Feb 1, 2026
Your pineal gland is shrinking. It started calcifying before you turned 20, and by the time you hit 50, it produces less than a fifth of the melatonin it made during childhood. That is not speculation. That is biology. And it explains why sleep becomes harder, shallower, and less restorative as you age, no matter how disciplined your bedtime routine is.
The problem goes deeper than melatonin supplements can reach.
Exogenous melatonin replaces what is missing, but it does nothing to restore the gland itself. It does not reverse calcification. It does not upregulate the enzymes responsible for melatonin synthesis. It does not retrain your circadian clock at the genetic level. That is precisely where pineal peptides enter the picture, offering a fundamentally different approach to sleep restoration that works with your biology rather than around it. These peptides, derived from or designed to target pineal gland tissue, aim to rehabilitate the organ responsible for your sleep architecture instead of merely compensating for its decline.
This guide covers the three most researched pineal peptides for sleep: Pinealon, Epitalon, and DSIP. You will learn how each one works at the cellular level, what the research actually shows (and what it does not), specific protocols researchers use, and how to determine which peptide matches your particular sleep problem. Whether you are dealing with chronic insomnia, age-related sleep fragmentation, circadian rhythm disruption from shift work, or simply want deeper, more restorative rest, understanding these peptides gives you options that conventional sleep aids cannot match. SeekPeptides members have access to detailed protocols for each of these compounds, and this guide will give you the foundation you need to understand why they work.
Why your pineal gland matters more than you think
Rene Descartes called it the seat of the soul. Modern science calls it a neuroendocrine transducer. Both descriptions hint at something important: the pineal gland punches far above its weight. Weighing barely 150 milligrams, this tiny pine-cone-shaped structure sits deep in the center of your brain, tucked between the two hemispheres. Its primary job is converting information about light and darkness into a chemical signal, melatonin, that orchestrates your entire circadian rhythm.
But melatonin is just the beginning.
The pineal gland also produces several bioactive peptides and neurotransmitters that influence everything from immune function to reproductive hormones to oxidative stress defense. It receives input from the suprachiasmatic nucleus (SCN) of the hypothalamus, which acts as the body master clock, and translates that input into hormonal signals that synchronize virtually every biological process in your body. When this system works correctly, you fall asleep easily, cycle through all sleep stages efficiently, wake feeling refreshed, and maintain consistent energy throughout the day.
When it does not, everything unravels.
The calcification problem nobody talks about
Here is the uncomfortable truth about your pineal gland. It has the highest calcification rate of any organ in the human body. Calcium, phosphorus, and fluoride deposits begin accumulating in childhood, and by age 60, most people have significant calcification that directly impairs melatonin production. Research published in the journal Molecules found that this calcification jeopardizes melatonin synthetic capacity and is associated with a variety of neuronal diseases, including cognitive decline and neurodegeneration.
The consequences for sleep are severe. Calcified pineal tissue produces less melatonin. Less melatonin means weaker circadian signals. Weaker circadian signals mean fragmented sleep, difficulty falling asleep, reduced slow-wave sleep, and impaired REM cycles. It is a cascade that worsens year after year, and taking melatonin pills does nothing to address the underlying structural problem. This is why researchers have turned their attention to peptides that can potentially restore pineal function at the cellular level, rather than simply replacing its output.
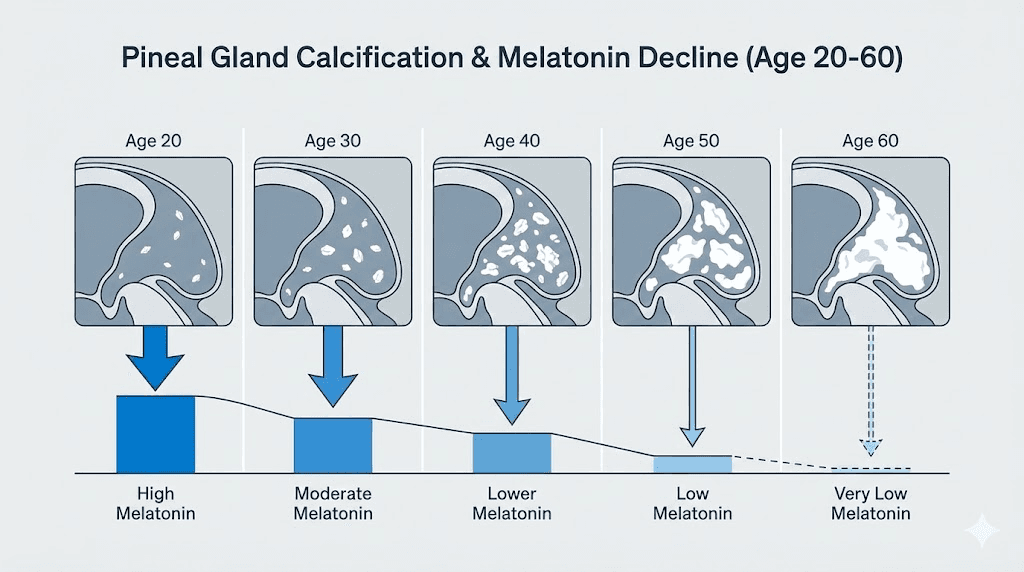
Melatonin production across the lifespan
The numbers tell a striking story. Melatonin rhythms first appear around 2 to 3 months after birth, with levels rising exponentially through childhood until reaching a lifetime peak in prepubertal children. A steady decrease follows, reaching typical adult concentrations by the late teens. Values remain relatively stable until ages 35 to 40, then begin a significant decline in both amplitude and baseline levels. By age 90, melatonin levels drop below 20% of young adult concentrations.
Multiple factors drive this decline. The density of beta-adrenergic receptors in the pineal gland decreases with age. Gene expression and phosphorylation of AANAT (the rate-limiting enzyme in melatonin synthesis) become downregulated. And here is something most people miss: aged cells generate more reactive oxygen species, and since melatonin acts as a potent endogenous antioxidant, the body consumes more of it to neutralize oxidative stress. So you are producing less while using more. It is a double hit that explains why longevity researchers pay such close attention to pineal health.
This age-related decline is not merely inconvenient. Research from the journal Experimental Gerontology describes a theory where deteriorating melatonin rhythms cause other circadian rhythms to weaken and desynchronize, contributing significantly to the aging process itself and rendering the body more susceptible to age-related diseases. In other words, poor sleep is not just a symptom of aging. It may actually accelerate it. Understanding this connection is what makes bioregulator peptides targeting the pineal gland so compelling for both sleep optimization and longevity.
