Jan 31, 2026
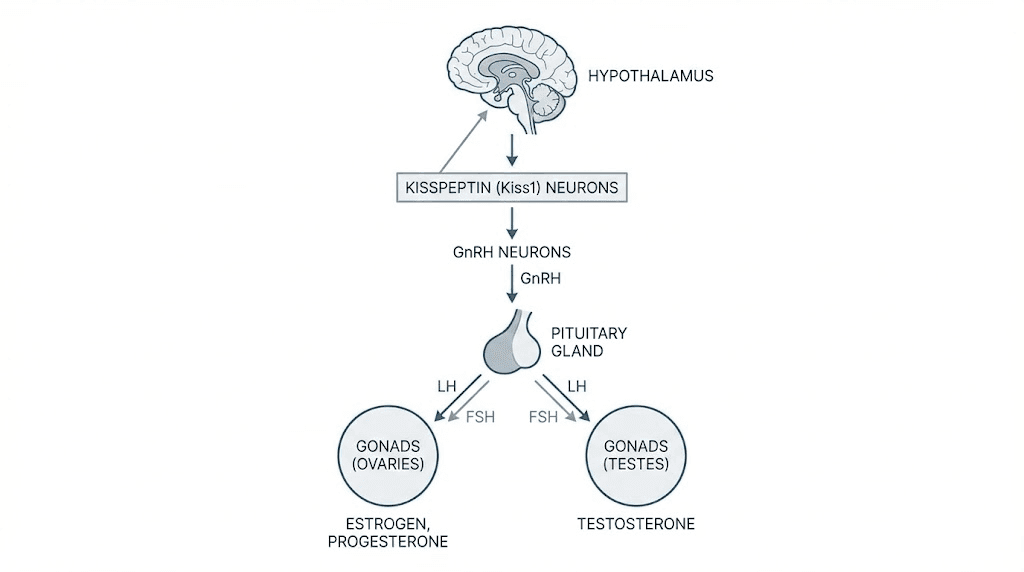
Most people who research peptides have never heard of kisspeptin. That is a problem. Because while compounds like BPC-157 and TB-500 get the headlines, kisspeptin sits at the very top of the reproductive hormone cascade, controlling everything downstream. It tells your brain to release GnRH. GnRH tells your pituitary to release LH and FSH. And those hormones tell your gonads to produce testosterone, estrogen, and mature eggs. Without kisspeptin, the entire system goes dark.
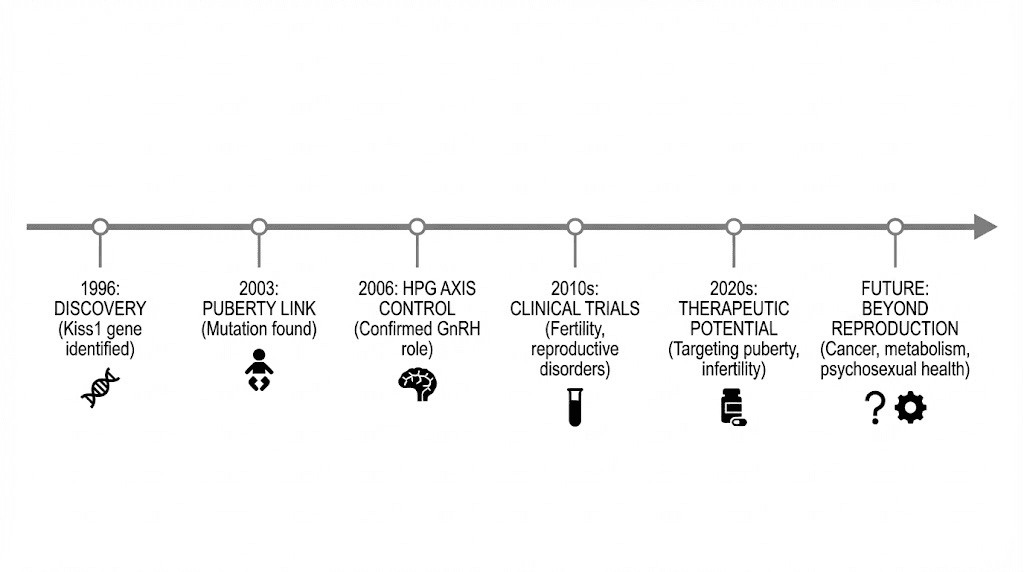
The science behind this peptide is not speculative. Researchers at Imperial College London have safely administered kisspeptin to more than 500 men and women across multiple clinical trials. The results cover fertility, sexual desire, testosterone production, IVF outcomes, and even emotional processing. Yet outside of academic endocrinology, almost nobody talks about it.
This guide covers everything researchers need to know about kisspeptin peptide benefits. You will learn exactly how it works at the molecular level, what the clinical data actually shows, how it compares to hCG and GnRH analogs, what dosing protocols look like, and where the research is heading. Whether your interest is muscle growth, libido, fertility, or longevity, understanding kisspeptin means understanding the master switch your entire endocrine system depends on. SeekPeptides members already know this is one of the most underappreciated peptides in the field. Here is why.
What is kisspeptin and why does it matter
Kisspeptin is not one peptide. It is a family of peptides, all derived from the KISS1 gene, which encodes a 145-amino-acid precursor called prepro-kisspeptin. Through proteolytic cleavage, this precursor produces several active fragments: kisspeptin-54, kisspeptin-14, kisspeptin-13, and kisspeptin-10. Each fragment shares the same C-terminal sequence, which is the portion that binds to the kisspeptin receptor (KISS1R, also known as GPR54). This means all variants activate the same signaling pathway, though they differ in potency and half-life.
The name itself has a surprisingly lighthearted origin. The gene was discovered in 1996 by researchers working in Hershey, Pennsylvania, and they named it after the city famous for Hershey Kisses chocolate. Originally, scientists called the protein "metastin" because the first known function was suppressing cancer metastasis in melanoma cell lines. The reproductive connection came later.
In 2003, two independent research groups changed everything. They discovered that loss-of-function mutations in the KISS1R gene caused a condition called hypogonadotropic hypogonadism, where the body fails to produce adequate testosterone or estrogen because the brain never signals the pituitary to release LH and FSH. Children with these mutations could not enter puberty naturally. That single finding proved kisspeptin was not just involved in reproduction. It was essential.
The HPG axis: how kisspeptin controls your hormones
To understand kisspeptin peptide benefits, you need to understand the hypothalamic-pituitary-gonadal axis. This three-level hormone cascade governs reproduction, sexual function, and a significant portion of overall endocrine health in both men and women.
