Jan 22, 2026
Something is wrong. You started ipamorelin a few days ago, expecting smooth sailing based on everything you read about its clean side effect profile. But now you have a headache. Some water retention.
Maybe tingling in your fingers. Is this normal? Is it dangerous? Should you stop?
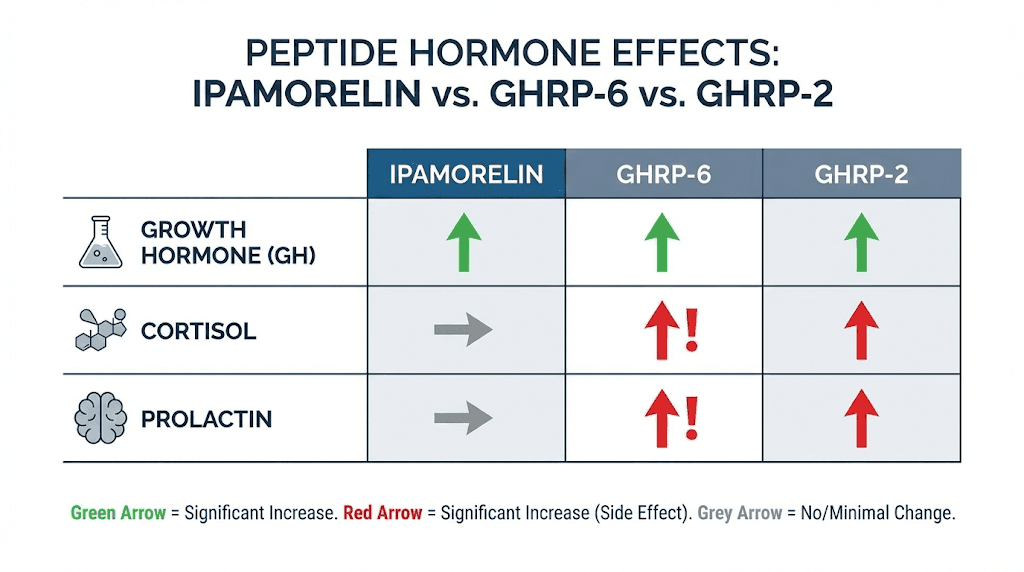
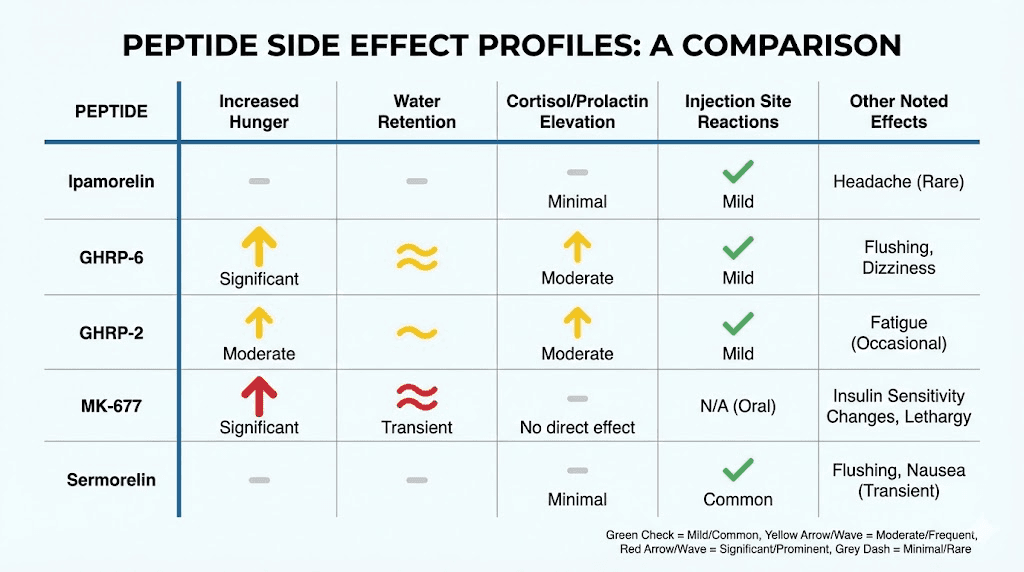
These questions matter. Ipamorelin is often described as one of the safest growth hormone releasing peptides, and that reputation is largely deserved. Unlike older peptides such as GHRP-6 or GHRP-2, ipamorelin does not significantly raise cortisol or prolactin levels. It does not trigger the extreme hunger that makes some growth hormone secretagogues difficult to tolerate. It stimulates growth hormone release through a selective mechanism that leaves other hormones relatively undisturbed.
But safe does not mean side effect free. Every compound that produces meaningful physiological effects will produce some reactions in some people. The key is understanding what to expect, knowing when something is concerning versus normal adaptation, and having clear strategies for managing whatever comes up.
This guide covers everything you need to know about ipamorelin side effects. The common ones. The rare ones. The mechanisms behind them. The practical management strategies that actually work. By the time you finish reading, you will know exactly what is happening in your body and what to do about it. SeekPeptides members have access to comprehensive protocols that incorporate these safety considerations from day one.
Understanding why ipamorelin causes side effects
Before diving into specific side effects, you need to understand the fundamental mechanism at play. Ipamorelin is a growth hormone releasing peptide that works by stimulating the pituitary gland to produce and release more growth hormone. This is not the same as injecting synthetic HGH directly. Your body is still producing its own growth hormone, just in larger amounts than it would naturally.
This distinction matters for side effects.
When you inject synthetic HGH, you are adding a fixed amount of hormone to whatever your body is already producing. The total level can spike unpredictably. With ipamorelin, you are working with your body's own regulatory systems. The pituitary still responds to feedback signals. It still releases growth hormone in pulses rather than constant elevated levels. This pulsatile release pattern is one reason ipamorelin tends to produce fewer side effects than direct HGH supplementation.