The three pineal peptides that matter for sleep
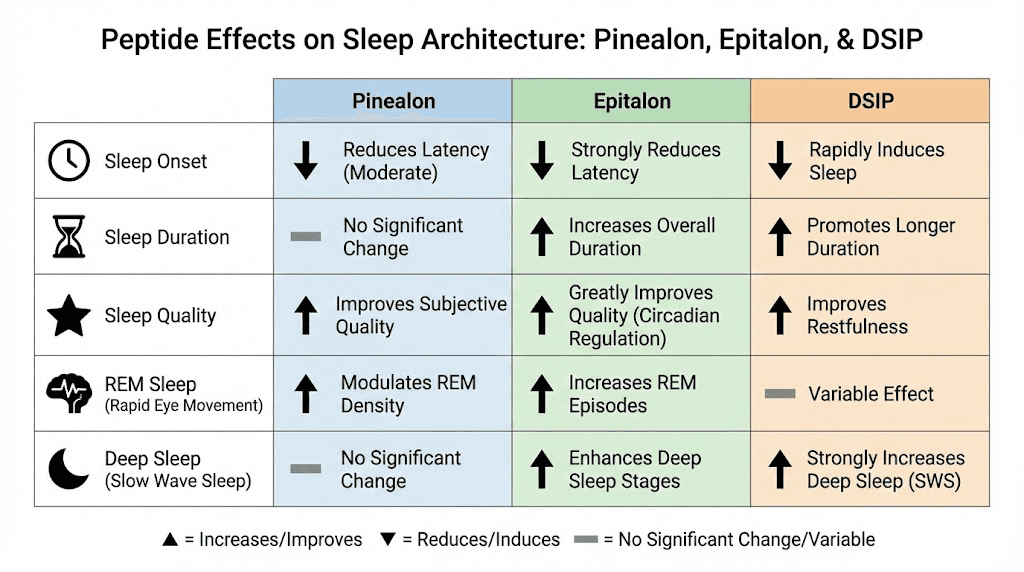
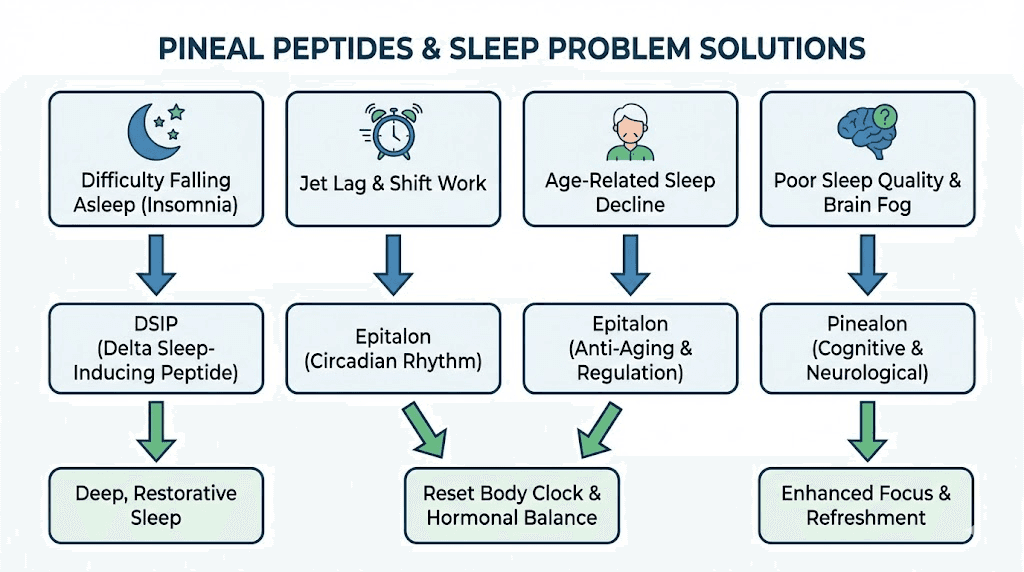
Not all sleep peptides are created equal. Some work on the hypothalamus. Some modulate GABA receptors. Some target growth hormone release. But three specific peptides stand out for their direct action on pineal gland function and sleep architecture: Pinealon, Epitalon, and DSIP. Each takes a different approach to the same fundamental problem, and understanding their distinct mechanisms helps you determine which one, or which combination, fits your situation.
Think of it this way. Pinealon is the neuroprotector that calms brain activity and supports serotonin pathways. Epitalon is the regenerator that restores melatonin production at the enzymatic level. DSIP is the sleep inducer that directly promotes deep delta-wave sleep. They complement each other, and many researchers use them in combination, but each has value on its own depending on the primary sleep issue being addressed.
Pinealon: the neuroprotective sleep optimizer
Pinealon is a tripeptide consisting of three amino acids: glutamic acid, aspartic acid, and arginine (Glu-Asp-Arg). Originally developed in Russia by Professor Vladimir Khavinson for military and cosmonaut applications, it was designed to protect brain function under extreme stress and high-pressure environments. Its mechanism centers on direct pineal gland function enhancement, melatonin production optimization, and circadian clock gene expression modulation.
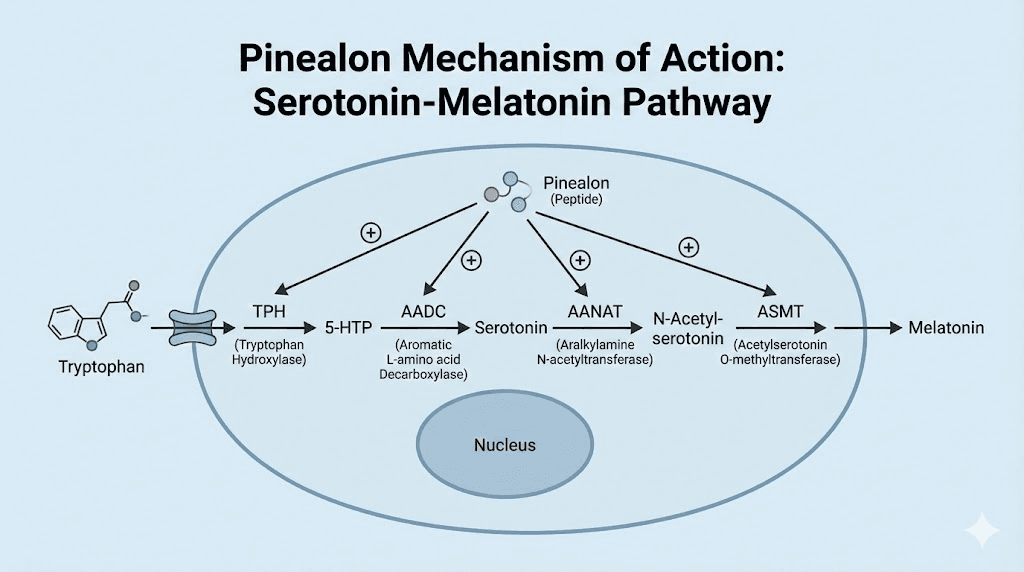
What makes Pinealon unique among sleep peptides is its neuroprotective profile. A 2014 in vitro study on brain cortex cells demonstrated that Pinealon stimulates serotonin expression, the neurotransmitter that serves as the direct precursor to melatonin. This is significant because the melatonin synthesis pathway runs from tryptophan to serotonin to N-acetylserotonin to melatonin. By boosting serotonin production in brain tissue, Pinealon supports the entire upstream chain rather than just the final product.