Level one: the hypothalamus
Kisspeptin neurons reside primarily in two regions of the hypothalamus: the arcuate nucleus and the anteroventral periventricular nucleus (AVPV). These neurons do not work alone. They form part of what researchers call KNDy neurons, a term pronounced "candy," because they co-express three key signaling molecules: kisspeptin, neurokinin B (NKB), and dynorphin. Each plays a distinct role. Neurokinin B stimulates kisspeptin release in a pulsatile fashion. Dynorphin inhibits it. Together, they create the rhythmic on-off pattern that drives pulsatile GnRH secretion.
Why does pulsatility matter? Because GnRH must be released in pulses to function properly. Continuous GnRH exposure actually desensitizes pituitary receptors and shuts down LH and FSH production. This is how GnRH agonists used in prostate cancer treatment work: they flood the system with constant GnRH, initially causing a surge, then causing complete suppression. Kisspeptin ensures the pulses stay rhythmic and appropriate.
Level two: the pituitary
When kisspeptin stimulates GnRH neurons, GnRH travels through the hypothalamic-hypophyseal portal system to the anterior pituitary gland. There, it binds to GnRH receptors on gonadotroph cells, triggering the release of two critical hormones. Luteinizing hormone (LH) and follicle-stimulating hormone (FSH). In men, LH stimulates Leydig cells in the testes to produce testosterone. FSH acts on Sertoli cells to support sperm production. In women, LH triggers ovulation and progesterone production. FSH drives follicular development and estrogen synthesis.
Level three: the gonads
The gonads respond to LH and FSH by producing sex steroids and gametes. These steroids, testosterone in men and estrogen plus progesterone in women, then feed back to the hypothalamus, primarily through kisspeptin neurons. Here is the critical detail: GnRH neurons themselves lack the estrogen receptor alpha (ERalpha) needed for this feedback. The feedback loop runs through kisspeptin neurons, which do express ERalpha and progesterone receptors. Kisspeptin neurons are the central integrator of the entire system.
This means kisspeptin is not just a trigger. It is a sensor. It monitors sex steroid levels, integrates metabolic signals, processes stress information, and adjusts GnRH output accordingly. No other single peptide occupies this position in the reproductive axis. Understanding this architecture explains why peptides that work at the top of a cascade tend to have broader and more physiological effects than those that act further downstream.
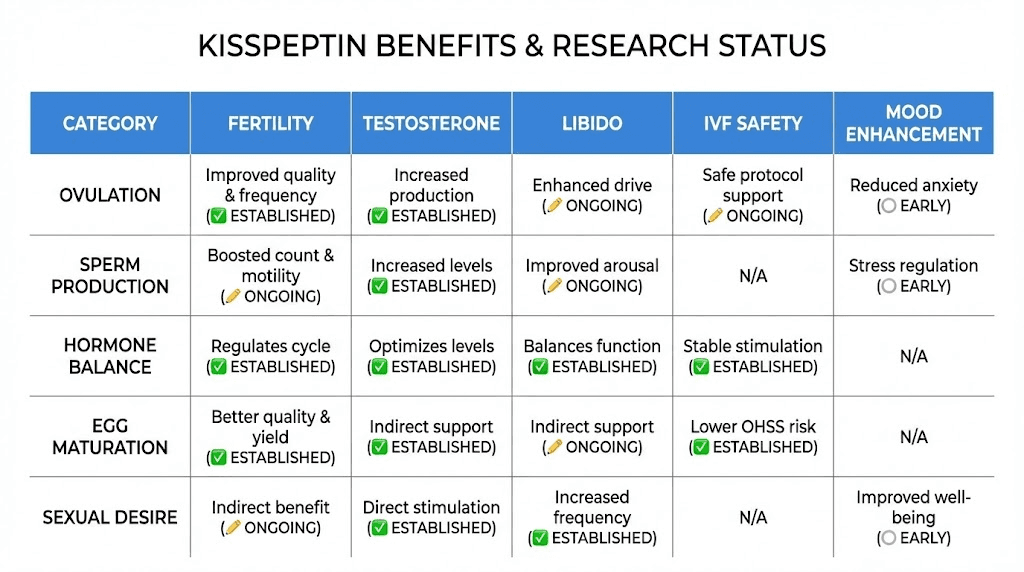
Kisspeptin peptide benefits: what the research shows
The clinical research on kisspeptin has expanded rapidly since those first genetic studies. What follows is not speculation. These are findings from published trials, many conducted by the team at Imperial College London under Professor Waljit Dhillo, one of the leading kisspeptin researchers in the world.
Testosterone and LH stimulation in men
One of the most robust findings is kisspeptin's ability to stimulate LH and testosterone in men. A study published in the Journal of Clinical Endocrinology and Metabolism administered kisspeptin-10 as an IV bolus at 0.3 nmol/kg to healthy men. Even at this modest dose, serum LH rose significantly. At higher doses, the response was dramatic.
When researchers infused kisspeptin-10 continuously at 4 micrograms per kilogram per hour for 22.5 hours, mean LH levels climbed from 5.4 IU/L to 20.8 IU/L. That is nearly a fourfold increase. Testosterone rose from 16.6 nmol/L to 24.0 nmol/L. The study also showed increased LH pulse frequency and pulse amplitude, confirming that kisspeptin was not just dumping LH into the bloodstream but actually increasing the pulsatile signaling that characterizes healthy endocrine function.
This matters enormously for anyone interested in natural hormone optimization. Unlike exogenous testosterone, which suppresses your own production through negative feedback, kisspeptin works from the top down. It tells your brain to make more of its own GnRH, which tells your pituitary to make more LH, which tells your testes to produce more testosterone. The entire axis stays active. Enclomiphene works on a similar principle, but at a different point in the cascade.
