Jan 31, 2026
Tired of conflicting information about peptide injection pens? One source says use a syringe. Another swears by autoinjectors. A third tells you the pen is only for semaglutide. And somewhere in the middle of all that noise, you are left holding a vial of reconstituted peptide with no clear answer on the best way to actually inject it. Here is what actually works.
The peptide injection pen has changed the way researchers and patients approach subcutaneous peptide administration. These handheld devices deliver doses with precision that traditional syringes simply cannot match at low volumes. We are talking increments as small as 0.01 mL. That kind of accuracy matters when the difference between an effective dose and a wasted one comes down to fractions of a milliliter. But precision alone does not make a tool worth using. The real advantage of peptide pens lies in their combination of accuracy, ease of use, and reproducibility, three qualities that directly influence whether a peptide protocol delivers results or falls flat.
This guide covers everything you need to know about peptide injection pens. From selecting the right device and needle to mastering the dosing math that trips up even experienced users, from step-by-step injection technique to storage protocols that keep your peptides potent, every section is built on real data and practical experience. Whether you are brand new to peptide research or switching from syringes to a pen system, the information here will save you time, money, and frustration. SeekPeptides has compiled this resource from clinical studies, ISO standards, and the collective knowledge of thousands of researchers who have navigated this exact learning curve.
What is a peptide injection pen
A peptide injection pen is a handheld device designed to deliver precise subcutaneous doses of peptide solutions through a fine needle. Think of it as the modern evolution of the insulin syringe. Same destination. Far better engineering.
These devices originated in the diabetes world, where insulin pens replaced vial-and-syringe setups decades ago. The technology proved so effective that it expanded into other injectable therapies, including growth hormones, GLP-1 receptor agonists, and research peptides. The core principle remains consistent across all applications. A mechanical or spring-loaded mechanism pushes a measured volume of solution through a short, ultra-fine needle into the subcutaneous fat layer just beneath the skin.
What separates a peptide pen from a standard insulin syringe is the delivery mechanism itself. With a syringe, you manually draw fluid from a vial, estimate the volume by reading tiny markings on a barrel, and push the plunger with your thumb while trying to maintain a steady angle. With a pen, you dial a dose, press a button, and the device handles the rest. The precision comes from engineering, not from your ability to read a graduation line at arm length while pinching skin with your other hand.
How peptide pens differ from traditional syringes
The differences go deeper than convenience. Traditional insulin syringes measure volume in units. A U-100 syringe reads 100 units per milliliter. That works perfectly for insulin, which is standardized at known concentrations. But peptides are not insulin. They come in varying amounts, get reconstituted at different concentrations, and require dose calculations that translate micrograms into volume. This mismatch between the syringe markings and the actual dose creates a gap where errors thrive.
Pen injectors close that gap. Modern devices offer dose increments as fine as 0.01 mL, and the dial mechanism provides tactile and visual confirmation of the selected dose. You feel each click. You see the number. There is no squinting at tiny lines on a plastic barrel.
Research supports this advantage. A study published in Diabetes Care found that pen injectors were significantly more accurate than insulin syringes at low doses, where small volume errors translate to large percentage differences in the actual amount delivered. For peptide researchers working with doses of 100 to 500 mcg, where the injection volume might be 0.04 to 0.2 mL, this accuracy difference is not trivial. It is the difference between a consistent protocol and a guessing game.
The two main categories
Peptide pens fall into two broad categories based on their injection mechanism.
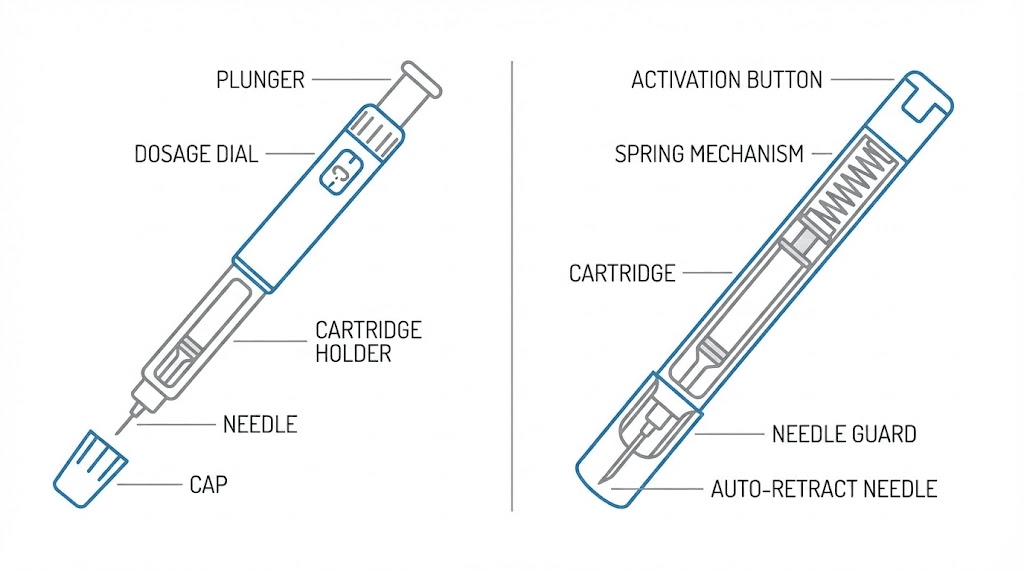
Manual pen injectors require you to press a button or push a plunger to deliver the dose. You control the speed and force of injection. These are the most common type for peptide research because they accommodate different cartridge sizes and dose ranges. They give you control over the injection process while still providing the precision of a dial-based dosing system.
Autoinjectors use a spring-loaded mechanism that triggers when you press the device against your skin or push a button. The spring drives the needle in, delivers the dose, and retracts the needle, all in one motion. The semaglutide pen used in weight management is a well-known example. A usability study of the semaglutide single-dose pen-injector found a mean ease-of-use rating of 6.9 out of 7.0, with no serious use errors even among participants who received zero training before their first injection. That is the kind of user-friendliness that changes adoption rates.
Within those two categories, you also find reusable pens and disposable pens. Reusable pens accept replaceable cartridges and use fresh pen needles for each injection. Disposable pens come pre-filled and get discarded after the medication runs out. For peptide research, reusable pens with refillable cartridges offer the most flexibility since you can reconstitute your own peptides and load them into standard 3 mL cartridges.
Why peptide pens are replacing traditional syringes
The shift from syringes to pens is not a trend. It is a response to measurable problems with the old way of doing things.
Precision dosing advantages
Accuracy at low volumes is where pens truly separate themselves. A standard 1 mL insulin syringe has graduation marks every 0.01 mL, but reading those marks accurately at the small volumes common in peptide dosing requires excellent vision and steady hands. At 0.05 mL, you are working with a volume smaller than a single drop of water. The margin for visual error on a syringe barrel at that volume is enormous relative to the dose.
Pen injectors eliminate this problem mechanically. The dial clicks in fixed increments, and each increment corresponds to a precise volume. ISO 11608 standards require pen injectors to deliver doses within tight accuracy specifications. Testing validates dose delivery down to increments of 0.01 mL. When your BPC-157 protocol calls for exactly 250 mcg and your reconstitution concentration is 5,000 mcg per mL, you need to deliver exactly 0.05 mL. A pen makes that straightforward. A syringe makes it a test of your eyesight.
You can verify your own concentrations and volumes using the peptide calculator before loading your pen, which further reduces the chance of a dosing mistake.