A 2012 study in aged rats found that Pinealon injection improved behavioral sleep patterns. The peptide did not force sedation. It helped restore normal sleep architecture, a critical distinction from pharmaceutical sleep aids that often suppress certain sleep stages while artificially extending others. This aligns with what researchers observe clinically: Pinealon helps the body remember how to sleep on its own, rather than creating artificial drowsiness.
For people dealing with anxiety-related sleep problems, Pinealon offers particular advantages. Its neuroprotective properties calm overactive neural circuits without sedation, making it easier to transition into sleep naturally. Research suggests it may help mitigate circadian disruptions caused by shift work and jet lag by modulating circadian clock gene expression, essentially helping your internal clock recalibrate after being knocked off rhythm. This makes it relevant for anyone whose sleep problems stem from stress, irregular schedules, or cognitive overactivation at bedtime.
Epitalon: the pineal gland regenerator
Epitalon (also written as Epithalon) is a synthetic tetrapeptide with the sequence Ala-Glu-Asp-Gly (AEDG). It was developed as a synthetic version of Epithalamin, a peptide complex originally extracted from bovine pineal gland tissue. For years, researchers suspected it existed naturally in the human body, and in 2017, Epitalon was detected for the first time in physiological pineal gland extract, confirming it as an endogenous compound.
The primary sleep-related mechanism of Epitalon is its direct influence on melatonin synthesis. In rat pinealocytes (the melatonin-producing cells of the pineal gland), Epitalon was shown to upregulate both AANAT (arylalkylamine N-acetyltransferase, the rate-limiting enzyme in melatonin production) and pCREB (a transcription factor involved in melatonin gene expression). This is not a subtle effect. It represents direct enzymatic stimulation of the melatonin biosynthesis machinery.
But Epitalon goes further than just boosting enzyme activity.
Research demonstrates that it protects pineal tissue itself from age-related degeneration. In aged human pinealocytes, Epitalon selectively safeguarded cells from degenerative changes, suggesting a tissue-specific rejuvenating effect on the very gland responsible for circadian control. This is fundamentally different from taking melatonin. Where supplemental melatonin replaces what is missing, Epitalon aims to restore the factory that produces it. It is the difference between refilling a leaking tank and repairing the tank itself.
The evidence in aging primates is particularly compelling. When researchers administered Epitalon to old rhesus monkeys (aged 20 to 27 years), nighttime melatonin levels increased significantly. Notably, the same treatment had no effect on young monkeys, suggesting that Epitalon specifically addresses age-related decline rather than artificially elevating melatonin beyond normal levels. This selective action is exactly what you want in a sleep-focused peptide protocol, something that restores normal function without overshooting.
Beyond melatonin, Epitalon has earned attention in longevity research for its ability to stimulate telomerase activity. A 2003 review published in the International Journal of Molecular Sciences detailed Epitalon regulatory influence on circadian genes including Clock, Csnk1e, and Cry2. These genes control your internal biological clock, and their proper expression is essential for maintaining healthy sleep-wake cycles. By modulating these genes, Epitalon acts as what researchers describe as a molecular metronome, realigning internal timekeeping mechanisms that tend to falter with age.
Long-term studies show additional benefits. One trial involving six courses of Epithalamin over three years demonstrated decelerated cardiovascular aging, preserved physical endurance, normalized circadian melatonin rhythm, and improved carbohydrate and lipid metabolism. The treatment group also showed significantly lower mortality compared to controls. While these results come primarily from the Khavinson research group in Russia and have not been independently replicated, they represent the most extensive human data available on pineal peptide supplementation.
DSIP: the delta-wave sleep promoter
Delta sleep-inducing peptide is a nonapeptide (nine amino acids: Trp-Ala-Gly-Gly-Asp-Ala-Ser-Gly-Glu) originally isolated from the hemodialysates of sleeping rabbits in 1977. Unlike Pinealon and Epitalon, which primarily target the pineal gland, DSIP is produced in the hypothalamus and works through a broader range of neurological pathways. Its name gives away its primary function: promoting delta-wave sleep, the deepest and most restorative stage of the sleep cycle.
Understanding why delta sleep matters requires a brief detour into sleep architecture. Your sleep consists of four stages that cycle approximately every 90 minutes. Stages 1 and 2 are light sleep. Stage 3 is deep slow-wave (delta) sleep, where tissue repair, growth hormone release, immune system strengthening, and memory consolidation primarily occur. Stage 4 is REM sleep, associated with dreaming and cognitive processing. Most adults spend only 15 to 20 percent of total sleep time in deep delta sleep, and this percentage decreases with age. By 60, some people get almost no stage 3 sleep at all.
This is the problem DSIP targets directly.
Research shows that DSIP promotes slow-wave sleep specifically, increasing both the depth and duration of delta-wave activity. In a controlled double-blind study, single and multiple DSIP injections normalized disturbed sleep patterns, and participants showed better performance and increased alertness during waking hours, along with improved stress tolerance. A separate study on chronic insomniacs found higher sleep efficiency and shorter sleep latency with DSIP compared to placebo.
The mechanism behind these effects is complex and, honestly, still not fully understood four decades after the peptide discovery. DSIP appears to interact with NMDA receptors, components of the MAPK signaling cascade, and glucocorticoid pathways. It decreases basal corticotropin levels and blocks cortisol release, which explains its stress-reducing properties. It also stimulates the release of growth hormone through somatoliberin stimulation, connecting sleep quality directly to recovery and repair processes.
One of DSIP most interesting properties is its apparent safety profile. A 2001 editorial in the European Journal of Anaesthesiology described DSIP as "incredibly safe," noting that no dose had ever killed an animal subject in research, and the only human side effects observed were transient headache, nausea, and vertigo. The peptide crosses the blood-brain barrier easily and is not denatured by digestive enzymes, making it versatile in terms of administration routes.