But increased growth hormone, regardless of how it gets there, creates downstream effects. Growth hormone influences water balance, tissue repair, glucose metabolism, and dozens of other physiological processes. When you increase GH levels, these processes shift. Some shifts are the benefits you want. Others manifest as side effects.
The selectivity advantage
Research published in the European Journal of Endocrinology demonstrated something remarkable about ipamorelin. Unlike GHRP-6 and GHRP-2, ipamorelin does not stimulate the release of ACTH or cortisol in levels significantly different from those observed following GHRH stimulation. This selectivity is what makes ipamorelin special among growth hormone secretagogues.
What does this mean practically? ACTH triggers cortisol release from the adrenal glands. Elevated cortisol causes a cascade of issues including increased fat storage, muscle breakdown, immune suppression, and sleep disruption. Peptides that raise cortisol alongside growth hormone force you to deal with these competing effects. Ipamorelin avoids this problem almost entirely.
The same selectivity applies to prolactin. Elevated prolactin can cause mood changes, libido issues, and even gynecomastia in men over time. Both GHRP-6 and GHRP-2 elevate prolactin. Ipamorelin does not. This makes the side effect profile fundamentally different and generally more manageable.
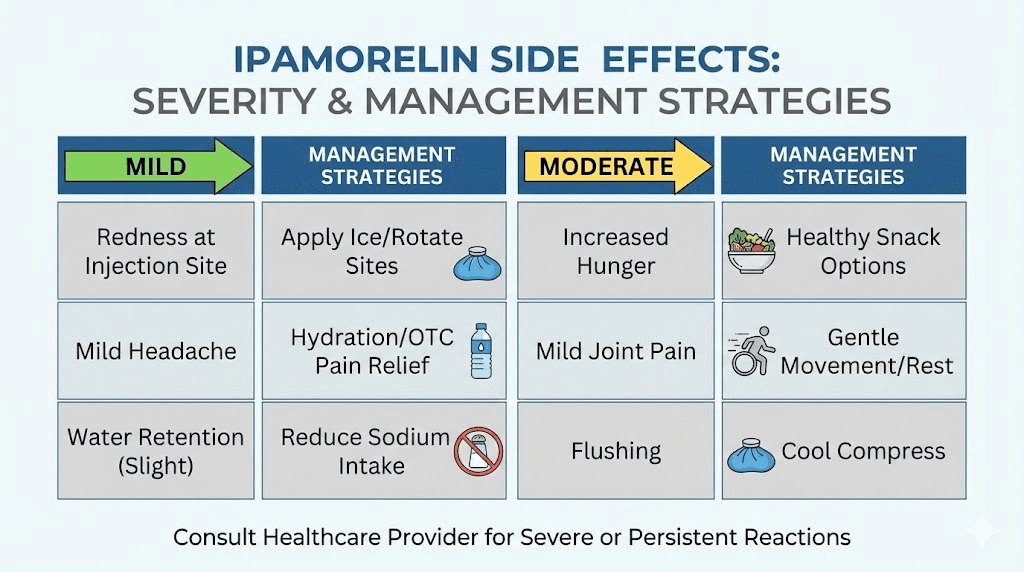
Common ipamorelin side effects
Let us start with what most people experience. These are the side effects that occur frequently, typically resolve on their own or with minor adjustments, and rarely require stopping the peptide entirely.
Headaches
Headaches are the most commonly reported side effect, particularly during the first one to two weeks of use. The mechanism is straightforward. Growth hormone influences intracranial pressure, and when GH levels rise, some people experience this as a headache. The sensation is typically mild to moderate, described as a dull pressure rather than a sharp pain.
Several factors determine whether you will experience this. Your baseline GH levels matter. If you have been running on low growth hormone for years, the sudden increase creates a more dramatic shift. Your starting dose matters. Higher initial doses create more pronounced GH pulses.
Hydration status matters too. Dehydration amplifies headache symptoms from almost any cause.
The good news is that headaches almost always resolve. Your body adapts to the new hormone environment within one to three weeks. The vasculature adjusts. The pressure normalizes. For most people, headaches become a non-issue after the initial adaptation period.
Management strategies for headaches
Start with a lower dose than you might otherwise consider optimal. If the standard range is 200 to 300 mcg, begin at 100 to 150 mcg for the first week. Let your body adapt before increasing. Use the peptide calculator to determine precise amounts based on your weight and goals.
Hydration is critical. Drink at least half your body weight in ounces of water daily when using growth hormone peptides. Many researchers find that headaches decrease dramatically simply by increasing water intake. This is not complicated advice, but it works.
If headaches persist beyond two weeks at conservative doses with proper hydration, consider splitting your dose. Instead of one injection, divide the amount between morning and evening.
This creates smaller individual GH pulses that may be more tolerable.