Sexual desire and brain processing
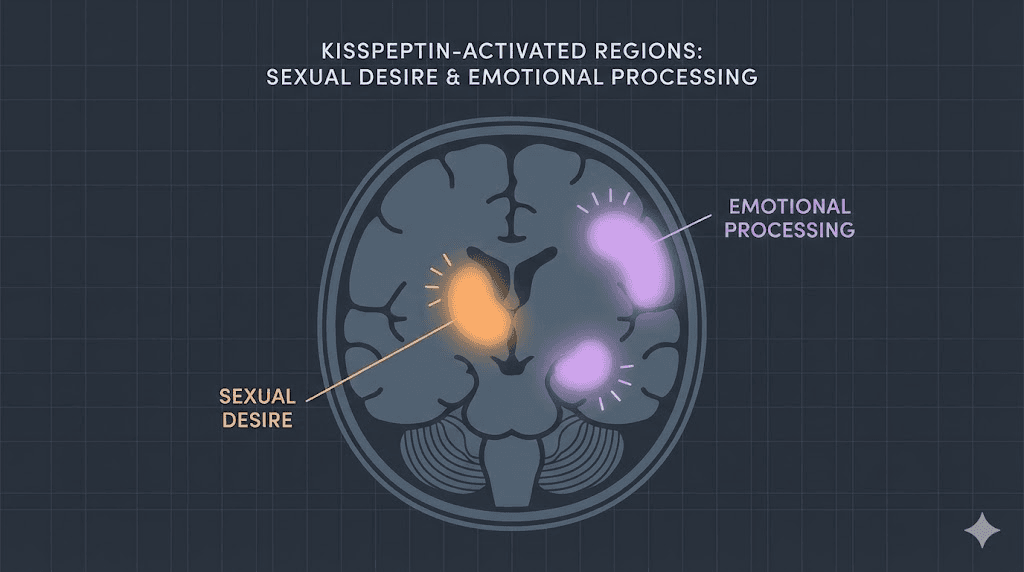
Perhaps the most surprising kisspeptin peptide benefits involve sexual behavior and brain processing. This is where the research gets genuinely fascinating.
In a randomized clinical trial published in JAMA Network Open, men with hypoactive sexual desire disorder (HSDD) received kisspeptin or placebo while undergoing functional MRI. During a video task, kisspeptin produced a marked increase in penile tumescence, providing the first direct evidence of kisspeptin's proerectile effects in humans. The peptide also enhanced brain activity in the limbic system, specifically regions associated with sexual arousal, reward processing, and emotional bonding. This correlated with improved mood and reduced sexual aversion.
A separate trial, also published in JAMA Network Open, examined 32 premenopausal women with HSDD. After kisspeptin administration, women reported increased feelings of being "sexy" on the Sexual Arousal and Desire Inventory. Brain imaging showed enhanced activity in the hippocampus, a region implicated in female sexual desire, and in the posterior cingulate cortex, which is involved in romantic love and reward. Kisspeptin also deactivated the inferior frontal gyrus, which reduced internal negative self-talk, and the secondary somatosensory cortex, reducing excessive self-focus on body image.
Let that sink in. A single peptide simultaneously enhanced sexual brain processing, reduced negative self-talk about body image, increased feelings of attraction, and improved mood. In both men and women. With no reported side effects.
For researchers exploring peptides for libido, kisspeptin represents a fundamentally different approach. Rather than directly manipulating blood flow or neurotransmitters like PT-141, it works through the reproductive hormone axis while simultaneously engaging emotional and behavioral circuits in the brain. SeekPeptides provides detailed protocol comparisons for members navigating these options.
Fertility and IVF applications
Kisspeptin's role in fertility is where the most advanced clinical work has been done. The problem it solves is serious. During standard IVF treatment, women receive supraphysiological doses of stimulatory hormones to mature multiple eggs. The final trigger for egg maturation has traditionally been human chorionic gonadotropin (hCG). But hCG carries a significant risk: ovarian hyperstimulation syndrome (OHSS).
OHSS is not a minor inconvenience. It can cause massive ovarian enlargement, fluid accumulation in the abdomen and chest, kidney failure, blood clots, respiratory distress, and in rare cases, death. It remains one of the most dangerous complications of IVF treatment.
Kisspeptin offers a safer alternative. Because it works at the top of the axis rather than directly on the ovaries, it produces a more physiological LH surge. The ovaries respond by maturing eggs, but without the prolonged, excessive stimulation that hCG causes.
In the landmark trial by Jayasena and colleagues, kisspeptin-54 triggered egg maturation in a dose-dependent manner. Fertilization and embryo transfer occurred in 92% of patients. Biochemical pregnancy rates reached 40%, and clinical pregnancy rates were 23%. A subsequent phase 2 trial specifically enrolled women at high risk for OHSS and confirmed that kisspeptin-54 could safely and effectively trigger oocyte maturation in this vulnerable population.
The numbers speak for themselves. Across early trials, kisspeptin-triggered IVF cycles resulted in 73 healthy babies born, with none of the mothers developing OHSS. This represents a fundamental safety improvement over traditional hCG triggers.
A 2025 review published in the Journal of Clinical Medicine found that kisspeptin analogs offer a primary advantage through their short action on LH receptors, making them inherently safer for inducing ovulation compared to recombinant hCG. The review also noted emerging applications in cryopreservation and in vitro maturation of oocytes.
Hypothalamic amenorrhea
Hypothalamic amenorrhea is a condition where women lose their menstrual periods due to insufficient GnRH signaling. Common causes include extreme exercise, severe caloric restriction, and chronic stress. The condition affects fertility, bone density, cardiovascular health, and overall wellbeing.
Research shows that kisspeptin can restore LH pulsatility in women with hypothalamic amenorrhea, essentially restarting the reproductive axis from the top. This is particularly promising because it addresses the root cause rather than bypassing it. Instead of giving exogenous hormones, kisspeptin tells the body to resume its own hormone production.
However, there is an important nuance. A study examining twice-daily subcutaneous kisspeptin injections at 6.4 mcg/kg in women with hypothalamic amenorrhea found robust initial responses, but efficacy declined by day 14 due to tachyphylaxis, the desensitization of kisspeptin receptors with sustained exposure. This finding has shaped how researchers think about dosing protocols, favoring intermittent or pulsatile administration over continuous exposure.
Anxiety and emotional processing
Kisspeptin receptors are not limited to the hypothalamus. They are expressed in the amygdala, hippocampus, and other limbic structures involved in emotional processing. This has led researchers to investigate kisspeptin's effects on anxiety and mood.
Intracranial administration of kisspeptin to zebrafish stimulates exploratory behavior and attenuates anxiety-like responses. Selective chemogenetic stimulation of kisspeptin neurons in the rodent amygdala produces similar effects. In humans, a dedicated investigation of kisspeptin's effects on anxiety, the first of its kind, analyzed data from 95 male and female participants. The findings showed that kisspeptin stimulated reproductive hormones without negatively affecting anxiety measures.
This is relevant because many peptides for anxiety work through entirely different mechanisms. Kisspeptin appears to positively modulate emotional circuits while simultaneously enhancing reproductive function, a combination unique in the peptide landscape.
Cancer research applications
Remember that kisspeptin was originally discovered as a metastasis suppressor. The KISS1 gene product inhibits the spread of melanoma cells. Research has continued to explore this anticancer potential across multiple tumor types.
More recently, a different therapeutic angle has emerged. Prolonged kisspeptin agonism can induce testosterone suppression through receptor desensitization, similar to how GnRH agonists work. Phase 1 clinical trials are investigating this approach for prostate cancer treatment. The advantage over GnRH agonists is that kisspeptin works upstream, potentially offering more physiological modulation with fewer side effects during the initial flare period.
