imbalances, and other factors affect how effectively peptides work.
Adherence determines outcomes. Consistent dosing, appropriate nutrition, and regular exercise separate best from average outcomes.
Genetics play a role. GLP-1 receptor variants and other genetic factors create individual variation in response.
Dealing with plateaus
Plateaus are normal and expected. The body adapts to caloric deficit by reducing energy expenditure. Metabolic adaptation is a survival mechanism, not a failure.
Strategies for breaking through include diet breaks (returning to maintenance calories briefly), adjusting macronutrients while maintaining deficit, increasing exercise intensity or volume, and dose adjustment if not at maximum.
Sometimes patience is the answer. Bodies release fat in spurts, not linear progressions. A plateau that lasts a few weeks often breaks spontaneously.
Safety considerations specific to women
Peptide therapy is generally well-tolerated, but women face specific considerations that require attention.
Pregnancy and reproductive health
GLP-1 agonists should be discontinued before pregnancy. The FDA recommends discontinuing semaglutide at least two months before planned pregnancy. Animal studies show potential fetal harm.
Effects on fertility are not fully characterized. Women actively trying to conceive should discuss peptide use with healthcare providers.
During lactation, most peptides have insufficient safety data. Conservative approach is to avoid during breastfeeding.
Hormonal interactions
Peptides interact with female hormones in complex ways not fully understood. Women on hormone replacement therapy should discuss peptide use with prescribers.
GLP-1 agonists may affect oral contraceptive absorption due to delayed gastric emptying. Backup contraception methods may be warranted, particularly during dose escalation.
Thyroid function monitoring is recommended with GLP-1 agonists. Report symptoms like neck swelling, difficulty swallowing, or voice changes.
Gallbladder considerations
Rapid weight loss increases gallstone risk. This is true regardless of weight loss method, but GLP-1 agonists carry specific gallbladder warnings. Symptoms include upper abdominal pain, especially after eating, that may radiate to the back or shoulder.
History of gallbladder disease does not automatically preclude peptide use but requires discussion with healthcare providers.
Bone health monitoring
Rapid weight loss can affect bone density. Women with osteoporosis risk factors should discuss bone health monitoring during peptide therapy. Adequate calcium, vitamin D, and weight-bearing exercise help mitigate risk.
Psychological effects
Weight loss, even when desired, can trigger complex psychological responses. Body image issues, disordered eating patterns, and adjustment to physical changes all occur.
The reduction in food preoccupation with GLP-1 agonists can be profoundly liberating for women who have struggled with food obsession. It can also create disorientation when food no longer provides its usual emotional function.
Support from healthcare providers, therapists familiar with weight loss psychology, or peer communities helps navigate these changes.
When to consider peptide therapy
Peptides are not first-line weight loss interventions for everyone. Understanding when they make sense helps with decision-making.
Appropriate candidates
Women who have genuinely tried lifestyle approaches without adequate results often benefit most from peptide therapy. This means sustained effort with nutrition and exercise, not just brief attempts.
BMI of 27 or greater with weight-related health conditions, or BMI of 30 or greater regardless of comorbidities, represents the typical clinical threshold for considering pharmaceutical weight loss assistance.
Metabolic dysfunction including insulin resistance, prediabetes, or difficulty maintaining blood sugar despite appropriate diet suggests potential benefit from metabolically-active peptides.
Age-related metabolic slowing, particularly during perimenopause and menopause, creates situations where peptides can restore metabolic function that lifestyle alone cannot address.
When to wait or avoid
Without genuine lifestyle foundation, peptides provide temporary solutions. Developing sustainable nutrition and exercise habits first creates the foundation for peptide-enhanced results.
During pregnancy, breastfeeding, or active attempts to conceive, most peptides should be avoided due to insufficient safety data.
Certain medical conditions contraindicate specific peptides. Personal or family history of medullary thyroid carcinoma or MEN2 contraindicates GLP-1 agonists. Active pancreatitis, severe gastrointestinal disease, and other conditions require individual evaluation.
Psychological readiness matters. If the relationship with food is primarily disordered rather than metabolically driven, addressing psychological factors may be more appropriate than pharmaceutical intervention.