Ease of use and compliance
Compliance matters more than most people realize. The best protocol in the world fails if you skip doses because the injection process feels like a chore, or worse, something you dread.
Studies on insulin delivery show the scale of this effect. In one review of 29 studies, more than 66 percent of patients preferred pen injectors over vial-and-syringe setups. In 8 of 9 studies assessing pain, more than 50 percent of patients said the pen caused less pain. And in 10 of 12 studies assessing acceptability, over 75 percent rated the pen as more acceptable than the traditional approach. Those numbers translate directly to compliance. Among pen users in one study, 22.2 percent achieved optimal glycated hemoglobin levels compared to just 2.2 percent among syringe users, a statistically significant difference driven largely by better adherence.
For peptide researchers running protocols that last weeks or months, these compliance advantages compound. Missing one injection of BPC-157 during a six-week healing protocol might not matter. Missing several because the injection process is intimidating or inconvenient absolutely does.
Comfort and reduced needle anxiety
Needle anxiety is real. It affects an estimated 20 to 25 percent of adults, and it is one of the most common reasons people avoid or delay injectable therapies. Pen injectors address this problem in several ways.
The needle is hidden inside the device until the moment of injection. You do not see it sitting exposed on a syringe barrel while you prepare. The injection depth and speed are controlled by the device rather than by your shaking hand. And the pen needles themselves, typically 30G or 31G in 4 to 5 mm lengths, are so fine that many users describe the sensation as barely noticeable.
Compare that to the process of drawing from a vial with a larger needle, switching to an injection needle, finding your site, and pushing the plunger while maintaining angle and depth. The pen simplifies every step. For anyone who has ever hesitated with a syringe poised over their abdomen, the pen offers a legitimate path past that hesitation. It also helps when traveling, since peptide pens are more discreet and less intimidating at airport security than a bag of syringes and vials.
Types of peptide injection pens explained
Not all pens serve the same purpose. Understanding the differences helps you select the right device for your specific peptide protocol.
Manual pen injectors
Manual pens are the workhorse of the peptide research community. You dial your dose, place the pen against your skin, and press the injection button yourself. The plunger advances at whatever speed and force you apply.
This manual control has advantages. You can inject slowly, which reduces discomfort with larger volumes. You can pause mid-injection if needed. You feel the resistance and can adjust accordingly. For researchers who want full control over every aspect of their injectable peptide protocol, manual pens deliver that control with better precision than a syringe.
Most reusable manual pens accept standard 3 mL cartridges, which you fill yourself from reconstituted peptide vials. This flexibility makes them compatible with virtually any peptide that can be administered subcutaneously. The dose dial typically ranges from 0.01 mL to 0.60 or 0.70 mL per injection, covering the volume range needed for most peptide protocols.
Autoinjectors
Autoinjectors do the work for you. Press the button or push against your skin, and a spring mechanism inserts the needle, delivers the dose, and retracts the needle in one smooth motion. The entire process takes seconds.
The trade-off is flexibility. Most autoinjectors deliver a fixed dose from a pre-filled cartridge. You cannot adjust the amount. This makes them ideal for standardized medications like semaglutide or tirzepatide, where the dose is set by a prescriber and does not change between injections. For peptide research protocols that require dose adjustments, autoinjectors are less practical unless you have access to multiple pre-filled options at different dose levels.
The usability data for autoinjectors is impressive, though. In the STEP 8 phase III trial for semaglutide 2.4 mg, participants self-injected 3,864 times with only 22 reported errors, most of which were minor observations of liquid on the skin. Between 87 and 93 percent of users agreed that the pen fit well into their everyday routine.
Reusable versus disposable
Reusable pens accept fresh cartridges and new pen needles for each use. The pen body itself lasts for months or years. You replace the cartridge when it empties and attach a new needle for each injection. This is the most cost-effective option for ongoing peptide research.
Disposable pens come pre-loaded and get discarded when the medication runs out. They require no loading, no cartridge changes, and no maintenance. They are the simplest option but offer no flexibility in concentration or peptide selection. Pharmaceutical semaglutide pens and tirzepatide pens are common examples.
For researchers working with multiple peptides like TB-500, Ipamorelin, and CJC-1295, a reusable pen with multiple labeled cartridges provides the best combination of precision and versatility.
Pre-filled versus refillable
Pre-filled pens arrive ready to use. The medication is already in the cartridge at a known concentration. Dial and inject. No reconstitution, no calculations, no loading steps.
Refillable pens require you to reconstitute the peptide, calculate the concentration, transfer the solution into an empty cartridge, and load that cartridge into the pen. More steps. More room for error. But also more control over what goes in, how concentrated it is, and which peptides you use. For anyone running custom stacks involving peptides like BPC-157, TB-500, and GHK-Cu, the refillable option is the only practical choice. The peptide reconstitution calculator takes the guesswork out of the preparation step.
How to use a peptide injection pen step by step
The process has more steps than a simple syringe injection, but each step exists for a reason. Skip one, and you compromise either safety or accuracy. Do them all, and you get reliable results every time.
Step one: reconstitution
Most research peptides arrive as lyophilized powder, a freeze-dried form that must be mixed with a solvent before injection. This step happens before you ever touch the pen.
Start with a clean workspace. Wash your hands thoroughly. Wipe the rubber stoppers of both the peptide vial and the bacteriostatic water vial with separate alcohol swabs. Let them dry.
Calculate your desired concentration. If your vial contains 5 mg of peptide and you add 2 mL of bacteriostatic water, your concentration will be 2,500 mcg per mL (since 5 mg equals 5,000 mcg). The peptide dosage calculation guide walks through this math in detail, and you can double check your numbers with the peptide calculator.
Draw the bacteriostatic water into a syringe using a 21G or 23G needle. Insert the needle through the rubber stopper of the peptide vial and aim the stream of water down the inside wall of the glass. Never blast the water directly onto the powder. That can damage the peptide structure. Let the water run gently down the side.
Once all the water is in the vial, do not shake it. Gently swirl or roll the vial between your palms until the powder dissolves completely. Some peptides dissolve in seconds. Others need 5 to 15 minutes of patient swirling. If it has not dissolved after 15 minutes, place the vial in the refrigerator for a few hours and try again. Refer to the complete mixing guide if you run into solubility issues.
Step two: loading the pen cartridge
With your peptide fully dissolved, it is time to transfer the solution from the vial into a pen cartridge.
Sanitize the top of a sterile 3 mL pen cartridge with an alcohol swab. Insert a small vent needle (27G works well) through the rubber stopper of the cartridge. This vent allows air to escape as you inject fluid in. Without it, the increasing pressure inside the cartridge can crack the glass or push the plunger out.
Using a syringe with a 21G needle, draw the reconstituted peptide from the vial. Insert the syringe needle into the cartridge stopper alongside the vent needle. Slowly inject the solution into the cartridge, angling the needle so the fluid runs down the glass wall rather than spraying into the air space. Take your time here. Rushing creates bubbles.
Once the fluid is in, gently tap the cartridge to bring any air bubbles to the top. Remove the vent needle first, then the syringe needle. The cartridge is now loaded and ready for the pen.
Step three: assembling and priming the pen
Open the pen by unscrewing the cartridge holder from the pen body. If the plunger rod is extended, push it back until it sits flush. Insert the loaded cartridge, then screw the holder back onto the pen body until it is snug.
Attach a fresh pen needle. These typically twist on until finger-tight. Remove both the outer and inner needle caps. Hold the pen with the needle pointing up.