Metabolic integration
Kisspeptin neurons receive input from metabolic sensors throughout the body. They express receptors for leptin, insulin, and ghrelin, allowing them to adjust reproductive signaling based on energy availability. This explains why severe caloric restriction suppresses fertility: low leptin levels reduce kisspeptin expression, which reduces GnRH, which reduces LH and FSH, which shuts down reproductive function.
For researchers interested in peptides for weight loss, this metabolic link is significant. It suggests that kisspeptin sits at the intersection of metabolic and reproductive health, a connection that compounds like cagrilintide and semaglutide do not directly address.
Kisspeptin-10 vs kisspeptin-54: which variant and why
Understanding the different kisspeptin variants matters for practical application. They are not interchangeable.
Kisspeptin-10
Kisspeptin-10 is the shortest active fragment, consisting of the 10 C-terminal amino acids of the full-length peptide. It retains full receptor binding activity. Its half-life is approximately 4 minutes in circulation, though downstream effects persist for hours because the GnRH and LH cascades it triggers have their own kinetics. Most bodybuilding and research community protocols use kisspeptin-10 because it is readily available and easier to dose predictably.
Clinical data in men show that IV kisspeptin-10 at doses as low as 0.3 nmol/kg reliably elevates serum LH. Subcutaneous protocols in research contexts typically reference 100 to 200 mcg per injection, though this is based on limited clinical guidance rather than large-scale trials.
Kisspeptin-54
Kisspeptin-54 is the full-length mature peptide. It has a longer half-life than kisspeptin-10 and produces more sustained LH responses. Most IVF research uses kisspeptin-54 because the longer duration of action better supports the egg maturation process, which requires sustained LH elevation over several hours.
Clinical IVF doses range from 1.6 to 12.8 nmol/kg, administered as a single subcutaneous injection. The dose-dependent response has been well characterized, with 6.4 and 12.8 nmol/kg producing the most consistent oocyte maturation.
Choosing between variants
For testosterone and LH stimulation research, kisspeptin-10 is the more practical choice due to availability and established subcutaneous protocols. For fertility and IVF applications, kisspeptin-54 is preferred due to its longer action and more extensive clinical data in that context. Both variants bind the same receptor and activate the same downstream pathways.
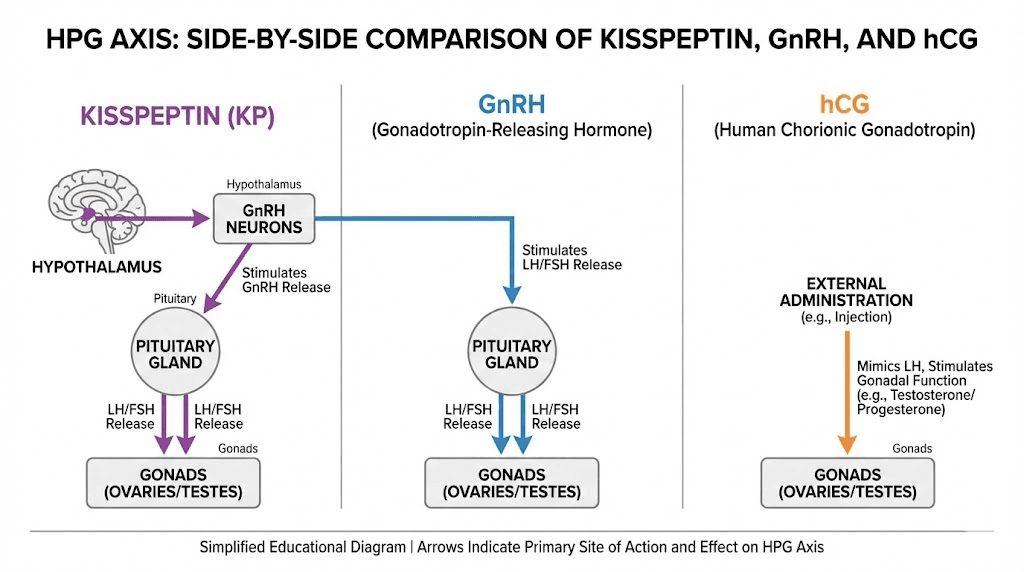
How kisspeptin compares to hCG and GnRH analogs
Researchers frequently ask how kisspeptin stacks up against other compounds that stimulate the reproductive axis. The comparison is straightforward once you understand where each agent acts.
Site of action
Kisspeptin acts at the very top of the HPG axis, on GnRH neurons in the hypothalamus. GnRH and its analogs (like gonadorelin) act one level down, directly on the pituitary. hCG acts at the bottom, directly on the gonads by mimicking LH. This hierarchy matters because higher-level interventions produce more physiological downstream responses, while lower-level interventions are more direct but less nuanced.
Testosterone stimulation comparison
hCG is well established for testosterone stimulation. A study in men with average total testosterone of 361.8 ng/dL found that six months of 2000 IU weekly hCG raised mean testosterone to 519.8 ng/dL. The response is reliable and well characterized.
Kisspeptin-10 can stimulate testosterone production within 30 to 40 minutes of administration. However, its short half-life means the effect is transient without repeated dosing. Continuous infusion of kisspeptin-10 at 4 mcg/kg/hour raised testosterone from 16.6 to 24.0 nmol/L (approximately 479 to 692 ng/dL) in healthy men over a 22.5-hour period. The magnitude is comparable to hCG, but the kinetics are completely different.
IVF trigger comparison
A prospective analysis of 499 IVF cycles compared all three trigger agents. Peak hormone levels differed significantly. hCG levels peaked at 121 IU/L at 24 hours. LH peaked at approximately 140 IU/L at 4 hours following GnRH agonist trigger, and at approximately 41 IU/L at 4 hours following kisspeptin trigger. The lower LH peak with kisspeptin is precisely why it carries a lower OHSS risk. The stimulation is sufficient for egg maturation without the excessive, prolonged ovarian stimulation that causes hyperstimulation.
Safety comparison
Feature | Kisspeptin | GnRH agonist | hCG |
|---|---|---|---|
Site of action | Hypothalamus (top) | Pituitary (middle) | Gonads (bottom) |
Half-life | Very short (4 min for Kp-10) | Short (minutes) | Long (days) |
OHSS risk | Lowest | Lower than hCG | Highest |
FDA approved | No | Yes (various forms) | Yes |
Testicular atrophy risk | Minimal (preserves axis) | Minimal | Low (direct stimulation) |
Tachyphylaxis | Yes (with continuous use) | Yes (with continuous use) | Minimal |
For men using TRT who want to maintain fertility and testicular function, kisspeptin offers an interesting alternative to hCG.