Water retention
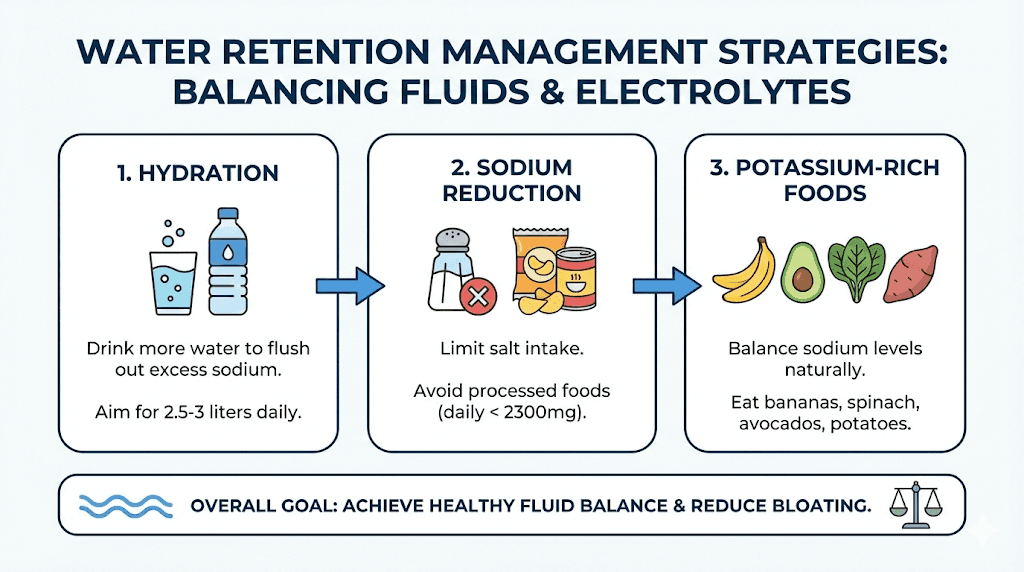
Growth hormone has a well-documented effect on fluid balance. It promotes sodium retention in the kidneys, which pulls water along with it. The result is mild water retention that shows up as puffiness in the hands, feet, or face. Some people notice their rings feel tighter. Others see slight swelling in the ankles after standing.
This is not the same as the dangerous edema associated with serious medical conditions. The water retention from ipamorelin is typically mild, often unnoticeable, and represents a shift in fluid distribution rather than true fluid overload. Your body is holding slightly more water in the extracellular spaces.
Water retention tends to be dose dependent. Higher doses produce more noticeable retention. It also tends to stabilize over time. The first few weeks often show the most pronounced effects as your body adjusts to consistently elevated GH levels.
Managing water retention
Diet plays a significant role. High sodium intake worsens water retention considerably. If you are experiencing noticeable puffiness, examine your food choices. Processed foods, restaurant meals, and many prepared foods contain far more sodium than home-cooked alternatives. Reducing sodium intake often reduces water retention proportionally.
Potassium helps counterbalance sodium. Foods rich in potassium include bananas, potatoes, spinach, and avocados. You do not need supplements in most cases. Simply emphasizing potassium-rich foods while reducing sodium often makes a noticeable difference within days.
Light activity helps move fluid through the lymphatic system. Walking, swimming, or other low-impact movement reduces pooling in the extremities. If you spend long hours sitting, periodic movement breaks become especially important when using growth hormone peptides.
Dose reduction remains the most reliable solution if water retention becomes genuinely bothersome. Lower your dose by 25 to 40 percent and reassess after two weeks. Often you can find a dose that provides benefits without significant water retention.
Injection site reactions
Subcutaneous injections inevitably cause some local tissue response. With ipamorelin, this commonly includes mild redness, slight swelling, occasional itching, or a small lump at the injection site. These reactions are usually minor and resolve within hours to days.
The mechanism involves both the physical trauma of the injection and the body's response to the peptide solution itself. Some people experience localized histamine release that causes itching and redness. This is not a true allergic reaction in most cases but rather direct mast cell activation. The distinction matters because true allergies require stopping the peptide while localized histamine responses can be managed.
Some researchers notice small nodules under the skin at injection sites. These are typically deposits of the peptide solution that absorb slowly. They are not dangerous and usually disappear within a few days to a week.
Minimizing injection site reactions
Proper injection technique matters enormously. Use appropriate needle length for subcutaneous injection, typically 27 to 31 gauge and half inch in length. Inject at a 45 to 90 degree angle depending on your subcutaneous fat layer. Allow the alcohol from the prep swab to dry completely before injecting as wet alcohol irritates tissue.
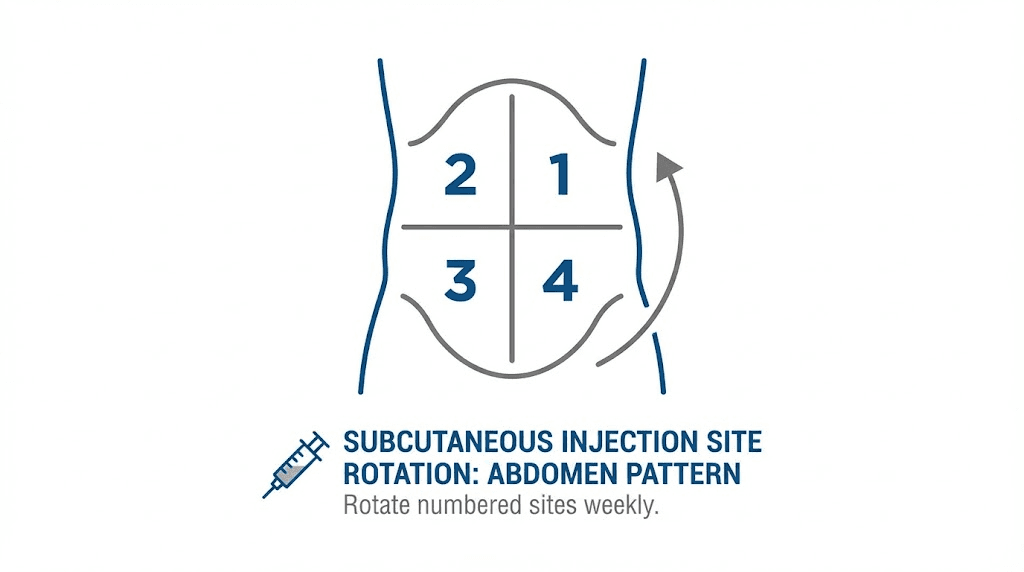
Rotate injection sites systematically. The abdomen offers the most surface area and consistent absorption. Create a mental map dividing your abdominal area into zones and rotate through them. Never inject into the same spot twice in a row. Rotation prevents cumulative tissue irritation and allows each site to fully recover before the next injection.