Now prime. Dial up 1 to 2 units (or the minimum dose increment) and press the injection button while holding the pen upright. You should see a small droplet of fluid appear at the needle tip. This confirms that the pen is delivering solution and that air has been expelled from the needle assembly. If no droplet appears, repeat the priming step. Do not skip this. Injecting air instead of peptide is a waste and a safety concern.
Step four: choosing your injection site
Subcutaneous injection sites for peptides include the lower abdomen (at least two inches from the navel), the outer thigh (middle third), and the upper outer arm. The abdomen tends to be the most popular choice because of its accessibility and consistent fat layer. The peptide injection guide covers site selection in depth.
Rotate your injection sites. Never inject in the same spot twice in a row. Move at least 1 to 2 centimeters from your last injection point. Repeated injections in the same area can cause lipohypertrophy, a buildup of fatty tissue that looks like a small lump and can affect peptide absorption rates unpredictably.
Clean the selected site with an alcohol swab. Let it air dry completely. Injecting through wet alcohol stings and can push contaminants into the skin.
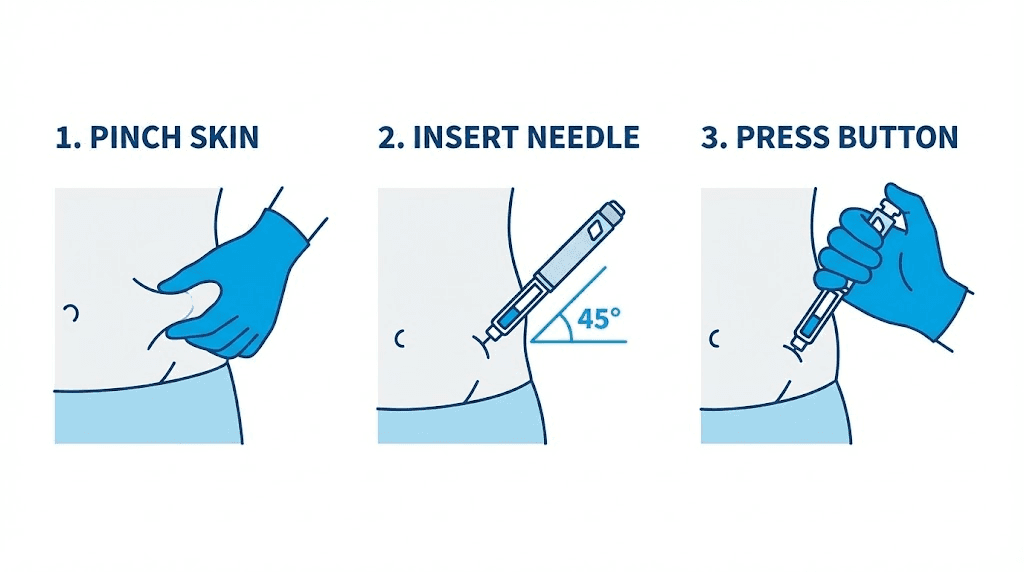
Step five: injection technique
Dial your calculated dose on the pen. The numbers should be clearly visible through the dose window.
Pinch a fold of skin at your chosen site. This lifts the subcutaneous fat layer away from the muscle beneath it, creating a clear target zone. With short pen needles (4 to 5 mm), you can insert at a 90-degree angle directly into the pinched skin fold. With longer needles (6 to 8 mm) or if you have very low body fat, insert at a 45-degree angle to stay in the subcutaneous layer and avoid hitting muscle. Understanding the difference between injectable and oral peptide delivery helps explain why proper subcutaneous placement matters for absorption.
Insert the needle smoothly. Do not jab or hesitate. Press the injection button firmly and hold it down. Count slowly to ten before removing the needle. This dwell time allows the full dose to be delivered and prevents solution from leaking back out through the needle track. In the semaglutide usability study, this step alone accounted for most of the minor use errors, where participants removed the needle too quickly and noticed fluid on the skin.
Withdraw the needle at the same angle you inserted it. Do not rub the injection site. A small dot of blood is normal and nothing to worry about. If you see a drop of fluid at the site, the needle may not have been held in long enough. Extend your count to 15 next time.
Step six: post-injection care
Remove the pen needle immediately after injection. Do not leave it attached to the pen between uses. An attached needle creates a pathway for air to enter the cartridge and for fluid to leak out, both of which affect your next dose. Dispose of used needles in a proper sharps container.
Replace the pen cap. Store the pen with its loaded cartridge in the refrigerator if it contains reconstituted peptide. Keep it upright if possible to minimize air bubble formation near the cartridge stopper. The peptide storage guide covers temperature and duration requirements for various peptides.
Choosing the right needle for your peptide pen
The needle matters more than most people think. Too thick, and every injection hurts. Too thin, and viscous solutions will not flow properly. Too short, and you might not reach the subcutaneous layer. Too long, and you risk injecting into muscle. Getting it right makes the entire experience better.
Understanding needle gauge
Gauge refers to the diameter of the needle. Here is the counterintuitive part: higher gauge numbers mean thinner needles. A 31G needle is thinner than a 29G. A 32G is thinner still. For subcutaneous peptide injections, the usable range runs from 29G to 32G.
Thinner needles cause less pain. That is not debatable. Research consistently shows that higher-gauge needles result in lower pain scores. But thinner needles also have smaller internal diameters, which means fluid flows through them more slowly and more force is needed to push the injection button. For the volumes used in peptide research (typically 0.05 to 0.5 mL), this is rarely an issue. The solution is water-based and flows easily through even a 32G needle.
Gauge and length guide by body type
Your body composition determines the optimal needle length. The goal is to deposit the peptide into the subcutaneous fat layer, which sits between the skin surface and the underlying muscle.
32G x 4mm: Best for lean to average body fat. The 4mm length keeps the injection comfortably in the subcutaneous zone without any risk of reaching muscle. This is the most popular choice for peptide researchers with low to moderate body fat. Virtually painless for most users.
31G x 5mm: Ideal for individuals with slightly more subcutaneous fat. The extra millimeter of length ensures full penetration into the fat layer. Still extremely comfortable. Good all-around choice if you are unsure about your body fat level.
30G x 6mm: Suitable for thicker fat layers, particularly in the abdominal area. The slightly larger gauge means marginally more sensation on insertion, but the difference is minimal. Good for injection sites with more tissue depth like the outer thigh.
30G x 8mm: Reserved for individuals with significant subcutaneous fat or for injection sites where extra length is needed to reach the target layer. Use a 45-degree insertion angle with this length to avoid intramuscular delivery if the site has a thinner fat pad.
For most peptide researchers using abdominal injection sites, the 31G x 5mm needle represents the best balance of comfort, reliability, and universal fit. You can explore the full range of injection equipment options in our detailed guide, which covers both pen needles and traditional syringe needles.
When to use which needle
Match the needle to the situation, not just your body type.
For daily peptide protocols like BPC-157 dosing where you inject once or twice per day, prioritize comfort. Go with the thinnest, shortest needle that reliably reaches subcutaneous tissue. A 32G x 4mm makes daily injections feel routine rather than daunting.
For weekly injections at larger volumes, such as a TB-500 loading dose of 0.5 to 0.7 mL, a slightly larger gauge like 30G allows the fluid to flow faster and reduces the time you spend holding the pen in place. The injection frequency is low enough that the marginal comfort difference does not matter as much.
For rotating between multiple injection sites, consider having two needle options. A shorter needle for lean sites like the abdomen and a longer one for thicker areas like the outer thigh or flank. This ensures consistent subcutaneous delivery regardless of site.