While hCG directly stimulates the testes, kisspeptin preserves the entire axis from top to bottom.
The tradeoff is dosing frequency. hCG stays active for days. Kisspeptin requires daily or every-other-day administration to maintain consistent stimulation. SeekPeptides members can explore detailed protocol comparisons that account for these practical differences.
Kisspeptin dosing protocols in research
Dosing kisspeptin is more nuanced than most peptides because of the tachyphylaxis risk and the significant differences between routes of administration. Here is what the clinical data shows.
Intravenous protocols (clinical research)
Most published clinical data uses IV administration. For kisspeptin-10, effective IV bolus doses range from 0.3 to 1.0 nmol/kg for acute LH stimulation. Continuous IV infusion at 1.5 to 4 mcg/kg/hour for up to 22.5 hours produces sustained LH and testosterone elevation. These protocols are impractical outside clinical settings but establish the effective dose range and confirm the biological response.
Subcutaneous protocols (research context)
Subcutaneous administration is more practical for ongoing research. Published references suggest 100 to 200 mcg of kisspeptin-10 per injection. The typical approach involves single daily injections rather than continuous administration. Researchers in the bodybuilding community often reference 100 to 500 mcg per dose, though data at the higher end comes from anecdotal reports rather than controlled trials.
The critical consideration is frequency. Because kisspeptin's half-life is measured in minutes, not hours, single injections produce transient spikes in LH and testosterone. For sustained elevation, researchers use pulse-style dosing, one to two injections daily rather than continuous administration. This mimics the natural pulsatile pattern and reduces the risk of receptor desensitization.
Intranasal protocols (emerging research)
A groundbreaking study published in 2025 demonstrated that intranasal kisspeptin-54 rapidly stimulates gonadotropin release in healthy men and women, and in patients with hypothalamic amenorrhea. The dose of 12.8 nmol/kg administered intranasally induced clinically significant increases in serum LH across all study groups. No side effects or adverse events were reported.
This represents the first non-invasive method to robustly and safely stimulate gonadotropins with kisspeptin. If validated in larger trials, intranasal delivery could dramatically improve the practical utility of kisspeptin for both clinical and research applications. For researchers currently using nasal spray peptides, this is a development worth following closely.
IVF trigger protocols
For IVF egg maturation, kisspeptin-54 is administered as a single subcutaneous injection at 6.4 to 12.8 nmol/kg. This is a one-time dose, not a repeated protocol. The timing is critical, typically administered 36 hours before oocyte retrieval, replacing the traditional hCG trigger.
Tachyphylaxis: the key dosing challenge
Repeated kisspeptin administration leads to receptor desensitization. A study in women with hypothalamic amenorrhea found that twice-daily subcutaneous injections produced strong initial LH responses that declined significantly by day 14. This phenomenon, called tachyphylaxis, is the primary limitation of kisspeptin as a chronic therapy.
Practical implications for researchers:
Avoid continuous daily dosing beyond 2 weeks without breaks
Consider pulsatile protocols (once daily or every other day)
Cycle kisspeptin administration (2 weeks on, 1-2 weeks off)
Monitor LH response to detect early signs of desensitization
This cycling approach is familiar to anyone experienced with peptide cycling. The same principle applies: periodic breaks allow receptor sensitivity to recover. Use our peptide calculator to plan doses based on your specific reconstitution method.
Women and cycle-phase sensitivity
For women using peptides, kisspeptin response varies dramatically across the menstrual cycle. The preovulatory phase produces the strongest response: a 10 mcg/kg IV bolus reliably elevates both LH and FSH. During the early follicular phase, the response is far weaker, with only 50% of women responding to a 0.24 mcg/kg IV bolus. This sexual dimorphism and cycle-phase sensitivity is unique among reproductive peptides and must be factored into any research protocol involving female subjects.
Kisspeptin for post-cycle therapy
The bodybuilding and research community has taken particular interest in kisspeptin as a post-cycle therapy (PCT) agent. The rationale is compelling. After a cycle of anabolic compounds, the HPG axis is suppressed. LH is low. Testicular function is diminished. Natural testosterone production has been replaced by exogenous sources that are now discontinued.
Traditional PCT relies on selective estrogen receptor modulators (SERMs) like clomiphene and tamoxifen, which block estrogen's negative feedback at the hypothalamus and pituitary, thereby increasing GnRH, LH, and FSH. hCG directly stimulates the testes to maintain size and function during the cycle, but its use in PCT is more controversial due to potential desensitization of Leydig cells.
Kisspeptin offers a different approach. By acting at the very top of the cascade, it essentially presses the restart button on the entire HPG axis. It stimulates GnRH release, which stimulates LH and FSH release, which stimulates testicular function. The entire pathway is engaged from the top down, promoting genuine recovery rather than artificially propping up one level of the cascade.
However, the tachyphylaxis issue limits its utility as a standalone PCT agent for extended protocols. Researchers exploring kisspeptin for PCT often combine it with other compounds or use it in short bursts (5 to 10 days) to jumpstart the axis, followed by more sustainable interventions. For a comprehensive understanding of post-cycle recovery options, comparing peptides to steroids provides essential context. Many researchers also explore testosterone boosters versus peptides when planning recovery protocols.
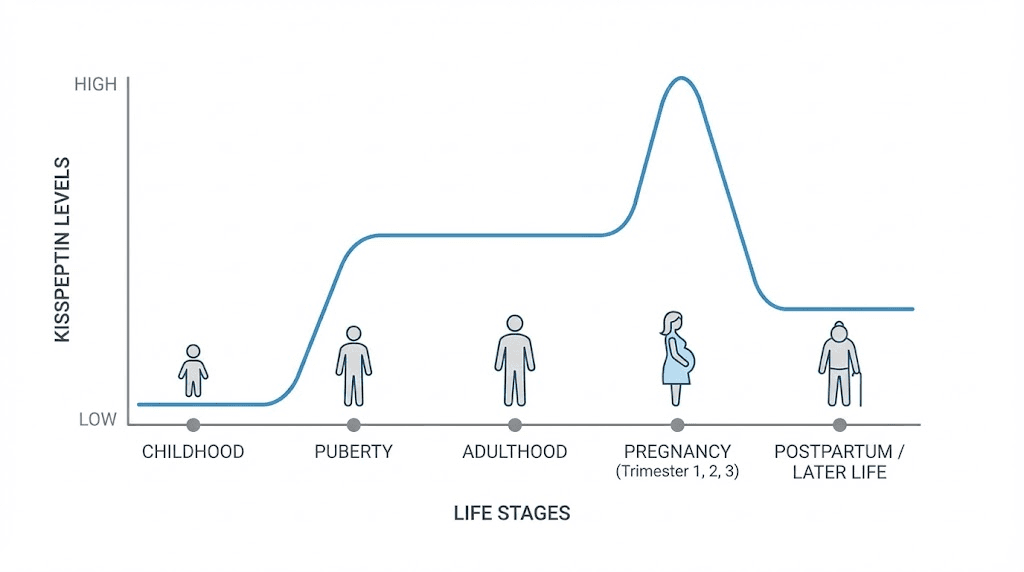
Kisspeptin and pregnancy
Kisspeptin levels change dramatically during pregnancy. Circulating levels increase massively, far exceeding non-pregnant concentrations. The placenta becomes a major source of kisspeptin production, and the peptide plays a role in regulating placenta formation and vascular remodeling.