If you experience consistent histamine reactions with redness and itching, consider taking a natural antihistamine like quercetin before your injection. Some researchers find that diluting the peptide with more bacteriostatic water reduces irritation. Instead of reconstituting with 1 mL, try 2 mL for the same total peptide amount.
For nodules that form at injection sites, warm compresses help disperse the fluid and accelerate absorption. Apply a warm, not hot, compress for 10 to 15 minutes once or twice daily until the nodule resolves.
Increased appetite
Some people experience increased hunger when using ipamorelin. This is notably less pronounced than with GHRP-6, which is famous for causing extreme, almost uncontrollable hunger. But ipamorelin can still affect appetite in some individuals, particularly at higher doses.
The mechanism relates to ghrelin receptor activation. Ipamorelin is a ghrelin mimetic, meaning it activates the same receptors that the hunger hormone ghrelin targets. However, ipamorelin is selective in its binding. It preferentially activates the growth hormone releasing aspects of these receptors while having less effect on the appetite stimulating pathways. This selectivity is why hunger is less of an issue compared to older GHRPs, but the effect is not completely absent for everyone.
Some researchers actually view mild appetite increase as beneficial. If you are trying to build muscle, eating more supports that goal. The issue arises when you are using ipamorelin for fat loss and increased hunger works against your caloric targets.
Managing appetite changes
Timing your injection strategically can help. Many researchers inject before bed specifically because they sleep through any appetite increase.
By morning, the effect has passed. This timing also aligns with the body's natural growth hormone release patterns during sleep, potentially optimizing effectiveness.
If you need to inject during waking hours and find appetite increase problematic, have a small protein-rich snack prepared. Protein provides satiety with minimal caloric impact compared to carbohydrates or fats. Greek yogurt, cottage cheese, or a small portion of meat can satisfy the increased hunger without derailing your nutrition plan.
Fiber-rich foods also help. Vegetables, especially leafy greens, provide volume and fiber that promote fullness. Keeping cut vegetables readily available gives you a low-calorie option when appetite spikes hit.
Nausea and dizziness
Some researchers experience transient nausea or dizziness, particularly immediately after injection. This effect is usually mild and brief, lasting minutes rather than hours. It occurs more commonly with higher doses or when injecting on an empty stomach.
The mechanism involves the sudden spike in growth hormone affecting various systems simultaneously. Some people are simply more sensitive to these hormonal shifts than others. There is often a genetic component. If you have historically been sensitive to hormonal fluctuations, you may be more likely to experience these effects.
Reducing nausea and dizziness
Avoid injecting on a completely empty stomach. Having a small amount of food in your system, even just a few crackers or a piece of fruit, can reduce nausea considerably. You do not need a full meal, just something to stabilize your system.
Inject slowly. Pushing the plunger too quickly can cause the solution to pool rather than disperse, potentially intensifying local and systemic reactions. A slow, steady injection over 5 to 10 seconds is preferable.
If dizziness occurs, sit or lie down until it passes. Do not attempt to stand or move quickly. The sensation almost always resolves within minutes. If it persists longer or becomes severe, this warrants dose reduction and possibly consultation with a healthcare provider.
Less common ipamorelin side effects
Beyond the frequently reported effects, some researchers experience less common reactions. These are not rare in an absolute sense but occur in a smaller percentage of users.
Joint pain and stiffness
Growth hormone promotes tissue repair and growth. This includes connective tissues in the joints. As these tissues grow and repair, some people experience temporary joint discomfort. This is actually a sign that the peptide is working, though it is understandably uncomfortable.
The discomfort typically manifests as stiffness upon waking or after periods of inactivity. It may feel similar to the early stages of arthritis. Some researchers describe it as their joints feeling tight or creaky. The sensation is usually symmetric, affecting both knees or both wrists rather than just one side.
This effect is more common in people who already have some joint issues or those using higher doses. It tends to resolve as the body adapts, usually within the first few weeks to a month.
Managing joint discomfort
Light movement helps. Gentle stretching and low-impact activity keeps the joints mobile and reduces stiffness. Avoid heavy loading on affected joints until the discomfort resolves. Swimming is particularly beneficial as it provides movement without joint stress.
Omega-3 fatty acids from fish oil provide natural anti-inflammatory support. If you are not already supplementing with fish oil, starting during peptide use can help mitigate joint discomfort. Look for products providing at least 2 grams of combined EPA and DHA daily.
Hydration matters here too. Synovial fluid, the lubricant in your joints, is largely water. Dehydration makes joints feel worse. The standard recommendation of half your body weight in ounces of water applies.
If joint pain is significant, reduce your dose by 25 to 40 percent and reassess. You can always increase again once your body has adapted. Pushing through significant joint pain is counterproductive.
Numbness and tingling
Some researchers experience numbness or tingling, particularly in the hands and fingers. This can manifest as pins and needles sensations, especially upon waking. In some cases, it resembles the symptoms of carpal tunnel syndrome.
The mechanism involves water retention affecting nerve pathways. The median nerve runs through the carpal tunnel in the wrist, a narrow space surrounded by bones and ligaments. When fluid retention increases, the space becomes tighter, potentially compressing the nerve. This compression causes the classic carpal tunnel symptoms of numbness, tingling, and sometimes weakness in the thumb and first three fingers.
This is more likely to occur at higher doses or in people who already have some degree of carpal tunnel narrowing. It is typically reversible with dose reduction but should not be ignored.
Addressing numbness and tingling
Dose reduction is the first line response. If you are experiencing numbness or tingling, lower your dose by 30 to 50 percent immediately. Continue at the reduced dose for two to four weeks and assess. For most people, symptoms resolve completely at lower doses.
Wrist splints worn at night can help. They keep the wrist in a neutral position that minimizes carpal tunnel compression. These are inexpensive and available at most pharmacies. Wearing them during sleep, when symptoms often peak, provides relief for many people.