Peptide pen dosing math explained
This section saves protocols. Dosing math is where most errors happen, and most errors happen because people confuse units, micrograms, milligrams, and milliliters. Let us clear that up permanently.
Understanding units versus mcg versus mg versus mL
These four measurements describe different things. Mixing them up is the single most common peptide dosing mistake.
mg (milligrams) and mcg (micrograms) measure mass. How much peptide substance you have. One milligram equals 1,000 micrograms. A vial labeled 5 mg contains 5,000 mcg of peptide.
mL (milliliters) measures volume. How much liquid. When you add 2 mL of water to a 5 mg vial, you now have 2 mL of solution.
Units are where confusion explodes. On a U-100 insulin syringe, 100 units equals 1 mL. So 10 units equals 0.1 mL, and 1 unit equals 0.01 mL. Units are just another way to express volume on insulin syringes. They are not a universal measure of peptide dosage. When someone says they injected 10 units of BPC-157, they mean they injected 0.1 mL. How much BPC-157 that actually contains depends entirely on the concentration.
Pen injectors typically display the dose in mL rather than units, which eliminates one layer of confusion. But you still need to know your concentration to translate between the mL on the pen dial and the mcg your protocol calls for.
The concentration formula
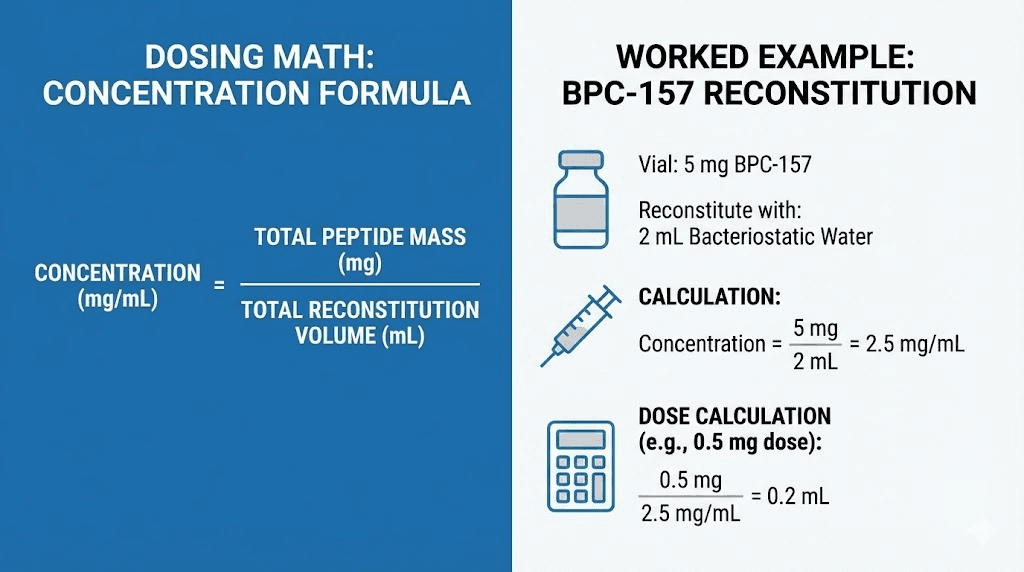
Every peptide dosing calculation starts with concentration. The formula is simple.
Concentration (mcg/mL) = Total Peptide (mcg) divided by Water Volume (mL)
Example: You have a 5 mg vial of BPC-157 (that is 5,000 mcg). You add 2 mL of bacteriostatic water. Your concentration is 5,000 divided by 2, which equals 2,500 mcg/mL.
To find out how much volume to inject for a specific dose:
Volume to inject (mL) = Desired Dose (mcg) divided by Concentration (mcg/mL)
If your protocol calls for 250 mcg of BPC-157 and your concentration is 2,500 mcg/mL, you need to inject 250 divided by 2,500, which equals 0.1 mL. On your pen, dial to 0.10 mL. Simple.
The peptide calculator does this math instantly for any peptide, any vial size, and any reconstitution volume. Use it every time. Even experienced researchers double check their math because one decimal place error means a ten-fold dosing mistake.
Worked examples for common peptides
Let us walk through the math for several popular peptides to make the process concrete.
BPC-157 (5 mg vial, targeting 250 mcg per dose): Add 2 mL bacteriostatic water. Concentration becomes 2,500 mcg/mL. For 250 mcg, inject 0.10 mL. The BPC-157 dosage calculator confirms this and shows how different reconstitution volumes change the injection amount.
TB-500 (5 mg vial, targeting 2,000 mcg per dose): Add 2 mL bacteriostatic water. Concentration becomes 2,500 mcg/mL. For 2,000 mcg (2 mg), inject 0.80 mL. That is a larger volume, which is why the TB-500 dosage calculator can help you plan reconstitution volumes that keep injection sizes manageable. If you add only 1 mL of water instead, the concentration jumps to 5,000 mcg/mL, and the dose volume drops to 0.40 mL, which is more comfortable to inject.
Ipamorelin (5 mg vial, targeting 300 mcg per dose): Add 2.5 mL of bacteriostatic water. Concentration becomes 2,000 mcg/mL. For 300 mcg, inject 0.15 mL. A small, comfortable volume.
CJC-1295 (2 mg vial, targeting 100 mcg per dose): Add 2 mL of water. Concentration is 1,000 mcg/mL. For 100 mcg, inject 0.10 mL. The CJC-1295 dosage calculator helps plan these numbers for different vial sizes and dose targets.
Semaglutide (varies by product): Pharmaceutical semaglutide pens come pre-filled at specific concentrations, and the pen dial is calibrated to deliver the dose in mg directly. No math required. But if working with research-grade semaglutide, the same concentration formula applies. The semaglutide dosage calculator handles both scenarios.
Common dosing mistakes to avoid
Mistake number one: confusing mg and mcg. Injecting 250 mg instead of 250 mcg would be 1,000 times the intended dose. Always confirm your units before dialing. Always.
Mistake number two: using insulin syringe units as if they represent a universal dose. When a forum post says "I inject 10 units of BPC-157," that person means 0.1 mL. How much BPC-157 that represents depends on their reconstitution concentration. If their concentration is 2,500 mcg/mL, 10 units is 250 mcg. If their concentration is 5,000 mcg/mL, 10 units is 500 mcg. Same syringe reading, very different doses.
Mistake number three: not accounting for priming volume. When you prime your pen, you expel a small amount of solution. Over an entire cartridge, these priming losses add up. Account for them when calculating how many doses you will get from a single reconstitution.
Mistake number four: assuming all pen dials read the same way. Some pens display dose in mL. Others display in arbitrary dial units that you must convert using the included instructions. Always read the pen manual before your first use. For precise calculations across any scenario, rely on the peptide dosage calculation guide.
Which peptides work best with injection pens
Not every peptide is a perfect fit for pen delivery. The ideal candidates share certain characteristics: they are administered subcutaneously, the dose volume falls within the pen range of 0.05 to 0.70 mL, and they are stable in solution long enough to use from a cartridge over multiple days.
BPC-157
BPC-157 is perhaps the most natural fit for a peptide pen. Typical doses of 200 to 300 mcg result in injection volumes of 0.04 to 0.12 mL depending on reconstitution concentration, well within the precision range of any quality pen. The peptide is usually administered once or twice daily, making the speed and convenience of a pen particularly valuable. Researchers using BPC-157 for tendon repair, joint support, or gut health applications find the pen system especially practical for consistent daily dosing.