Research suggests that women with lower kisspeptin levels during early pregnancy may be more susceptible to complications, including miscarriage. This has led to investigation of kisspeptin as a blood test biomarker for predicting pregnancy outcomes. Low kisspeptin levels in the first trimester could potentially identify high-risk pregnancies before clinical symptoms appear.
For researchers interested in peptides and pregnancy, kisspeptin represents one of the few compounds with a direct, physiological role in pregnancy maintenance. This is not off-label speculation. The placenta naturally produces kisspeptin in massive quantities throughout healthy pregnancy.
Kisspeptin and puberty
Kisspeptin is the gatekeeper of puberty. The developmental increase in kisspeptin expression triggers the cascade of hormonal changes that initiate sexual maturation. Mouse models with disrupted kisspeptin or KISS1R genes fail to undergo puberty entirely, and both sexes are infertile with poor gonadal growth.
In humans, loss-of-function mutations in the kisspeptin pathway cause hypogonadotropic hypogonadism and absent puberty. Conversely, gain-of-function mutations can cause precocious puberty, where children enter sexual development years earlier than normal. These opposing extremes demonstrate how precisely kisspeptin calibrates the timing and intensity of pubertal activation.
This pubertal role explains why kisspeptin must be used cautiously. In prepubertal individuals, exogenous kisspeptin could theoretically accelerate pubertal development. In adults, this concern is irrelevant, but it underscores the peptide's potency as a reproductive axis regulator.
Safety profile and side effects
The safety data on kisspeptin is more reassuring than for most research peptides, primarily because it has been studied in controlled clinical trials with proper oversight.
Clinical trial safety data
Kisspeptin has been administered to more than 500 men and women in clinical trials without serious adverse events. In the HSDD trials, kisspeptin was well tolerated with no reported side effects. Blood pressure and heart rate were unaffected. In IVF trials, kisspeptin-54 was administered at various doses (1.6 to 12.8 nmol/kg) with no OHSS cases in the kisspeptin-triggered group.
Reported mild effects
When side effects do occur, they tend to be mild and transient. These include injection site reactions (redness, swelling, mild pain), occasional headaches, and mild abdominal discomfort. These are consistent with typical peptide injection side effects rather than kisspeptin-specific concerns.
Key safety considerations
FDA status. Kisspeptin does not have FDA approval for any medical use. The FDA has classified it as presenting substantial safety risks for compounding, which limits its availability through regulated pharmacy channels.
Cardiovascular effects. Kisspeptin has documented effects on blood vessels, including potential vasoconstriction. People with existing cardiovascular conditions should exercise particular caution. The clinical significance of this effect in typical research doses is unclear, but it warrants monitoring, especially in individuals with pre-existing heart disease. For a broader perspective on peptide safety, comprehensive understanding of cardiovascular considerations is essential.
Hormonal overproduction risk. Excessive kisspeptin could theoretically cause overproduction of gonadotropic hormones. While this is unlikely at typical research doses, it reinforces the importance of conservative dosing and monitoring, particularly for individuals new to reproductive peptides.
Tachyphylaxis as a safety mechanism. Ironically, kisspeptin's tendency toward receptor desensitization may serve as a built-in safety mechanism. Continuous overstimulation is self-limiting because the receptors downregulate. This is different from hCG, where persistent ovarian stimulation can cause OHSS precisely because the long half-life maintains continuous receptor activation.
Long-term unknowns. No long-term safety studies exist for repeated kisspeptin administration. Existing data covers acute and short-term use (days to weeks). How chronic or repeated cyclical use affects the HPG axis over months or years remains an open question.
Populations that should avoid kisspeptin:
Pregnant or breastfeeding women (effects on fetal development unknown)
Children and adolescents (risk of affecting pubertal timing)
Individuals with hormone-sensitive cancers (breast, prostate, ovarian)
People on other hormone therapies without medical supervision
For anyone prioritizing safety, understanding proper peptide storage and reconstitution techniques is equally important. A perfectly dosed peptide stored improperly is a wasted peptide.
Kisspeptin stacking considerations
Researchers often ask about combining kisspeptin with other peptides. Because kisspeptin acts at the top of the HPG axis, interactions with other reproductive compounds are particularly important to consider.
Kisspeptin with hCG
This combination provides top-down and bottom-up stimulation simultaneously. Kisspeptin activates the brain to release GnRH, while hCG directly stimulates the gonads. The theory is comprehensive axis activation. Some TRT patients use this approach to maximize testicular function preservation while maintaining natural GnRH signaling. The risk is overstimulation, and no controlled trials have evaluated this specific combination.
Kisspeptin with enclomiphene
Both compounds ultimately increase GnRH and LH, but through different mechanisms. Kisspeptin directly stimulates GnRH neurons. Enclomiphene blocks estrogen feedback at the hypothalamic and pituitary level, releasing the brake on GnRH production. Whether combining them produces synergistic or redundant effects is unknown. The theoretical risk is excessive LH stimulation.
Kisspeptin with BPC-157 or TB-500
These combinations serve entirely different purposes. BPC-157 and TB-500 are tissue repair peptides with no direct interaction with the HPG axis. There is no known contraindication to using them alongside kisspeptin, but there is also no synergistic benefit. They address completely different biological systems. For those exploring peptide stacking, understanding which compounds interact and which operate independently is essential.
Kisspeptin with growth hormone secretagogues
Compounds like ipamorelin, CJC-1295, and sermorelin stimulate growth hormone release through the GH axis, which is separate from the HPG axis. No direct interaction with kisspeptin is expected. Researchers sometimes combine reproductive and GH-releasing peptides to address multiple goals simultaneously, though this approach lacks controlled trial data.
For any multi-peptide protocol, the standard advice applies: start with one compound to establish baseline responses before adding complexity. Use our peptide stack calculator to plan combinations carefully.
Kisspeptin for men: practical applications
The male-specific applications of kisspeptin center on three areas: testosterone optimization, fertility preservation, and sexual function enhancement.