Beyond sleep, DSIP research has revealed potential applications in pain management (showing analgesic effects when administered intracerebroventricularly), addiction treatment (alleviating withdrawal symptoms in 97% of opiate-dependent and 87% of alcohol-dependent patients in one trial), antioxidant defense, and even stroke recovery. Intranasal DSIP administration accelerated motor function recovery in rats after focal stroke, suggesting neuroprotective effects that extend well beyond sleep regulation.
How pineal peptides compare to conventional sleep aids
The fundamental difference between pineal peptides and conventional sleep medications comes down to philosophy. Pharmaceutical sleep aids, from benzodiazepines to Z-drugs like zolpidem, work by suppressing central nervous system activity. They force sleep by dampening neural function. And they work. In the short term. But that forced sedation comes at a cost: altered sleep architecture, next-day grogginess, tolerance development, dependency risk, and rebound insomnia when you stop taking them.
Pineal peptides take the opposite approach. They do not force anything.
Instead, they support the biological systems responsible for natural sleep. Pinealon calms overactive neural circuits and supports serotonin production. Epitalon restores melatonin synthesis at the enzymatic level. DSIP promotes deep sleep through natural neurological pathways. None of them suppress consciousness or create artificial sedation. The result is sleep that feels normal, cycling through all stages properly, because the body is actually performing normal sleep processes rather than being chemically shut down.
This distinction matters enormously for long-term outcomes. Research suggests Pinealon has a low risk of dependency. DSIP studies have not demonstrated tolerance development with repeated use. Epitalon works by restoring function rather than providing exogenous compounds, so there is no withdrawal when you stop. Compare that to the well-documented withdrawal syndromes associated with benzodiazepines and the rebound insomnia that follows discontinuation of most pharmaceutical sleep aids.
That said, honesty requires acknowledging the limitations. Pineal peptides do not have the extensive clinical trial data that pharmaceutical sleep aids do. Much of the Epitalon research comes from a single group in Russia. DSIP mechanism of action is still not fully characterized after 40 years. And Pinealon studies are predominantly preclinical. These are promising compounds, not proven medications, and anyone considering them should understand that distinction clearly.
Who benefits most from pineal peptides
Not everyone with sleep problems needs pineal peptides. Someone with acute insomnia triggered by a stressful life event might resolve the problem simply by addressing the stressor. Someone with sleep apnea needs a CPAP machine, not a peptide. The question of who benefits most from pineal peptides comes down to the underlying mechanism driving the sleep problem.
Adults over 40 with declining sleep quality
This is the primary population where pineal peptides show the strongest rationale. After 40, melatonin production declines measurably, pineal calcification accelerates, and sleep architecture progressively deteriorates. Epitalon research specifically targets this population, with primate studies showing melatonin restoration only in aged subjects, not young ones. If your sleep was fine in your 20s and 30s but has gradually worsened, age-related pineal decline is the most likely culprit, and pineal peptides address that directly.
Shift workers and frequent travelers
Circadian rhythm disruption from rotating shifts or frequent time zone changes creates a specific type of sleep problem that melatonin alone handles poorly. Pinealon research suggests benefits for circadian rhythm synchronization in shift work disorders, and Epitalon modulation of circadian genes (Clock, Csnk1e, Cry2) offers a deeper reset than simply taking melatonin at a new bedtime. If your sleep problems are primarily about timing rather than ability, these peptides may offer advantages over conventional approaches.
People with stress-related sleep disruption
When cortisol stays elevated at night, falling asleep becomes nearly impossible. DSIP directly addresses this by decreasing basal corticotropin levels and blocking cortisol release. Pinealon neuroprotective properties calm overactive neural circuits. Together or individually, they target the hormonal and neurological basis of stress-related insomnia, which explains why researchers studying anxiety and peptide protocols often include one or both in their frameworks.
Those seeking deeper, more restorative sleep
Even people who sleep seven to eight hours sometimes wake feeling unrefreshed. The problem is usually insufficient deep sleep, specifically stage 3 slow-wave sleep, where the most critical restoration occurs. DSIP specifically promotes delta-wave sleep, addressing this exact problem. If you sleep enough hours but never feel rested, delta sleep deficiency is the prime suspect, and DSIP is the peptide designed for that.
Dosage protocols and administration
Dosage information for pineal peptides exists primarily in a research context, as none of these compounds are approved medications. What follows reflects protocols documented in research literature and clinical practice settings. Individual needs vary, and working with a qualified healthcare provider is essential for determining appropriate approaches. SeekPeptides members access detailed protocol builders and dosing guidance that account for individual factors.
Pinealon protocols
Pinealon is available in both injectable and oral/sublingual formulations, giving researchers flexibility in administration.
Subcutaneous injection protocol:
Starting dose: 200 to 300 mcg daily
Titration: Increase by approximately 100 mcg every 1 to 2 weeks as tolerated
Target dose: 400 to 500 mcg daily by weeks 5 through 12
Frequency: Once daily, subcutaneous
Cycle length: 8 to 12 weeks, with optional extension to 16 weeks
Timing: Consistent daily timing, typically evening for sleep applications
Oral/sublingual protocol:
Duration: 30 days
Frequency: 1 to 4 cycles per year
Best combined with: Exercise and nutrient-rich diet
Injection sites should be rotated between the abdomen, thighs, and upper arms to prevent lipohypertrophy and ensure consistent absorption. For injection technique details, clean the vial stopper and skin with alcohol, allow to dry, pinch a skinfold, and insert the needle at 45 to 90 degrees into subcutaneous tissue. Aspiration is not recommended for routine subcutaneous injections.
Epitalon protocols
Epitalon is typically administered in shorter, more intensive cycles compared to Pinealon.
Standard injection protocol:
Dose: 1 to 2 mg daily
Duration: 10 to 20 day cycles
Frequency: 1 to 3 cycles per year, spaced 4 to 6 months apart
Timing: Evening administration to align with natural melatonin production timing
Administration: Subcutaneous or intramuscular
Maintenance protocol (sublingual):
Daily sublingual sprays between injection cycles
Lower bioavailability than injection but convenient for ongoing support
The cyclic nature of Epitalon protocols reflects how the peptide works. Rather than continuous supplementation, Epitalon aims to stimulate the pineal gland restoration processes that then continue independently for months. Think of it like jump-starting a car battery rather than keeping jumper cables permanently attached. This cycling approach aligns with how experienced researchers structure peptide protocols for optimal results with minimal intervention.
DSIP protocols
DSIP protocols vary more widely in the literature, reflecting the peptide long research history across multiple applications.