TB-500
TB-500 works well with pens during maintenance dosing phases, where volumes are moderate. Loading doses of 2 to 2.5 mg can push volume higher (0.4 to 0.8 mL depending on concentration), which approaches the upper limit for comfortable subcutaneous injection. Consider reconstituting at higher concentrations if you plan to use a pen for TB-500 loading. During maintenance phases at lower doses, the pen is ideal. The BPC-157 versus TB-500 comparison explores the differences between these two popular healing peptides and how they can work together in the Wolverine stack.
Ipamorelin and CJC-1295
Growth hormone secretagogues like Ipamorelin and CJC-1295 are excellent pen candidates. Dose volumes are typically small (0.05 to 0.20 mL), and these peptides are usually administered daily or multiple times per day. The convenience of a pen versus preparing a syringe from a vial at bedtime cannot be overstated. These peptides are commonly used for muscle growth, fat loss, and anti-aging protocols. The Ipamorelin versus CJC-1295 comparison helps determine which secretagogue fits your goals.
Semaglutide
Semaglutide is the peptide that brought injection pens into mainstream awareness. The pre-filled weight loss peptide pens require no preparation whatsoever. Dial, inject, done. For those using research-grade semaglutide, a refillable pen with proper reconstitution works well. The weekly dosing schedule means each cartridge lasts a long time. Compare the benefits and differences using the semaglutide dosage calculator and the semaglutide versus tirzepatide comparison.
GHK-Cu
GHK-Cu injection protocols typically involve small volumes, making this copper peptide a good pen candidate. The main consideration is that GHK-Cu can be administered via multiple routes, including subcutaneous injection, topical application, and even nasal delivery. For injection-based protocols targeting skin rejuvenation, hair regrowth, or systemic anti-aging effects, a pen provides consistent dosing. Refer to the GHK-Cu reconstitution guide for preparation specifics.
Other compatible peptides
Several other peptides work well with pen delivery systems. Sermorelin for growth hormone support, KPV for inflammatory conditions, Selank for cognitive and anxiety support, and PT-141 for libido enhancement all fall within the dose and volume ranges that pens handle efficiently. The complete peptide list shows every peptide currently used in research and identifies which ones are commonly administered subcutaneously.
For multi-peptide protocols, keep each peptide in its own labeled cartridge. Never combine different peptides in a single cartridge unless you have verified compatibility. The peptide stack calculator helps plan combination protocols while the peptide stacking guide covers compatibility in detail.
Peptide pen versus insulin syringe comparison
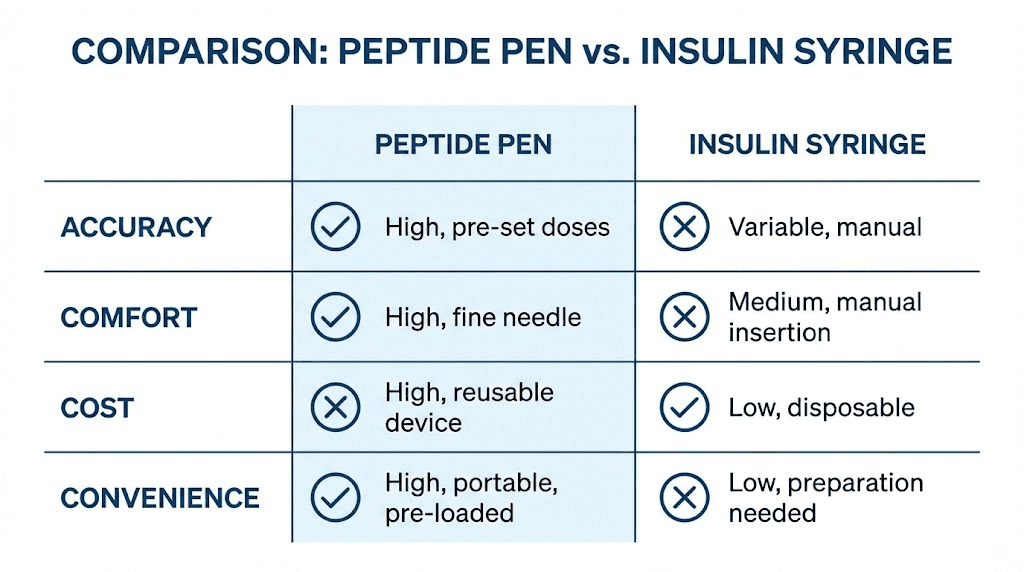
Both tools deliver peptides subcutaneously. Both work. But they are not equal in practice, and knowing where each excels helps you make the right choice for your specific situation.
Detailed comparison
Dosing accuracy: Pen injectors are more accurate at low volumes. Research confirms this consistently. At doses below 5 units (0.05 mL), the percentage error on a syringe becomes significant. Pens maintain accuracy across their entire dial range because the mechanical mechanism delivers a fixed volume per click regardless of how well you can read the barrel markings. For anyone following a precise peptide dosage chart, the pen gives you confidence that what the chart says is what your body actually receives.
Ease of use: Pens require fewer manual steps. No drawing from a vial. No switching needles. No reading graduation marks. Dial and press. Multiple studies confirm that patients learn pen technique faster and make fewer errors. The learning curve matters because errors during the learning phase can mean wasted peptide and inconsistent results.
Pain and comfort: Pen needles tend to be shorter and finer than standard insulin syringe needles. The hidden needle reduces anxiety. The spring or mechanical delivery means you do not have to simultaneously hold the device, maintain angle, and push a plunger. Less multitasking means more comfort.
Portability: A pen fits in a pocket or bag more discreetly than a syringe-and-vial kit. No loose needles, no vials to protect from breaking, no alcohol swabs for vial prep. For researchers who travel or need to inject away from home, pens simplify the logistics considerably.
Flexibility: This is where syringes have an advantage. A syringe can draw from any vial at any concentration with no cartridge loading required. Need to switch peptides? Grab a new syringe. Need an unusual volume? Any syringe from 0.3 mL to 1.0 mL covers it. Pens require cartridge prep and are limited to one peptide per cartridge.
Cost: Syringes are cheaper per injection. A box of 100 insulin syringes costs a fraction of a reusable pen plus pen needles. However, cost analysis must include the value of accuracy. Wasting peptide through imprecise syringe dosing can cost more over a protocol cycle than the pen investment. The peptide cost calculator helps quantify the full cost picture including waste and reconstitution efficiency.
Smaller syringes bridge the gap
If you prefer syringes but want better accuracy, consider smaller barrels. A 0.3 mL syringe has graduation marks closer together than a 1.0 mL syringe, making small volumes easier to read accurately. For peptide doses requiring less than 0.3 mL, these micro syringes significantly improve precision compared to standard 1.0 mL insulin syringes. They do not match the mechanical precision of a pen, but they narrow the gap considerably. Learn more about choosing between injectable and oral peptide delivery methods.
When each is the better choice
Choose a pen if you inject daily or more frequently, if your doses are small and precision matters most, if needle anxiety is an issue, if you value convenience and portability, or if you are committed to a long-term protocol where consistency determines outcomes.
Choose a syringe if you inject infrequently (weekly or less), if you use many different peptides and switching cartridges would be impractical, if cost is the primary concern and you have steady hands with good vision, or if your doses are large enough that syringe accuracy is adequate.
Many experienced researchers use both. Pens for their primary daily peptides. Syringes for occasional or one-off injections. There is no rule that says you must commit to one method exclusively.
Storage and maintenance for peptide pens
Proper storage protects both the pen mechanism and the peptide inside the cartridge. Neglect either one, and you compromise your protocol.