Natural testosterone optimization
Men seeking to increase testosterone without exogenous replacement find kisspeptin appealing because it works entirely through the body's own production machinery. Unlike TRT, which suppresses natural production, kisspeptin enhances it. The limitation is duration of effect. Single injections produce transient testosterone spikes. Sustained optimization requires regular, carefully timed administration with periodic breaks to avoid receptor desensitization.
Researchers report that the 100 to 500 mcg subcutaneous range provides consistent and predictable LH responses in men with functional hypothalamic signaling. Those with primary hypogonadism, where the problem is testicular failure rather than insufficient signaling, will not benefit because kisspeptin cannot force damaged testes to produce testosterone.
Fertility preservation during TRT
Exogenous testosterone suppresses the HPG axis, reducing sperm production to near zero in many men. hCG has traditionally been the solution, maintaining testicular stimulation while on TRT. Kisspeptin offers a potentially superior approach because it preserves the entire axis from hypothalamus through gonads, not just the final step.
Some clinicians describe kisspeptin as mimicking the actions of both clomiphene and hCG simultaneously, maintaining fertility while deterring testicular atrophy. This positions it as a single-agent solution for a problem that currently requires multiple compounds. For men exploring this area, understanding HMG peptide and hCG alternatives provides important comparison points.
Libido and sexual function
The JAMA Network Open trial in men with HSDD showed kisspeptin enhanced penile tumescence, improved sexual brain processing, and reduced sexual aversion. For men whose low libido stems from insufficient hormonal signaling rather than purely psychological factors, kisspeptin addresses the root cause at the endocrine level while simultaneously engaging neural circuits involved in desire and arousal.
This dual mechanism, hormonal plus neural, distinguishes kisspeptin from both PT-141 (which works primarily through melanocortin receptors in the brain) and phosphodiesterase inhibitors like sildenafil (which work on blood flow). Kisspeptin occupies a unique therapeutic niche by addressing desire, arousal, and hormonal production simultaneously. Peptides for erectile dysfunction work through various mechanisms, and understanding these differences helps researchers choose the most appropriate approach.
Kisspeptin for women: practical applications
Women's applications span fertility treatment, menstrual restoration, sexual desire enhancement, and pregnancy monitoring.
IVF egg maturation trigger
This is the most clinically advanced application. Kisspeptin-54 as an IVF trigger has produced 73 healthy babies in early trials with zero OHSS cases. For women at high risk of OHSS, kisspeptin offers a fundamentally safer alternative to hCG. The approach is progressing through clinical trials and could eventually become standard practice in fertility clinics.
Restoring menstrual cycles
Women with hypothalamic amenorrhea from excessive exercise, caloric restriction, or stress may benefit from kisspeptin's ability to restart LH pulsatility. The challenge is maintaining the effect without tachyphylaxis. Current research suggests intermittent administration schedules may overcome this limitation, though optimal protocols are still being developed.
Sexual desire enhancement
The JAMA Network Open trial in women with HSDD showed kisspeptin enhanced sexual and attraction brain processing. Unlike currently available HSDD treatments in the US (flibanserin and bremelanotide), which carry significant side effects including nausea, drowsiness, and alcohol interactions, kisspeptin was well tolerated with no reported side effects. Research is expanding to include postmenopausal women, where HSDD prevalence ranges from 9 to 26% and no approved treatments currently exist.
Pregnancy biomarker potential
Blood kisspeptin levels could serve as a predictive biomarker for pregnancy complications. Lower first-trimester kisspeptin levels correlate with increased miscarriage risk. If validated, a simple kisspeptin blood test could identify high-risk pregnancies early enough for intervention. For women researching peptides for menopause and reproductive health transitions, kisspeptin adds an important dimension to the conversation.
Women also interested in peptides for perimenopause should note that kisspeptin levels naturally decline with age, particularly around menopause. Whether exogenous kisspeptin can meaningfully counteract menopausal hormonal changes is an active area of investigation. The connection between kisspeptin and peptide needs for women over 40 is becoming increasingly relevant as the research expands.
Reconstitution and handling
Kisspeptin-10 is typically supplied as a lyophilized (freeze-dried) powder. Proper handling follows the same principles as other lyophilized peptides.
Storage before reconstitution
Store lyophilized kisspeptin at -20C for long-term storage or 2-8C (refrigerated) for short-term storage. Unreconstituted peptide maintains stability for months under proper conditions. Keep away from light and moisture. For a detailed breakdown of temperature and shelf-life considerations, our peptide storage guide covers everything you need.
Reconstitution
Reconstitute with bacteriostatic water (not sterile water, unless you plan to use the entire vial immediately). Direct the stream of water against the vial wall, allowing it to run down gently. Do not shake. Swirl gently if needed. Use our peptide reconstitution calculator to determine exact volumes for your target concentration.
Storage after reconstitution
Reconstituted kisspeptin should be stored at 2-8C (refrigerator). Use within 2-3 weeks for optimal potency. Do not freeze reconstituted solution. Given kisspeptin-10's short half-life in circulation, maintaining peptide stability before injection is especially important. Every percentage of degradation matters more with a compound that already works in minutes rather than hours. For specific guidance on how long reconstituted peptides last, check our dedicated storage resources.
Testing and quality
Given the lack of FDA-regulated kisspeptin products, quality verification is critical. Third-party testing for purity, identity, and sterility should be considered mandatory. When evaluating sources, the same principles that apply to choosing peptide vendors apply here: independent COAs, HPLC purity data, and mass spectrometry confirmation. Our guide on peptide testing labs can help you verify what you receive.
Kisspeptin in the broader peptide landscape
Where does kisspeptin fit among the hundreds of peptides researchers use? Its niche is specific and important.
Kisspeptin is not a tissue repair peptide like BPC-157 or tissue repair compounds. It is not a growth hormone secretagogue like ipamorelin. It is not a fat loss peptide like AOD-9604 or a fat burning peptide. It is not a nootropic like semax or nootropic peptides.
Kisspeptin is the master regulator of the reproductive axis. Period.
Its closest comparisons are to compounds like enclomiphene and hCG, which also modulate the HPG axis but at different levels. What makes kisspeptin unique is its position at the very top of the cascade, plus its additional effects on brain circuits governing desire, arousal, and emotional processing. No other compound in the peptide researcher's toolkit operates at this intersection of endocrine regulation and neurobehavioral modulation.
For researchers building comprehensive protocols, kisspeptin complements rather than competes with most other peptide categories. You can pursue injury recovery with BPC-157, muscle growth with growth hormone secretagogues, and hormonal optimization with kisspeptin, all without direct pharmacological conflict. The key is managing injection frequency and monitoring markers for each category independently. SeekPeptides members access protocol builders that account for these multi-compound scenarios.