Research protocol (based on published studies):
Dose: Varies by study; intranasal doses of approximately 120 mcg/kg used in animal research
Timing: Evening administration, typically 30 to 60 minutes before intended sleep
Onset: Sleep pressure reported within approximately 130 minutes of administration in human studies
Duration: Effects on sleep architecture observed with both single doses and multi-day protocols
Regarding cycling, the evidence is mixed. Some researchers note that DSIP does not appear to induce tolerance with repeated use, while others recommend cycling as a precautionary measure. The conservative approach involves using DSIP for defined periods (10 to 20 days) followed by equal or longer breaks, similar to other peptide cycling strategies.
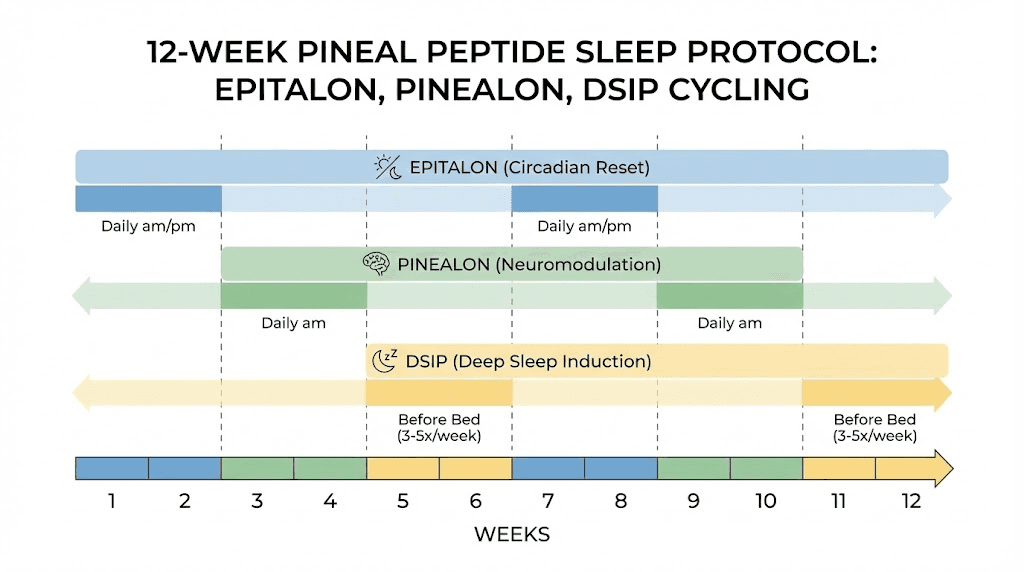
Stacking pineal peptides for sleep
Many researchers combine Epitalon and Pinealon for comprehensive sleep support, and the rationale is sound. While Epitalon resets the body internal clock by restoring melatonin production, Pinealon calms the mind and stabilizes the brain bioenergetic environment. Together, they address both the hormonal and neurological components of sleep disruption.
A common combination protocol:
Epitalon: 10-day injection cycle (1 to 2 mg daily) every 4 to 6 months
Pinealon: Daily sublingual or injection between Epitalon cycles
DSIP: Added as needed for acute sleep difficulties or during high-stress periods
The stacking approach allows each peptide to address a different aspect of sleep dysfunction. Epitalon handles the structural restoration of the pineal gland. Pinealon maintains neuroprotective support and serotonin optimization. DSIP provides acute deep-sleep promotion when needed. This layered strategy mirrors how experienced researchers approach other multi-peptide protocols.
Storage, handling, and reconstitution
Proper storage is not optional. It is the difference between a peptide that works and expensive water.
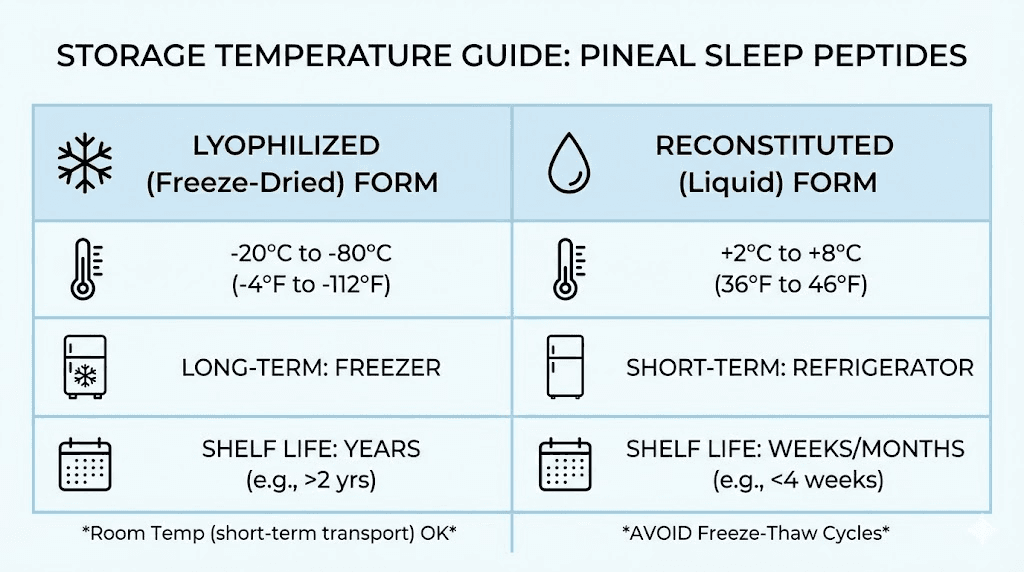
All three pineal peptides follow similar storage and handling requirements. Lyophilized (freeze-dried) peptide should be stored at minus 20 degrees Celsius (minus 4 degrees Fahrenheit) for long-term storage. Once reconstituted with bacteriostatic water, store at 2 to 8 degrees Celsius (35.6 to 46.4 degrees Fahrenheit), which means your refrigerator. Avoid repeated freeze-thaw cycles, as these degrade peptide structure and potency.
For reconstitution, use bacteriostatic water rather than sterile water. The bacteriostatic agent (typically 0.9% benzyl alcohol) prevents bacterial growth, extending the usable life of your reconstituted peptide. When adding water to the vial, direct the stream against the glass wall rather than directly onto the peptide cake, and swirl gently rather than shaking. These precautions preserve peptide integrity.
The SeekPeptides reconstitution calculator can help you determine exact water volumes for your specific vial sizes. Getting the concentration right matters for accurate dosing, and small errors in reconstitution translate to significant dosing variations over a full cycle. For more detail on mixing peptides with bacteriostatic water, follow proper sterile technique throughout the process.
Reconstituted DSIP specifically should be stored at 4 degrees Celsius (39 degrees Fahrenheit) according to the UK National Institute for Biological Standards and Control. Most reconstituted peptides remain viable for approximately 4 to 6 weeks in the refrigerator, though potency gradually declines over time. Label your vials with the reconstitution date and discard any that are more than 6 weeks old or show cloudiness, particles, or discoloration.