If symptoms persist despite dose reduction, stopping ipamorelin temporarily may be necessary. The good news is that growth hormone related carpal tunnel symptoms are almost always reversible once the cause is removed. True permanent carpal tunnel syndrome from peptide use is extremely rare.
Do not ignore persistent or severe numbness. Chronic nerve compression can cause lasting damage. If reducing dose does not resolve symptoms within a few weeks, consult a healthcare provider.
Fatigue and lethargy
This side effect seems paradoxical. Ipamorelin is supposed to increase energy, not decrease it. Yet some researchers, particularly in the first week or two, experience tiredness and lethargy. Understanding why requires looking at the adaptation process.
When you significantly alter your hormonal environment, the body needs time to recalibrate. Growth hormone affects metabolism, sleep architecture, and energy production systems. During the adaptation phase, these systems are adjusting. Some people experience this adjustment period as fatigue.
Additionally, ipamorelin can affect sleep, particularly if injected close to bedtime. Some researchers find they sleep more deeply but feel groggy upon waking. Others have unusually vivid dreams that disturb their sleep quality. These sleep changes can manifest as daytime fatigue.
Managing fatigue
Give it time. Most adaptation-related fatigue resolves within one to two weeks. If you are in the first week of use, expect some adjustment period and plan accordingly. Do not schedule demanding tasks or make important decisions if you are feeling unusually tired.
Optimize injection timing. If bedtime injection is causing morning grogginess, try injecting earlier in the evening. Some researchers find that injecting 2 to 3 hours before sleep rather than immediately before improves their sleep quality and morning energy.
Ensure adequate sleep duration. Growth hormone release peaks during deep sleep. If you are cutting sleep short, you are working against the peptide's effects and likely worsening fatigue. Aim for 7 to 9 hours during the adaptation period.
If fatigue persists beyond two weeks, evaluate your dose and timing. Chronic fatigue suggests something in your protocol needs adjustment. SeekPeptides members can access detailed troubleshooting guides for optimizing their protocols.
Rare but serious ipamorelin side effects
While ipamorelin has an excellent safety profile compared to many alternatives, rare but potentially serious side effects can occur. Understanding these helps you recognize warning signs early.
Insulin sensitivity changes
Growth hormone has complex effects on glucose metabolism. It can promote insulin resistance, meaning your cells become less responsive to insulin and blood sugar levels may rise. Research published in Neuro Endocrinology Letters showed that ipamorelin stimulates insulin release from the pancreas, which is actually beneficial for glucose control. However, the effects on insulin sensitivity over long-term use are less well understood.
This becomes more relevant with extended use, typically after several months. Short-term use of a few weeks rarely causes significant insulin sensitivity changes. But if you are using ipamorelin continuously for many months, monitoring becomes important.
People with prediabetes, diabetes, or family history of diabetes should be particularly vigilant. The effects on glucose metabolism can compound existing issues.
Monitoring and management
Get baseline bloodwork before starting ipamorelin. At minimum, this should include fasting glucose and ideally HbA1c. These provide reference points for comparison.
Repeat testing every three to four months during use. If fasting glucose trends upward or HbA1c increases, this signals developing insulin resistance. Catching this early allows for intervention before problems become significant.
Lifestyle factors amplify or mitigate these effects. Regular exercise improves insulin sensitivity independent of other factors. A diet lower in refined carbohydrates reduces glucose spikes. Maintaining healthy body composition helps as well. If you are using ipamorelin as part of a comprehensive fat loss protocol that includes exercise and diet modification, you are already doing the things that protect insulin sensitivity.
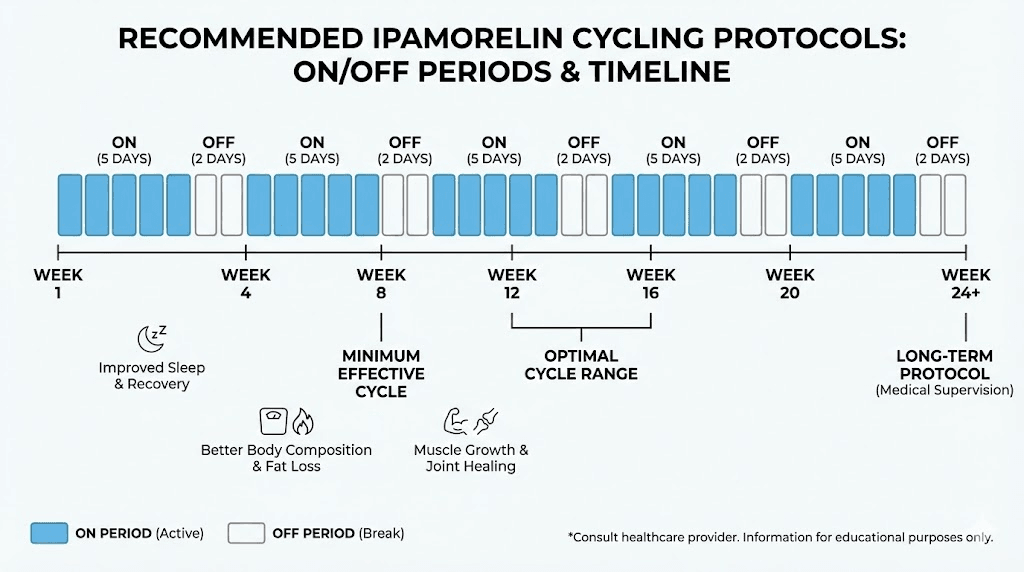
If significant insulin sensitivity changes occur despite healthy lifestyle, dose reduction or cycling becomes necessary. Taking periodic breaks from ipamorelin, such as four weeks off after eight to twelve weeks on, may help prevent this adaptation.