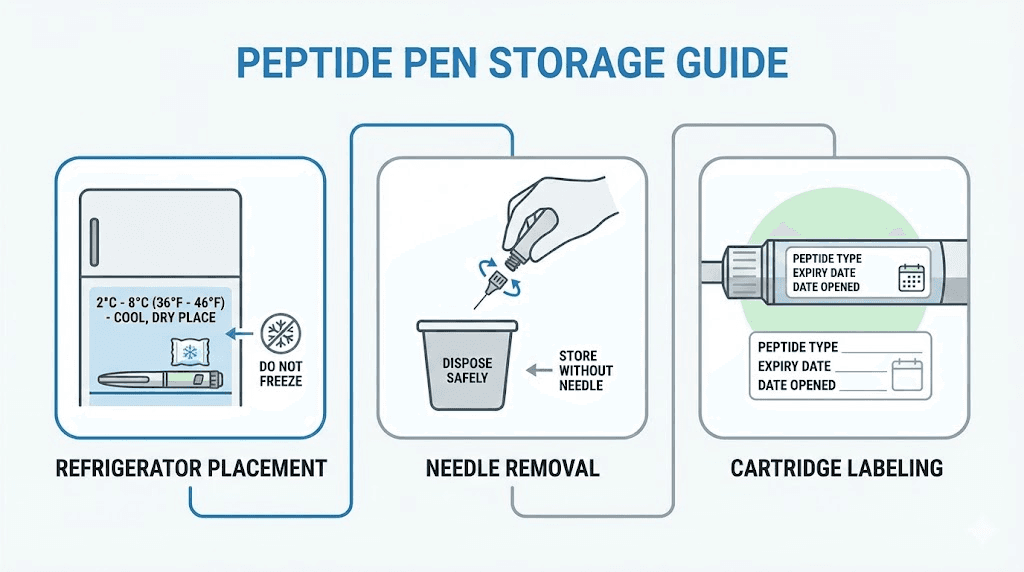
Reconstituted peptide storage
Reconstituted peptides are fragile. Once that lyophilized powder meets bacteriostatic water, the clock starts. Most reconstituted peptides remain stable for three to four weeks when stored at 2 to 8 degrees Celsius (36 to 46 degrees Fahrenheit) in a standard refrigerator. The reconstituted peptide shelf life guide provides specific timelines for different peptides.
Never freeze reconstituted peptides unless the specific protocol permits it. Freezing can cause peptide aggregation and loss of potency. Room temperature exposure should be minimized as well. The room temperature stability guide explains how quickly degradation occurs outside refrigeration.
When a peptide is loaded in a pen cartridge, the same storage rules apply. Keep the pen in the refrigerator with the cartridge installed but the needle removed. This maintains peptide potency while preventing the needle channel from acting as a contamination pathway. For information about unreconstituted peptide storage, the powder form stability guide and the general fridge storage guide cover the essentials.
Pen cleaning and care
The pen body itself requires minimal maintenance. Wipe the exterior with a clean, dry cloth if it gets dirty. Do not submerge the pen in water or use chemical cleaners on the mechanism. The dial, button, and plunger assembly are engineered to tight tolerances, and liquid intrusion can cause malfunction.
Check the cartridge holder threading periodically. If the cartridge does not seat firmly, the seal may be compromised, and air can enter the system. Replace the pen body if the dial mechanism feels loose, skips clicks, or does not return to zero after a full injection. Mechanical precision is the whole point of using a pen. A worn mechanism defeats that purpose.
Between cartridge changes, inspect the plunger seal inside the pen body. A clean, intact seal ensures consistent dose delivery. If you notice the plunger sticking or moving unevenly, contact the pen manufacturer for replacement parts.
Traveling with peptide pens
Peptide pens are significantly more travel-friendly than syringe kits. The pen looks like a common medical device (insulin pen), which reduces questions at security checkpoints. Keep your peptides in a small insulated cooler bag with an ice pack to maintain refrigeration temperature during transit.
Pack pen needles in their sealed packaging. Carry a sharps disposal container for used needles. If traveling by air, keep the pen and supplies in your carry-on rather than checked luggage. Temperature extremes in cargo holds can damage peptides. A letter from a prescribing healthcare provider can be helpful for international travel, though domestic travel with medical injection devices rarely raises issues.
Know the peptide expiration considerations before any extended trip. If your reconstituted peptide will be more than three weeks old by the time you return, consider bringing unreconstituted vials and mixing supplies instead. The lyophilized versus liquid peptide comparison explains why unreconstituted powder is more stable for travel.
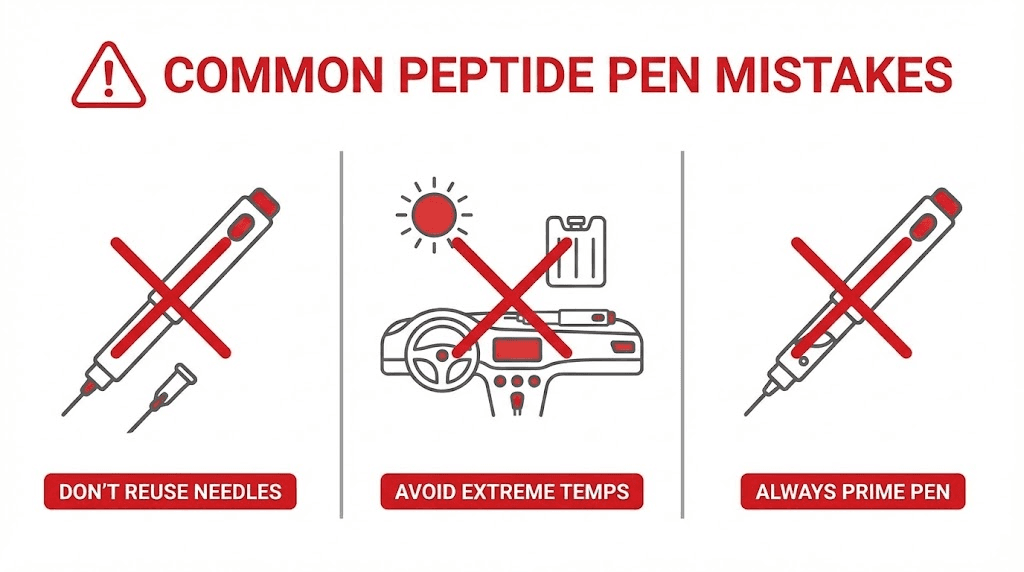
Common mistakes with peptide injection pens
Even with a precision tool, human error finds a way. These are the mistakes that derail protocols most often, and every single one is avoidable.
Dosing errors
The most dangerous mistake is calculating the wrong concentration. If you add 1 mL of water to a 5 mg vial instead of the intended 2 mL, your concentration doubles. Every injection delivers twice the intended dose. This seems obvious on paper, but it happens regularly, especially when someone changes their reconstitution volume and forgets to recalculate their dial setting. Use the peptide calculator every time you reconstitute, even if you have done it a hundred times before.
Another common error is forgetting to account for pen priming. Each time you prime the pen, you lose a small amount of solution. Over 20 or 30 doses from a single cartridge, those losses can add up to one or two full doses. Plan your reconstitution volume accordingly.
Reading the dose dial incorrectly happens more often than people admit. Some pens display increments that look similar at different settings. Double check the number in the dose window before every injection.
Needle reuse
A fresh needle for every injection. No exceptions.
Pen needles are designed for single use. After one insertion, the needle tip begins to dull and develop microscopic barbs. Reusing a needle increases pain, causes more tissue trauma, and raises infection risk. It also introduces contaminants into the cartridge, which can degrade the remaining peptide.