The science behind pineal gland restoration
Understanding why pineal peptides work requires understanding what goes wrong with the pineal gland during aging. The story is more nuanced than simple calcification, though that is certainly part of it.
The melatonin synthesis pathway
Melatonin production follows a precise biochemical chain. It begins when the retina detects darkness and sends signals through the retinohypothalamic tract to the suprachiasmatic nucleus (SCN). The SCN relays this information through the superior cervical ganglion to the pineal gland via noradrenergic nerve fibers. Norepinephrine released at the pineal gland activates beta-1 adrenergic receptors, which upregulate cyclic AMP (cAMP). This triggers the phosphorylation and activation of AANAT (arylalkylamine N-acetyltransferase), the rate-limiting enzyme that converts serotonin to N-acetylserotonin. The final step converts N-acetylserotonin to melatonin via hydroxyindole-O-methyltransferase (HIOMT).
Every step in this chain is vulnerable to age-related decline.
Beta-adrenergic receptor density decreases. AANAT gene expression and phosphorylation become impaired. Serotonin availability may decline. And the pineal cells themselves degenerate. Pineal peptides intervene at multiple points. Epitalon directly upregulates AANAT and pCREB (the transcription factor that drives melatonin gene expression). Pinealon stimulates serotonin expression in brain tissue, supporting the upstream supply. This multi-point intervention is why peptide approaches can achieve what single-compound supplements cannot.
Circadian gene expression
The circadian clock is not just about melatonin levels. It is a complex network of interlocking genetic feedback loops involving clock genes (Clock, Bmal1), period genes (Per1, Per2, Per3), and cryptochrome genes (Cry1, Cry2). These genes regulate each other in cycles of approximately 24 hours, and their coordinated expression is essential for proper sleep-wake rhythms.
Epitalon has been shown to modulate multiple circadian genes, including Clock, Csnk1e, and Cry2. This is significant because age-related sleep disruption often involves not just melatonin deficiency but broader circadian gene dysfunction. By acting at the genetic level, Epitalon offers the possibility of realigning the entire circadian system rather than simply adding more melatonin to a broken clock. This mechanism distinguishes it from virtually every other sleep intervention available and is a key reason longevity researchers are so interested in this peptide.
Neuroprotection and sleep quality
Sleep quality depends on more than just the timing and depth of sleep stages. The brain neural environment matters enormously. Oxidative stress, neuroinflammation, and neuronal damage all impair sleep quality even when the circadian system is functioning. This is where the neuroprotective properties of pineal peptides become relevant.
Pinealon research suggests it mitigates cellular aging in the central nervous system. Studies indicate it may exhibit anabolic effects in the brain, potentially slowing cellular aging processes. For sleep, this means the neural circuits responsible for sleep initiation, maintenance, and cycling function more effectively. If your sleep disruption involves frequent awakenings, difficulty maintaining sleep, or non-restorative sleep despite adequate duration, neuroprotective peptides targeting brain health may address the underlying issue.
DSIP also demonstrates neuroprotective effects, including antioxidant properties and stroke recovery benefits. A 2011 study concluded that DSIP has a strong antioxidant effect by activating the body natural mechanisms against oxidative stress. This connects to sleep because oxidative stress in the brain is both a cause and consequence of poor sleep, creating a vicious cycle that neuroprotective peptides may help break.
Common mistakes researchers make with pineal peptides
The difference between researchers who report significant sleep improvements and those who see minimal results often comes down to protocol errors rather than peptide quality. Here are the most common mistakes and how to avoid them.
Expecting overnight results
Pineal peptides are not sleeping pills. They do not knock you out the first night you use them. Pinealon and Epitalon work by restoring biological function, and that takes time. Most researchers report initial subtle improvements within 7 to 10 days, with significant changes in sleep quality emerging over 3 to 6 weeks. If you quit after three days because nothing happened, you never gave the peptide a chance to do its work. DSIP works faster, with sleep pressure reported within hours, but even its full effects on sleep architecture normalization develop over multiple doses.
Using the wrong peptide for the problem
Trouble falling asleep (sleep onset insomnia) is a different problem from waking frequently (sleep maintenance insomnia), which is different from non-restorative sleep. Epitalon is best for age-related melatonin decline and circadian rhythm issues. DSIP targets deep sleep deficiency and acute insomnia. Pinealon addresses stress-related and neuroprotective sleep concerns. Using DSIP for a circadian rhythm problem or Epitalon for stress-related insomnia means applying the wrong tool to the wrong problem.
Ignoring sleep hygiene basics
No peptide can overcome blue light exposure until midnight, caffeine at 4 PM, and an inconsistent sleep schedule. Pineal peptides work best as part of a comprehensive sleep optimization strategy that includes appropriate light exposure (bright in morning, dim in evening), consistent sleep-wake times, cool sleeping environment (65 to 68 degrees Fahrenheit), limited stimulants after noon, and reduced screen exposure before bed. The peptides restore biological capacity for good sleep. Your habits determine whether that capacity gets used.
Improper storage destroying potency
We covered this in the storage section, but it bears repeating. Peptides stored at room temperature lose potency rapidly. Reconstituted peptides left out of the refrigerator degrade within hours. Vials that have been repeatedly frozen and thawed may contain mostly inactive peptide fragments. If your peptide is not working, check your storage practices before blaming the compound. Use the refrigerator storage timeline as your guide and discard anything past its viability window.
Skipping the cycling protocol
Continuous daily use of Epitalon is not how the research was conducted. The protocols that showed results used defined cycles (typically 10 to 20 days) followed by extended breaks (4 to 6 months). The cycling allows the pineal gland to respond to the stimulation and then maintain improved function independently. Running Epitalon continuously is like revving an engine non-stop. It defeats the purpose and may reduce effectiveness. Follow established cycling guidelines for optimal outcomes.
Combining pineal peptides with other sleep-supporting compounds
Pineal peptides do not exist in a vacuum. Researchers often combine them with other compounds that support different aspects of sleep biology. Here are the most evidence-based combinations.
Pineal peptides plus magnesium
Magnesium deficiency affects roughly 50% of the population and directly impairs sleep quality. Magnesium activates GABA receptors, the main inhibitory neurotransmitter system that promotes sleep. Combining magnesium glycinate or threonate (the forms that best cross the blood-brain barrier) with Pinealon creates complementary support, with the peptide handling the melatonin pathway and magnesium handling the GABA pathway. This combination addresses two independent mechanisms of sleep disruption simultaneously.