Hormone desensitization
Any compound that artificially stimulates hormone release carries theoretical risk of desensitization over time. The pituitary gland could become less responsive to the ipamorelin signal, requiring higher doses for the same effect. Or the target tissues could become less responsive to growth hormone itself.
The research on this is limited. Most studies of ipamorelin have been short-term. Long-term data in humans is sparse. Anecdotally, some users report needing to increase doses over time to maintain effects, which could indicate some degree of desensitization.
Unlike synthetic HGH, ipamorelin does not suppress your natural growth hormone production. Your pituitary continues functioning normally. This is an important distinction that suggests ipamorelin poses less desensitization risk than direct hormone supplementation. But the concern is not entirely eliminated.
Preventing desensitization
Cycling is the primary prevention strategy. Rather than using ipamorelin continuously indefinitely, plan for periodic breaks. Common protocols include eight weeks on, four weeks off, or twelve weeks on, four weeks off. During off periods, your system has time to resensitize.
Use the minimum effective dose. More is not always better. If 200 mcg produces the results you want, there is no benefit to using 300 mcg. Higher doses may actually accelerate any desensitization that occurs.
Combine with other strategies that support natural GH release. Quality sleep, regular exercise, and intermittent fasting all naturally boost growth hormone. Using these alongside ipamorelin rather than relying solely on the peptide may allow for lower doses and reduce desensitization risk.
Allergic reactions
True allergic reactions to ipamorelin are rare but possible. These differ from the localized histamine responses discussed earlier. An allergic reaction is a systemic immune response that can range from mild hives to severe anaphylaxis.
Signs of allergic reaction include widespread hives or rash, swelling of the face, lips, or throat, difficulty breathing, rapid heartbeat, and dizziness or loss of consciousness. These symptoms require immediate medical attention. If you experience throat swelling or difficulty breathing after ipamorelin injection, call emergency services immediately.
Allergic reactions almost always occur early in use, typically with the first few injections. If you have used ipamorelin many times without issue, a sudden allergic reaction is extremely unlikely. The immune system either reacts or it does not, and this is usually apparent quickly.
Managing allergy risk
If you have a history of allergies to other peptides or injectable medications, proceed with extra caution. Consider having a first injection under medical supervision where treatment is immediately available if needed.
Have appropriate emergency medications available, particularly if you have known allergies. An epinephrine auto-injector is appropriate for anyone with a history of severe allergic reactions, regardless of the trigger.
If you experience any symptoms suggesting an allergic reaction, stop ipamorelin immediately and seek medical evaluation. Do not attempt to continue use or reduce the dose. Allergic reactions can escalate unpredictably, and the only safe approach is complete avoidance once a reaction occurs.
Ipamorelin side effects versus other growth hormone peptides
Context matters when evaluating side effects. Ipamorelin's profile looks even better when compared to alternatives. Understanding these comparisons helps you appreciate why ipamorelin is often the first choice for growth hormone optimization.
Ipamorelin versus GHRP-6
GHRP-6 is an older growth hormone secretagogue with a very different side effect profile. The most notorious difference is hunger. GHRP-6 causes intense, sometimes overwhelming hunger that makes it difficult to maintain any caloric restriction. Users describe hunger that feels almost painful, not just increased appetite but genuine distress if food is not available.
GHRP-6 also raises cortisol and prolactin levels significantly. This means you are dealing with stress hormone elevation alongside growth hormone elevation. The benefits become partially offset by the detriments. Fat may be harder to lose when cortisol is elevated. Sleep may be disrupted. Mood may be affected.
Ipamorelin provides similar growth hormone release without these issues. Research directly comparing the two peptides confirms that ipamorelin does not elevate cortisol or prolactin above baseline levels that occur with natural GHRH stimulation. The hunger effect is dramatically reduced or absent.
Ipamorelin versus GHRP-2
GHRP-2 was developed as an improvement over GHRP-6, and it is in some ways. The hunger effect is reduced compared to GHRP-6, though still present. GHRP-2 is more potent for growth hormone release, producing larger GH pulses at equivalent doses.
But GHRP-2 still raises cortisol and prolactin, though to a lesser degree than GHRP-6. It still has effects on blood sugar and has been associated with more concerning adverse events in some clinical contexts. The improved potency comes with a side effect profile that remains significantly more problematic than ipamorelin.
Ipamorelin sacrifices some of the raw GH-boosting power for a much cleaner experience. For most applications, this tradeoff is worthwhile. The difference in GH release is not dramatic, but the difference in side effects is substantial.
Ipamorelin versus MK-677
MK-677, also known as ibutamoren, is often compared to ipamorelin though it is not technically a peptide. It is an oral growth hormone secretagogue, which makes it convenient, but this comes with different considerations.
MK-677 has a much longer half-life, remaining active in the body for about 24 hours. This produces sustained GH elevation rather than the pulsatile release that ipamorelin creates. Some argue this sustained elevation is less physiological and may carry more risk over time.
Side effects of MK-677 include pronounced appetite increase, more significant water retention than ipamorelin, and notable effects on blood sugar and insulin sensitivity. MK-677 is more likely to cause lethargy, particularly in the first weeks of use. The convenience of oral dosing comes with a generally heavier side effect burden.
Ipamorelin requires injection, which is a barrier for some people. But the trade-off is a cleaner side effect profile and release patterns that more closely match natural physiology.
Ipamorelin versus sermorelin
Sermorelin is a growth hormone releasing hormone analog rather than a ghrelin mimetic like ipamorelin. It works through a different receptor system to achieve similar ends. The side effect profile is comparably clean to ipamorelin, with low rates of concerning reactions.
The main difference is potency. Sermorelin tends to produce smaller GH releases than ipamorelin. Some researchers find it insufficient for their goals. Others appreciate the gentler approach, particularly as an introduction to growth hormone optimization.