Some researchers reuse needles to save money. This is a false economy. A box of 100 pen needles costs far less than the peptide that a contaminated cartridge would ruin. Protect your investment. Use a fresh needle every time. The peptide safety guide covers this and other critical safety practices.
Improper storage
Leaving the pen with a cartridge of reconstituted peptide on the kitchen counter for hours while you go about your day is a surprisingly common habit. Each hour at room temperature reduces peptide potency. Some peptides degrade noticeably within just a few hours outside refrigeration.
Another storage mistake is leaving the needle attached between uses. An attached needle allows temperature changes to create a pumping effect that draws air into the cartridge and pushes small amounts of solution out. Over days, this can significantly alter the volume and concentration in the cartridge, throwing off your carefully calculated doses.
Store your pen in the refrigerator, needle removed, cap on. Simple. Effective. Non-negotiable. For a complete breakdown of how storage conditions affect different peptides, review the peptide storage guide.
Not priming before injection
Skipping the priming step means your first injection might deliver a mixture of air and solution rather than a full dose of peptide. Air bubbles in the cartridge or needle assembly are normal. Priming pushes them out. Skip this step, and you inject air, which wastes a dose and could cause a small subcutaneous air pocket at the injection site.
Prime the pen every time you attach a new needle. If you suspect air has entered the cartridge (after a temperature change or rough handling), prime again before your next injection. The few seconds this takes are worth the certainty that your dose is accurate and complete.
Safety and best practices
Precision dosing means nothing if the injection itself introduces contamination, damages tissue, or violates basic safety principles. Good technique protects both you and your peptide supply.
Sterile technique
Start every injection session with clean hands. Wash with soap and water for at least 20 seconds. This is not excessive caution. It is the minimum standard for any procedure that breaks the skin barrier.
Clean the injection site with an alcohol swab using firm, circular strokes from the center outward. Let the alcohol dry completely before inserting the needle. Injecting through wet alcohol causes stinging and can push bacteria or alcohol into the subcutaneous tissue.
Never touch the needle after removing the cap. If you accidentally contaminate the needle by touching it, brushing it against clothing, or dropping the cap, replace it with a fresh one. The few cents a new needle costs is nothing compared to the risk of a subcutaneous infection.
When loading cartridges, maintain sterile technique throughout. Wipe rubber stoppers with alcohol. Use fresh needles for drawing from vials. Work on a clean surface. These habits protect the entire batch of reconstituted peptide, not just a single injection. The comprehensive safety guide covers sterile protocols for every stage of peptide handling.
Injection site rotation
Rotate. Every. Time.
Repeated injections in the same spot cause lipohypertrophy, scar tissue formation, and erratic absorption. The abdomen alone offers dozens of potential injection points when you maintain a grid pattern with 1 to 2 centimeters between sites. Add the outer thighs and upper arms, and you have weeks of unique injection locations before needing to revisit any area.
Some researchers use a simple system: left abdomen on odd days, right abdomen on even days, rotating within each half in a clockwise pattern. Others use a numbered grid drawn on an adhesive bandage attached to the injection area. Whatever system you choose, make it consistent. Inconsistent rotation leads to favorite spots, which leads to tissue damage.
Site rotation also matters for absorption consistency. Damaged tissue absorbs peptides at different rates than healthy tissue, which means a dose injected into a scar-tissue-rich area delivers a different effective dose than the same volume injected into fresh tissue. For protocols where precise, reproducible dosing matters, and that should be all protocols, site rotation is essential. Resources like the injection technique guide provide visual maps of recommended rotation patterns.
When to seek medical help
Most peptide injections are uneventful. But know the warning signs that require professional attention.
Increasing redness, warmth, and swelling at an injection site that worsens over 24 to 48 hours may indicate infection. A small red mark immediately after injection is normal. A growing, painful area is not.
Fever following injection suggests a systemic response that warrants medical evaluation.
Unusual systemic symptoms such as severe headache, rapid heart rate, difficulty breathing, or rash may indicate an allergic or adverse reaction. Seek immediate medical attention for these.
Hard lumps at injection sites that persist for more than a week should be evaluated to rule out issues beyond normal injection-site reactions.
The peptide therapy clinic guide and the local peptide therapy guide can help you find qualified providers who understand injectable peptide protocols. For those who prefer remote consultations, the online peptide therapy guide covers telemedicine options.
Regulatory considerations
The legal landscape around peptides varies by jurisdiction and continues to change. Some peptides are available only through prescription. Others are sold as research chemicals. A few have been restricted or reclassified in recent years. Before starting any peptide protocol, understand the legal status of peptides in your area. The peptide regulation news section tracks the latest changes.
Quality also falls under the regulatory umbrella. Research-grade versus pharmaceutical-grade peptides differ significantly in purity testing, manufacturing standards, and documentation. The peptide vendor guide and the testing lab guide help identify reliable sources with verified quality standards.
Advanced tips for peptide pen users
Once you master the basics, these refinements can further improve your experience and results.
Optimizing reconstitution for pen use
The reconstitution volume you choose affects everything downstream. More water means a lower concentration, which means a larger injection volume for the same dose. Less water means a higher concentration and a smaller injection volume. For pen use, there is a sweet spot.
Aim for concentrations that result in injection volumes between 0.05 and 0.30 mL for your most common dose. This range is comfortable to inject, easy to read on the pen dial, and large enough that the precision advantage of the pen matters. If your calculated volume falls below 0.03 mL, you are working with such a tiny amount that even mechanical precision reaches its limits. Dilute more. If your volume exceeds 0.5 mL, the injection gets uncomfortable. Concentrate more. The reconstitution calculator lets you experiment with different water volumes to find the ideal balance.
Managing multiple peptides
Researchers running peptide stacks often need to inject two or three peptides in the same session. With a pen system, you have options.
The simplest approach: one pen per peptide. Label each pen clearly. This is the most foolproof method, but it means owning multiple pen bodies. For stacks involving BPC-157 and TB-500, this is the standard approach since these peptides have different dosing frequencies and volumes.
The efficient approach: one pen body with multiple labeled cartridges. Swap cartridges between peptides. This works well when you inject all peptides at the same time, but it requires careful labeling and a few extra minutes for cartridge changes. Keep the multi-peptide administration guide handy for compatibility information.
Never combine different peptides in the same cartridge unless you have specifically verified their compatibility in solution. Some peptides can interact, degrade each other, or form aggregates when mixed. The peptide cycling guide covers which peptides can be safely combined and which should remain separate.
Tracking your protocol
A pen makes dosing consistent, but consistency only matters if you know what you are being consistent about. Track every injection: date, time, peptide, dose, injection site, and any observations. This log becomes invaluable when evaluating results, troubleshooting issues, or planning future protocols.
Many researchers find that results become noticeable after specific timelines. The peptide results timeline provides general benchmarks, but your personal log gives you data specific to your response. Peptide transformation tracking goes deeper into methods for documenting and evaluating your progress over time.
Understanding what pens cannot do
Pens are excellent tools with real limitations. They cannot deliver intramuscular injections. They are not suitable for nasal spray peptides or oral peptide capsules. They have upper volume limits that make them impractical for certain loading protocols. And they add a preparation step (cartridge loading) that syringes do not require.
Know these boundaries. Use pens where they excel and other delivery methods where they are better suited. The injectable versus oral peptides comparison covers the broader landscape of delivery options beyond pens and syringes.