Pineal peptides plus adaptogens
For stress-related sleep problems, combining DSIP or Pinealon with adaptogenic compounds like ashwagandha or L-theanine can enhance the cortisol-lowering effects. DSIP blocks cortisol release while ashwagandha modulates the HPA axis more broadly. This combination is particularly relevant for people who lie awake with racing thoughts, a pattern driven by evening cortisol elevation that pineal peptides alone may not fully address.
Pineal peptides plus growth hormone secretagogues
Growth hormone is primarily released during deep sleep, creating an interesting synergy with DSIP. By promoting delta-wave sleep, DSIP naturally enhances GH release. Some researchers combine this with growth hormone secretagogues like Ipamorelin or CJC-1295 for amplified recovery and repair during sleep. The rationale is that deeper sleep creates a better environment for GH release, and GH secretagogues ensure the pituitary responds maximally during those deep-sleep windows.
What not to combine
Avoid combining pineal peptides with pharmaceutical sedatives or hypnotics without medical supervision. The mechanisms are different enough that interactions are unpredictable. Similarly, using multiple compounds that all increase serotonin (Pinealon plus high-dose 5-HTP plus an SSRI, for example) could theoretically create excessive serotonergic activity. When in doubt about combinations, consult the peptide safety guidelines and work with a qualified healthcare provider.
Understanding the research limitations
Intellectual honesty demands acknowledging what we do not know, and with pineal peptides, the unknowns are significant.
The Khavinson question
The majority of Epitalon and Pinealon research originates from Professor Vladimir Khavinson research group in Russia. This is not inherently problematic since someone has to do the initial research. But the lack of independent replication is a legitimate concern. At least half of the approximately 110 published articles on Epithalamin and Epitalon are in Russian and unavailable in English translation. Without independent groups confirming these findings in diverse populations, the evidence base remains narrower than ideal.
This does not mean the research is wrong. It means it is unconfirmed by the standards that the broader scientific community considers gold standard. Researchers using these peptides should understand they are working with promising but preliminary evidence, not settled science.
Mechanism gaps
Despite four decades of research, DSIP precise mechanism of action remains unclear. Researchers have yet to isolate the DSIP gene or identify its receptor, leading some to question whether the peptide exists naturally or only under artificial conditions. This is a significant gap that complicates dosing optimization and raises questions about long-term effects that cannot be fully answered yet.
Epitalon mechanism is better understood at the enzymatic level (AANAT upregulation, pCREB activation) but the full picture of how it achieves tissue-specific pineal protection remains unclear. And Pinealon serotonin-stimulating effects have been demonstrated in vitro but comprehensive in vivo dose-response data in humans is still lacking.
Clinical trial limitations
No pineal peptide has undergone the rigorous Phase I through Phase III clinical trial process required for FDA approval. The available human data comes from smaller studies, often unblinded, and primarily from the Khavinson group. While the safety profiles appear favorable (no serious adverse events reported across thousands of subjects), this does not carry the same weight as formal safety studies conducted under regulatory oversight.
For researchers considering these peptides, the practical implication is clear: start conservatively, monitor responses carefully, and do not assume that favorable research results guarantee individual outcomes. This is experimental territory, and treating it otherwise would be irresponsible. The common mistakes guide at SeekPeptides covers additional precautions for anyone new to peptide research.
Practical timeline: what to expect week by week
Setting realistic expectations prevents both premature discontinuation and misinterpretation of results. Here is what the research and clinical experience suggest for a typical pineal peptide sleep protocol.
Week 1: baseline and adjustment
Most researchers report no dramatic changes during the first week. This is normal. The peptides are beginning to interact with pineal cells and neural circuits, but the biological response takes time to manifest. Some people notice subtle shifts, perhaps slightly easier sleep onset or marginally improved morning alertness, but many notice nothing at all. Do not adjust dosing or add additional compounds during this period. Let the baseline protocol establish itself.
Weeks 2 to 3: initial signals
This is when the first consistent changes typically emerge. Sleep onset may become noticeably easier. Morning alertness often improves before subjective sleep quality does, because deep sleep restoration begins benefiting recovery even before you consciously perceive the sleep as better. Dream vividness sometimes increases, suggesting improved REM cycling. If using DSIP specifically, the deep-sleep enhancement effects are usually apparent by this point.
Weeks 4 to 6: meaningful improvement
The majority of positive responders report significant subjective improvement during this window. Sleep feels more restorative. Waking during the night decreases. Energy levels stabilize throughout the day. This corresponds with measurable changes in before and after comparisons that researchers track. If you are tracking sleep with a wearable device, this is typically when the data begins reflecting what you feel subjectively, with increased deep sleep percentages and reduced wake-after-sleep-onset metrics.
Weeks 6 to 12: optimization
The extended phase is about fine-tuning. Pinealon doses may be gradually increased toward the target range. The body circadian rhythm consolidates around the restored melatonin production. Sleep architecture continues to normalize. This is also when the broader health benefits of improved sleep become apparent: better cognitive function, improved mood, enhanced recovery from exercise, and more stable energy.
Post-cycle: the real test
For Epitalon specifically, the weeks and months after an injection cycle are the true measure of effectiveness. If the pineal gland has genuinely been stimulated to restore function, melatonin production and sleep quality should remain improved even after the peptide is discontinued. Most researchers report sustained benefits lasting 4 to 6 months post-cycle, which is why cycles are typically repeated only two to three times annually. This sustained effect is what separates genuine pineal restoration from temporary supplementation.
Specific populations and special considerations
Older adults (60+)
This population stands to benefit the most, but also requires the most caution. Pineal calcification is most advanced, melatonin production most impaired, and the potential for improvement greatest. However, older adults are also more likely to be taking multiple medications, and peptide interactions with common medications for hypertension, diabetes, and cardiovascular disease have not been systematically studied. Start with the lowest recommended doses and increase gradually while monitoring for any unexpected changes.
The Khavinson primate studies are most relevant here: Epitalon increased nighttime melatonin in old monkeys while having no effect on young ones. If you are over 60 and have tried melatonin supplements without satisfactory results, Epitalon approach of restoring endogenous production rather than adding exogenous hormone represents a fundamentally different strategy worth considering with medical guidance.
Women in perimenopause and menopause
Hormonal transitions create unique sleep challenges. Declining estrogen affects thermoregulation (hot flashes), mood regulation, and even melatonin receptor sensitivity. Peptide approaches for perimenopause may benefit from combining pineal peptides with compounds that address the broader hormonal picture. Pinealon neuroprotective properties are particularly relevant for menopausal women experiencing both sleep disruption and cognitive fog, as both conditions share underlying neural mechanisms.