Combining ipamorelin with CJC-1295, which is functionally similar to sermorelin, is a common strategy. This combination leverages the strengths of both pathways while keeping side effects manageable. The ipamorelin versus CJC-1295 comparison page provides detailed analysis of these options.
Side effects by dosage level
Dose and side effects have a clear relationship with ipamorelin. Understanding this helps you find the sweet spot that delivers benefits with minimal issues.
Low dose range: 100 to 150 mcg
At this dose range, most people experience minimal to no side effects. This makes it an excellent starting point, particularly for those new to peptide injections or those concerned about sensitivity.
Growth hormone release at these doses is modest but measurable. Benefits include improved sleep quality, mild recovery enhancement, and subtle improvements in skin and hair quality over time. These effects build gradually and may take several weeks to become noticeable.
The tradeoff is that more dramatic effects on body composition and performance require higher doses for most people. Low doses are sustainable long-term with very little risk but may not produce the results aggressive users seek.
Standard dose range: 200 to 300 mcg
This is the most common dose range and where most research has been conducted. Growth hormone release is significant and consistent. Most people experience meaningful benefits in recovery, body composition, and overall well-being.
Side effects in this range are more common but usually mild. Headaches during the first week or two are typical. Mild water retention occurs in a significant percentage of users. Occasional increased appetite, though less pronounced than with other GHRPs, may occur.
For most goals, this range represents the best balance of effectiveness and tolerability. The peptide dosing calculator can help determine your specific optimal dose based on body weight and objectives.
Higher dose range: 300 to 500 mcg
Some researchers push into higher dose ranges, often 300 to 500 mcg or occasionally higher. Growth hormone release increases, but not proportionally. The GH response curve begins to flatten at higher doses, meaning you get diminishing returns for each additional microgram.
Meanwhile, side effects increase more linearly with dose. Water retention becomes more pronounced. Headaches are more likely and more severe. Joint discomfort and numbness become real concerns at these doses. The risk of insulin sensitivity changes increases with prolonged high-dose use.
For most applications, these doses exceed what is necessary. The additional growth hormone release rarely justifies the additional side effect burden.
Exceptions might exist for competitive athletes with specific goals and medical supervision, but general users should view doses above 300 mcg with caution.
Managing side effects: practical protocols
Having covered individual side effects, let us consolidate the management strategies into practical protocols you can implement.
The adaptation protocol
Start low and increase gradually. This is the single most effective strategy for minimizing side effects while still achieving your goals.
Week one: Begin at 100 mcg once daily, preferably before bed. Monitor for any reactions. Note headaches, water retention, or other symptoms. Most people tolerate this dose without significant issues.
Week two: If week one was uneventful, increase to 150 mcg. Continue monitoring. Some people begin to notice mild headaches or water retention at this level. If symptoms are bothersome, remain at this dose for another week before increasing.
Week three: Increase to 200 mcg if tolerating well. This is within the standard effective range for most goals. Many researchers remain at this dose indefinitely. Others continue increasing.
Week four and beyond: Continue increasing by 50 mcg per week until reaching your target dose or until side effects become bothersome. The goal is to find your personal optimal dose, the highest amount you can tolerate without significant issues while achieving your desired results.
The hydration protocol
Proper hydration prevents or reduces many ipamorelin side effects. This protocol ensures adequate intake.
Calculate your baseline: Take your body weight in pounds and divide by two. This gives the minimum ounces of water you should consume daily. A 180-pound person needs at least 90 ounces, about 2.6 liters.
Add more for activity: For every hour of exercise, add 16 to 24 ounces. Sweating increases fluid needs significantly.
Distribute throughout the day: Do not try to drink your entire allocation in one sitting. Spread intake evenly, focusing on consuming more in the morning and less in the hours before bed to avoid sleep disruption.
Monitor your urine: Pale yellow indicates adequate hydration. Dark yellow suggests you need more water. Clear and frequent urination suggests you might be overdoing it.
The injection site rotation protocol
Systematic rotation prevents injection site reactions and ensures consistent absorption.
Map your abdomen into quadrants. Upper left, upper right, lower left, lower right. Each quadrant has multiple potential injection sites.
Inject in one quadrant per day, moving to the next quadrant the following day. Within each quadrant, vary the specific spot. Never inject into the exact same location twice in a row.
If one site becomes irritated, skip it entirely until it heals. Mark problem areas mentally and avoid them for at least a week after any reaction.
Consider alternating between abdomen and other sites like the outer thigh if abdominal issues persist. Thigh injections are slightly more variable in absorption but provide an alternative when needed.
The timing optimization protocol
When you inject affects both effectiveness and side effects. Optimizing timing helps on both fronts.
Bedtime injection is most common and often best. Growth hormone naturally peaks during sleep. Injecting before bed amplifies this natural rhythm. It also means you sleep through any immediate post-injection effects like headache or nausea.
Split dosing suits some researchers better. If side effects are bothersome with a single dose, try dividing into morning and evening doses. Each individual dose is smaller, potentially reducing per-dose side effects.
Fasted injection may enhance GH release but can increase nausea risk. If you inject fasted and experience nausea, try having a small snack first. The slight reduction in GH release is usually not significant enough to matter, and avoiding nausea is worthwhile.
Post-workout injection capitalizes on the natural GH elevation that occurs after exercise. Some researchers time their evening injection for immediately after training. This may enhance recovery benefits but requires consistent workout timing.
When to stop or seek medical attention
Most ipamorelin side effects are mild and manageable. But knowing when to stop or seek help is essential for safe use.
Stop immediately if:
You experience signs of severe allergic reaction including throat swelling, difficulty breathing, widespread hives, or dizziness and confusion. These require immediate medical attention. Call emergency services if symptoms are severe.