Building your peptide pen kit
Having the right supplies before you start prevents mid-protocol scrambling. Here is what a complete pen setup requires.
The pen body: A reusable manual pen injector with adjustable dose dial. Look for one that accepts standard 3 mL cartridges and offers increments of at least 0.01 mL. Quality construction matters because the mechanical precision you are paying for only exists if the mechanism stays tight and accurate over hundreds of injections.
Pen needles: A supply of 31G x 5mm needles covers most situations. Buy extra. You go through one per injection, and running out mid-protocol means either reusing a needle (never do this) or skipping a dose. A box of 100 is a good starting quantity.
3 mL pen cartridges: Keep several on hand, especially if you run multiple peptides. Clear glass cartridges with rubber plunger stoppers are the standard. Label each one with the peptide name, concentration, reconstitution date, and expiration date.
Reconstitution supplies: Bacteriostatic water, syringes (1 mL and 3 mL) with 21G to 23G needles for drawing and transferring, and 27G vent needles for cartridge loading.
Alcohol prep pads: For cleaning vial stoppers, cartridge tops, and injection sites.
Sharps container: For used pen needles and syringe needles. Never throw sharps in regular trash.
Insulated travel case: A small cooler bag with an ice pack for transporting your pen during the day or while traveling.
The total investment for a quality pen setup is modest when compared to the cost of the peptides themselves. And the accuracy improvement alone pays for the equipment in saved peptide within the first few weeks of use. The peptide cost guide and therapy cost analysis help you understand the full financial picture.
Peptide pens for specific goals
Different research objectives have different practical requirements. Here is how pen use fits into the most common peptide goals.
Injury recovery and healing
Protocols for fast injury healing often involve daily or twice-daily injections of BPC-157 at 200 to 300 mcg, sometimes combined with TB-500 at 2 mg twice weekly. The daily injection frequency makes pen convenience essential. The small BPC-157 volumes demand pen precision. Together, these factors make the pen the obvious tool for healing protocols.
The best peptides for injury recovery guide covers the full range of options. For specific conditions, see the guides on tendon repair peptides, pain management peptides, and bone and cartilage repair peptides.
Body composition optimization
Whether the goal is fat loss, muscle growth, or both simultaneously through recomposition protocols, pens simplify the daily execution. Growth hormone secretagogues require consistent timing, typically before bed on an empty stomach, and the pen makes that nightly routine a 30-second process rather than a multi-minute syringe preparation.
The best peptides for muscle growth, best fat-burning peptides, and best weight loss stacks articles identify which peptides are most commonly used with pen delivery for these goals. For those interested in the safety profile of growth-promoting peptides, the safest muscle growth peptides guide provides a balanced assessment.
Anti-aging and longevity
Anti-aging peptide protocols tend to be long-term commitments measured in months or years. The convenience advantage of pens scales with protocol duration. Over a six-month protocol, the cumulative time saved by using a pen versus a syringe adds up to hours. More importantly, the consistency advantage compounds. Every injection at the right dose, delivered accurately, day after day.
Popular anti-aging peptides compatible with pen delivery include Epitalon, SS-31, MOTS-c, and GHK-Cu. The longevity peptides guide covers the research behind each one.
Athletic performance
Athletes and active individuals using peptides for performance support need reliable dosing that does not interfere with training schedules. A pen injection takes seconds and can happen anywhere, including a gym locker room, a hotel room before a morning run, or at home before bed. That portability and speed matter when you are trying to fit peptide protocols into an already packed schedule.
The best peptides for energy, strength protocol peptides, and testosterone-supporting peptides guides identify options that pair well with active lifestyles.
Gender-specific considerations
Both men and women use peptide pens effectively, but there are practical differences worth noting. The peptides for men guide and the peptides for women guide cover gender-specific dosing considerations. Women may need different needle lengths depending on typical injection site composition, and the safest peptides for women guide addresses safety considerations specific to female physiology. Women going through menopause may find peptide protocols particularly relevant for supporting changing hormone levels.
Frequently asked questions
Can I use a regular insulin pen for peptides?
Yes, many reusable insulin pens accept standard 3 mL cartridges and work perfectly for peptide delivery. The key consideration is ensuring the pen dose dial is calibrated in mL or in units that you can accurately convert to volume. Verify that the dose range covers your target injection volume and that the increment size provides adequate precision for your protocol. The peptide calculator helps translate between units and volume for any concentration.
How many doses can I get from one pen cartridge?
This depends on your cartridge volume (typically 1.5 or 3 mL), your reconstitution concentration, and your dose per injection. For example, a 3 mL cartridge loaded with BPC-157 at 2,500 mcg/mL and dosed at 250 mcg (0.1 mL per injection) provides approximately 28 to 29 doses after accounting for priming losses. The dosage calculation guide walks through the math for different scenarios.
Do peptide pens hurt more or less than syringes?
Most users report that pen injections hurt less. The needles are typically shorter and finer than standard syringe needles. The mechanical delivery eliminates the need to simultaneously stabilize the device and push a plunger. And the hidden needle reduces the psychological component of injection anxiety. Multiple clinical studies confirm that over 50 percent of patients report less pain with pens compared to traditional syringe delivery.
How do I know if my pen is delivering the correct dose?
Confirm during priming that fluid appears at the needle tip when you press the injection button. After injection, verify that the dose dial has returned to zero or the starting position. If the dial stops short of zero, the full dose was not delivered, and you should note the remaining amount. Modern pen injectors are validated to ISO 11608 accuracy standards, so mechanical accuracy is rarely the issue. User technique is far more likely to cause dose variations.
Can I combine two peptides in one pen cartridge?
This is generally not recommended unless you have verified compatibility. Some peptides interact when combined in solution, potentially degrading each other or forming inactive aggregates. The peptide stacking guide identifies known compatible and incompatible combinations. When in doubt, use separate cartridges for each peptide.
How often should I replace my reusable pen?
A quality reusable pen body should last six months to a year or more with proper care. Replace it when the dose dial mechanism feels loose, skips increments, or does not consistently return to zero after injection. The mechanical precision that makes the pen valuable depends on tight tolerances, and wear degrades those over time.
Is it safe to fly with a peptide pen?
Yes. Injection pens are standard medical devices recognized by airport security worldwide. Keep the pen and supplies in your carry-on bag. Bring pen needles in sealed, unused packaging. A sharps container is helpful for disposal during travel. If you carry reconstituted peptide, keep it in an insulated bag with a cold pack. International travel may benefit from a prescriber letter, though this is rarely required domestically.
What should I do if air bubbles appear in my cartridge?
Small air bubbles are common and not dangerous in subcutaneous injections. To minimize them, hold the pen needle-up and prime until you see a steady stream of fluid without air. If large bubbles form, gently tap the cartridge to move them toward the needle end, then prime to expel them. Persistent large bubbles may indicate a compromised cartridge seal. Inspect the rubber stopper and replace the cartridge if the seal appears damaged.
External resources
PMC: Factors affecting performance of insulin pen injector technology
PMC: Usability and safety of semaglutide pen-injectors
For researchers serious about getting the most from every peptide protocol, SeekPeptides provides the most comprehensive resource available, with evidence-based guides, dosing calculators, and a community of thousands who have navigated these exact questions. Whether you are choosing your first pen, dialing in a complex multi-peptide stack, or troubleshooting an issue that has you stuck, SeekPeptides members get access to detailed protocols and expert support that takes the guesswork out of peptide research.
In case I do not see you, good afternoon, good evening, and good night. May your doses stay precise, your needles stay sharp, and your protocols stay consistent.