Athletes and recovery-focused users
Sleep quality directly impacts athletic recovery, and deep sleep is when growth hormone release peaks. DSIP promotion of delta-wave sleep naturally enhances this GH window, making it particularly interesting for athletes focused on recovery optimization. Combined with the tissue-repair benefits of compounds like BPC-157 or TB-500, a well-designed sleep protocol can significantly accelerate recovery between training sessions. The peptide stack calculator can help athletes determine compatible combinations.
People with neurodegenerative concerns
Research on the connection between sleep disruption and neurodegenerative disease is growing rapidly. Poor sleep accelerates amyloid-beta accumulation in the brain, and pineal dysfunction is common in Alzheimer disease. A study published in the Journal of Pineal Research documented the decline in pineal melatonin production in relation to Alzheimer disease progression. While no peptide has been shown to prevent or treat neurodegenerative disease, the neuroprotective properties of Pinealon and the pineal-restorative effects of Epitalon represent an area of active research interest for anyone concerned about long-term brain health.
Sourcing and quality considerations
The peptide market is unregulated, and quality varies enormously between suppliers. This matters for any peptide, but it matters especially for compounds targeting the brain and endocrine system. A contaminated or degraded pineal peptide is not just ineffective. It could potentially introduce harmful substances directly into your system.
Key quality indicators to look for include third-party testing with certificates of analysis (COA) showing purity above 98%, proper lyophilization (the powder should be a clean, white cake, not a yellow or clumpy mass), appropriate packaging (amber vials to protect from light degradation), and clear labeling including peptide identity, mass, lot number, and expiration date. The peptide testing labs guide provides details on what to look for in a quality certificate.
Price is a rough indicator but not a reliable one. Extremely cheap peptides are almost certainly compromised, but expensive peptides are not guaranteed to be good. The most reliable approach is purchasing from vendors who provide detailed testing documentation, have established reputations in the research community, and demonstrate transparency about their manufacturing and QA processes. For broader vendor evaluation strategies, the vendor comparison guide covers the key factors to assess.
Storage during shipping also matters. Peptides shipped without cold packs during summer may arrive with reduced potency. Reputable vendors use insulated packaging and cold chain shipping for temperature-sensitive compounds. If your peptide arrives warm, contact the vendor before using it.
Frequently asked questions
Can I take pineal peptides with melatonin supplements?
Yes, but the approach depends on which peptide you are using. Epitalon aims to restore endogenous melatonin production, so adding exogenous melatonin may confuse the feedback mechanisms you are trying to restore. A better strategy is using melatonin during the initial weeks while Epitalon takes effect, then tapering off the supplement as natural production increases. Pinealon and DSIP do not directly conflict with melatonin supplementation and can be used concurrently. Check our peptide stacking guide for more combination considerations.
How long do the effects of pineal peptides last after stopping?
This varies by peptide. Epitalon effects on melatonin production and circadian rhythm typically persist for 4 to 6 months after a 10 to 20 day cycle, which is why cycles are repeated only 2 to 3 times per year. Pinealon neuroprotective effects may last several weeks to months after completing a cycle. DSIP effects are more immediate and shorter-lasting, typically diminishing within days to a week after discontinuation. Understanding peptide timelines helps set realistic expectations.
Are pineal peptides safe for long-term use?
The longest study on pineal peptides (Epithalamin) tracked subjects for 6 to 8 years with annual 10-day treatments. The treatment group showed lower mortality than controls, and no significant adverse effects were reported. However, "long-term" in peptide research is still relatively short compared to pharmaceutical safety monitoring, and the data comes primarily from one research group. The cyclical dosing protocols used in research (short cycles followed by long breaks) inherently limit total exposure. Review the peptide safety guidelines for broader context on long-term considerations.
Do pineal peptides interact with prescription medications?
Formal drug interaction studies have not been conducted for any of the three pineal peptides discussed. DSIP cortisol-lowering effects could theoretically interact with corticosteroids or medications affecting the HPA axis. Epitalon melatonin-boosting effects could interact with drugs that affect melatonin metabolism. Pinealon serotonin effects warrant caution when combined with SSRIs or other serotonergic medications. Always discuss peptide use with a healthcare provider if you are taking prescription medications. The combination safety guide covers general principles for multi-compound protocols.
Which pineal peptide should I start with?
It depends on your primary sleep issue. If you are over 40 and your sleep has gradually worsened with age, Epitalon is the most targeted choice because it directly addresses declining melatonin synthesis. If stress and anxiety drive your sleep problems, Pinealon neuroprotective and serotonin-supporting effects make it the better starting point. If your main complaint is light, non-restorative sleep regardless of duration, DSIP promotion of delta-wave sleep targets that specific deficit. Many researchers eventually use all three in rotation, but starting with one allows you to isolate its effects.
Can younger adults (under 40) benefit from pineal peptides?
Yes, but for different reasons. In younger adults, pineal calcification is typically less advanced and melatonin production remains adequate, so the age-restoration rationale is less relevant. However, younger people dealing with circadian disruption from shift work, jet lag, or chronic stress can benefit from Pinealon circadian gene modulation and DSIP acute sleep-promoting effects. Epitalon is less commonly recommended for younger adults since the primate studies showed no effect in young subjects, suggesting the peptide specifically addresses age-related decline rather than enhancing already-normal function.
How do pineal peptides differ from over-the-counter sleep supplements?
Over-the-counter sleep supplements like melatonin, valerian, magnesium, and L-theanine provide compounds that support sleep through various mechanisms. They are generally safe but work as ongoing supplements that must be taken continuously. Pineal peptides aim to restore underlying biological function so that the body can produce its own sleep-regulating signals without permanent supplementation. This is the fundamental distinction: supplementation versus restoration. Both have their place, and they are not mutually exclusive. Many researchers use peptide protocols alongside foundational supplements.
Is it safe to use pineal peptides with alcohol?
There is no specific research on pineal peptide and alcohol interactions. However, alcohol disrupts sleep architecture (particularly REM sleep), impairs melatonin production, and increases cortisol, essentially working against everything pineal peptides are trying to achieve. Using alcohol during a pineal peptide protocol is not dangerous based on available data, but it undermines the purpose. If you are investing in sleep optimization through peptides, minimizing alcohol consumption, especially in the hours before bed, will significantly improve your outcomes.
External resources
Physiology of the Pineal Gland and Melatonin (NCBI Endotext)
Pineal Calcification, Melatonin Production, Aging, and Rejuvenation (MDPI Molecules)
For researchers serious about optimizing their sleep protocols through pineal peptides, SeekPeptides offers the most comprehensive resource available, with evidence-based guides, proven protocols, community support from thousands of experienced researchers, and personalized dosing calculators that help you build the right protocol for your specific situation.
In case I do not see you, good afternoon, good evening, and good night. May your pineal gland stay restored, your melatonin stay abundant, and your delta waves stay deep.