You develop significant, persistent joint pain that limits function. While mild joint discomfort is common and resolves, pain that prevents normal activities suggests something more concerning.
Numbness or tingling becomes constant rather than intermittent. Occasional tingling upon waking is usually manageable with dose reduction. Constant numbness that persists throughout the day suggests nerve compression that needs attention.
Reduce dose and monitor closely if:
Headaches persist beyond two weeks at starting doses. Adaptation should occur within this timeframe. Continued headaches suggest your current dose exceeds what your body can comfortably handle.
Water retention is significant enough to be visible or uncomfortable. Some retention is expected, but dramatic puffiness or rapid weight gain from fluid warrants dose reduction.
You experience persistent fatigue rather than improved energy. If you are consistently more tired than before starting ipamorelin after the first two weeks, your protocol needs adjustment.
Consult a healthcare provider if:
Symptoms persist despite dose reduction. If lowering your dose does not resolve issues, professional evaluation helps rule out other causes and determine if continuing is appropriate.
You have pre-existing conditions that could be affected. Diabetes, cardiovascular disease, or history of cancer warrant medical supervision when using growth hormone influencing compounds.
You notice changes in blood sugar regulation.
Increased thirst, frequent urination, or other signs of glucose dysregulation should prompt testing and evaluation.
Long-term considerations
Short-term side effects are well characterized. Long-term effects of ipamorelin use are less definitively known due to limited research extending beyond a few months.
What we know
Ipamorelin does not suppress natural growth hormone production. Unlike synthetic HGH, which can cause pituitary shutdown with prolonged use, ipamorelin works with your natural systems. Your pituitary continues functioning normally. When you stop ipamorelin, your natural GH production should continue at its previous baseline.
Short to medium term use appears safe based on available evidence. Studies lasting several weeks to a few months have not identified concerning safety signals beyond the side effects already discussed.
The selectivity that makes ipamorelin special, not raising cortisol, prolactin, or other hormones, should persist with continued use. There is no indication that long-term use changes this fundamental characteristic.
What we do not know
Multi-year continuous use has not been studied in humans. Most research involves weeks to months of administration. The effects of using ipamorelin continuously for years remain theoretical.
Cancer risk is a theoretical concern with any growth hormone influencing compound. Growth hormone promotes cell division, which could theoretically accelerate tumor growth if a cancer exists. Research specifically examining ipamorelin and cancer risk is lacking. Most oncologists advise against GH-enhancing compounds for anyone with active cancer or high cancer risk.
Cumulative effects on glucose metabolism over many years are unknown.
While short-term insulin sensitivity changes are usually minor, the picture with decades of use is unclear.
Prudent long-term use strategies
Cycle rather than use continuously. Taking breaks, typically four weeks off after two to three months on, allows your system to normalize and potentially reduces any cumulative effects.
Monitor bloodwork regularly. At minimum, check fasting glucose, HbA1c, and IGF-1 levels every three to four months during use. This catches any developing issues early.
Use the minimum effective dose. More is not better, especially for long-term use. The lowest dose that achieves your goals is the safest approach.
Maintain healthy lifestyle fundamentals. Good nutrition, regular exercise, adequate sleep, and stress management support your body's ability to handle the hormonal shifts ipamorelin creates. These foundations become even more important with long-term use.
For researchers serious about optimizing their peptide protocols safely, SeekPeptides offers the most comprehensive resource available. Members access evidence-based guides, proven protocols, and a community of thousands who have navigated these exact questions.
Frequently asked questions
How long do ipamorelin side effects typically last?
Most common side effects like headaches and initial water retention resolve within one to three weeks as your body adapts to elevated growth hormone levels. Injection site reactions usually clear within 24 to 48 hours. Side effects that persist beyond the adaptation period often respond to dose reduction.
Can I take ipamorelin if I have diabetes?
Ipamorelin affects glucose metabolism and insulin sensitivity. If you have diabetes or prediabetes, use requires careful monitoring and ideally medical supervision. Research shows ipamorelin stimulates insulin release from the pancreas, which could actually be beneficial, but effects on long-term glucose control need monitoring through regular bloodwork.
Is it normal to feel tired when starting ipamorelin?
Yes, transient fatigue during the first one to two weeks is common as your body adjusts to the new hormonal environment. This typically resolves spontaneously. If fatigue persists beyond two weeks, consider adjusting your injection timing or reducing your dose.
Why do I get headaches from ipamorelin?
Headaches result from growth hormone's effects on intracranial pressure and fluid dynamics. They are most common in the first two weeks and usually resolve with adaptation. Staying well hydrated, starting with lower doses, and using the peptide calculator to ensure appropriate dosing all help reduce headache frequency and severity.
Can ipamorelin cause carpal tunnel syndrome?
Ipamorelin can cause symptoms resembling carpal tunnel, including numbness and tingling in the hands, due to water retention in the wrist area. This is usually dose-dependent and reversible. Reducing dose typically resolves symptoms. Wearing wrist splints at night can provide relief while adjusting your protocol.
How do ipamorelin side effects compare to HGH side effects?
Ipamorelin generally has a milder side effect profile than synthetic HGH. It does not suppress natural GH production, produces more physiological pulsatile release, and does not carry the same risk of joint and cardiovascular effects seen with HGH. However, both can cause water retention, carpal tunnel symptoms, and effects on glucose metabolism at higher doses.
Should I stop ipamorelin if I experience water retention?
Mild water retention does not require stopping. First try reducing sodium intake, increasing potassium-rich foods, and ensuring adequate hydration. If retention is significant, reduce your dose by 25 to 40 percent. Only stop if retention is severe, causes discomfort, or does not respond to these interventions.
External resources
PubMed: Ipamorelin, the first selective growth hormone secretagogue
PMC: Growth hormone secretagogues in body composition management
In case I do not see you, good afternoon, good evening, and good night. Join us.