Finding qualified medical supervision
Peptide therapy requires medical supervision. The quality of that supervision significantly affects outcomes and safety.
What to look for in providers
Experience with peptide therapy specifically, not just general medical practice. Ask how many patients they have treated with the specific peptides you are considering.
Willingness to provide comprehensive monitoring including baseline labs, follow-up testing, and ongoing assessment. Providers who prescribe without monitoring are not providing adequate care.
Evidence-based approach. Skepticism of extreme claims and willingness to discuss both benefits and limitations indicates appropriate perspective.
Accessibility. Ongoing questions and concerns should have clear channels for communication with the prescribing provider.
Questions to ask potential providers
What is your experience with peptide therapy for weight loss?
What monitoring do you provide and how frequently?
What happens if I have side effects or concerns between appointments?
How do you determine appropriate dosing and protocol adjustments?
What outcomes have your patients typically achieved?
Red flags
Guaranteed results. No provider can guarantee specific outcomes because individual variation is inherent to peptide therapy.
No monitoring required. Proper peptide therapy requires ongoing assessment and adjustment.
One-size-fits-all protocols. Individual adjustment based on response is standard practice.
Pressure to purchase additional products or services beyond the therapeutic peptides.
Frequently asked questions
How quickly will I see weight loss results with peptides?
Most women notice appetite changes within two to four weeks of starting GLP-1 agonists. Visible weight loss typically begins in weeks four through eight. Maximum effect develops over six to twelve months. Growth hormone secretagogues work more gradually, with body composition changes often taking three to six months to become noticeable.
Can I use peptides if I am over 50?
Yes, and women over 50 often represent ideal candidates. Age-related metabolic decline, hormonal changes from menopause, and increased visceral fat accumulation are precisely the conditions peptides address well. Appropriate monitoring is especially important due to increased risk of gallbladder issues and other age-related concerns.
Will I regain weight after stopping peptides?
Some weight regain is common after discontinuing GLP-1 agonists, typically 30-50% of lost weight over one to two years in studies. Establishing sustainable lifestyle habits during peptide use, transitioning gradually rather than stopping abruptly, and potentially using maintenance dosing can minimize regain.
Are peptides safe to use with other medications?
It depends on the specific medications. GLP-1 agonists can affect absorption of oral medications due to delayed gastric emptying. They may enhance effects of insulin and other diabetes medications, requiring dose adjustments. Always provide complete medication lists to prescribing providers and coordinate with other healthcare providers managing your medications.
Can peptides help with stubborn belly fat specifically?
Tesamorelin specifically targets visceral abdominal fat and has FDA approval for this indication. GLP-1 agonists produce overall fat loss including abdominal fat. CJC-1295/ipamorelin combinations may preferentially support fat loss in stubborn areas including abdomen, hips, and thighs, though this is less well established.
How do I know which peptide is right for me?
Goals determine optimal choices. Maximum weight loss suggests GLP-1 agonists. Body recomposition with muscle preservation suggests growth hormone secretagogues. Visceral fat specifically suggests tesamorelin. Metabolic dysfunction suggests MOTS-C. Many women benefit from combinations. Medical evaluation helps match peptides to individual situations.
What side effects should I expect?
GLP-1 agonists commonly cause nausea, particularly during dose escalation, along with constipation and occasional diarrhea. Growth hormone secretagogues may cause water retention, joint discomfort, and tingling sensations. AOD-9604 is generally well-tolerated with minimal side effects. Individual response varies significantly.
Can I exercise normally while on peptides?
Yes, and exercise is recommended. Initial adjustment period with GLP-1 agonists may require reducing training intensity temporarily. Once stable on dose, most women return to normal training. Growth hormone secretagogues may enhance recovery, potentially allowing increased training volume.
External resources
For women serious about optimizing their peptide protocols, SeekPeptides offers the most comprehensive resource available. Evidence-based guides, proven protocols, and a community of thousands who have navigated these exact questions provide support throughout your journey.
In case I do not see you, good afternoon, good evening, and good night. May your protocols stay effective, your metabolism stay optimized, and your results stay lasting.