Common mistakes researchers make with kisspeptin
Understanding what goes wrong is as important as understanding what goes right.
Mistake 1: treating it like hCG
hCG has a half-life measured in days. One injection provides sustained gonadal stimulation. Kisspeptin-10 has a half-life of approximately 4 minutes. Using the same dosing schedule as hCG, injecting once or twice weekly, will produce almost no sustained effect. Kisspeptin requires daily administration for consistent results.
Mistake 2: continuous dosing without breaks
Tachyphylaxis is real. Researchers who dose kisspeptin daily for weeks without interruption often see diminishing responses. The solution is cycling: 2 weeks on, 1-2 weeks off, or pulse-style protocols that allow receptor recovery.
Mistake 3: expecting results with primary hypogonadism
Kisspeptin works by telling your brain to signal your gonads. If the gonads are damaged or non-functional, no amount of upstream signaling will produce testosterone or mature eggs. Kisspeptin requires functional gonads to deliver its benefits. This is a fundamental distinction from hCG, which directly stimulates gonadal function and may produce some response even with partial gonadal impairment.
Mistake 4: ignoring the variant difference
Kisspeptin-10 and kisspeptin-54 are not interchangeable in terms of half-life and clinical application. Using kisspeptin-10 for IVF triggering, for example, would likely be insufficient because the LH surge duration is too short for reliable oocyte maturation. Conversely, kisspeptin-54 may be unnecessarily complex for simple testosterone optimization where kisspeptin-10's rapid kinetics are adequate.
Mistake 5: skipping blood work
Any protocol that modulates the HPG axis demands baseline and follow-up bloodwork. At minimum, check LH, FSH, total testosterone, free testosterone, estradiol, and prolactin before starting. Repeat at 2-week intervals to track response and detect any adverse shifts. Without data, you are guessing. For a full understanding of what to monitor, our peptide research guide outlines the essential biomarkers.
The future of kisspeptin research
Kisspeptin research is moving in several directions simultaneously.
Intranasal delivery. The 2025 demonstration of effective intranasal kisspeptin-54 could transform accessibility. Non-invasive delivery removes the injection barrier and opens possibilities for on-demand use, particularly for sexual dysfunction applications.
HSDD treatment development. Both Imperial College London and collaborating institutions are planning larger-scale trials of kisspeptin for hypoactive sexual desire disorder. If these succeed, kisspeptin could become the first treatment that improves sexual desire in both men and women through the same mechanism. Current HSDD treatments are sex-specific and carry significant side effect burdens.
IVF protocol integration. Phase 3 trials are anticipated to further establish kisspeptin-54 as a standard IVF trigger, particularly for OHSS-prone patients. The safety data already supports this application, and the clinical community is increasingly receptive.
Long-acting analogs. The short half-life is kisspeptin's primary practical limitation. Research into modified kisspeptin analogs with extended duration of action could address this, potentially creating weekly or biweekly formulations that maintain efficacy without tachyphylaxis.
Cancer applications. The dual potential of kisspeptin in cancer, as both a metastasis suppressor and a tool for androgen deprivation through receptor desensitization, continues to attract research interest.
Metabolic-reproductive crossover. Understanding how kisspeptin integrates metabolic and reproductive signaling could lead to applications in conditions where both systems are disrupted: polycystic ovary syndrome, obesity-related infertility, anorexia-related amenorrhea, and diabetes-related reproductive dysfunction.
The pace of kisspeptin research has accelerated significantly since the first clinical trials. What was an obscure neuropeptide a decade ago is rapidly becoming one of the most promising therapeutic targets in reproductive medicine. Researchers who understand this peptide now will be well positioned as these clinical applications mature.
Frequently asked questions
What is kisspeptin and what does it do?
Kisspeptin is a neuropeptide produced in the hypothalamus that acts as the master regulator of the reproductive hormone axis. It stimulates the release of GnRH, which triggers LH and FSH production, which in turn drives testosterone production in men and estrogen plus ovulation in women. It also influences sexual desire, emotional processing, and metabolic-reproductive integration.
Does kisspeptin increase testosterone?
Yes. Clinical trials show that kisspeptin-10 significantly increases both LH and testosterone in men. Continuous infusion raised testosterone from approximately 479 to 692 ng/dL in healthy volunteers. The effect works through natural production pathways rather than exogenous hormone replacement, meaning the testes produce their own testosterone in response to kisspeptin-driven LH stimulation.
How is kisspeptin different from hCG?
Kisspeptin acts at the top of the HPG axis (hypothalamus), while hCG acts at the bottom (gonads). Kisspeptin stimulates the entire cascade from brain to gonads. hCG bypasses the brain and directly stimulates gonadal function. Kisspeptin has a much shorter half-life (minutes vs days), requires more frequent dosing, but produces a more physiological hormone profile with lower risk of ovarian hyperstimulation.
Can kisspeptin help with fertility?
Kisspeptin-54 has successfully triggered egg maturation in IVF patients, with 73 healthy babies born in early trials and zero cases of ovarian hyperstimulation syndrome. It also restores LH pulsatility in women with hypothalamic amenorrhea. In men, it enhances LH, FSH, and testosterone production, all of which support male fertility by improving sperm production.
What are the side effects of kisspeptin?
Clinical trials report minimal side effects. Over 500 participants have received kisspeptin without serious adverse events. Mild effects include injection site reactions, occasional headache, and mild abdominal discomfort. The main concern is tachyphylaxis with prolonged use and potential cardiovascular effects in susceptible individuals. Review our peptide safety guide for comprehensive risk management.
Is kisspeptin FDA approved?
No. Kisspeptin is not FDA approved for any medical use. It remains an investigational compound used in clinical research. The FDA has classified it as presenting substantial safety risks for compounding. All use outside of clinical trials is considered off-label research.
How long does kisspeptin last in the body?
Kisspeptin-10 has a circulating half-life of approximately 4 minutes. Kisspeptin-54 has a longer half-life but is still measured in minutes to hours. However, the downstream effects (LH release, testosterone production) persist for several hours because the hormones kisspeptin triggers have their own, longer half-lives. Proper peptide dosing accounts for this distinction between peptide half-life and effect duration.
Can women use kisspeptin?
Yes. Clinical trials have included women for IVF, HSDD, hypothalamic amenorrhea, and reproductive hormone studies. Response varies significantly by menstrual cycle phase, with the preovulatory phase producing the strongest effects. Women using peptides should work with knowledgeable practitioners who understand these cycle-dependent variations.
Does kisspeptin work for low libido?
Randomized clinical trials show kisspeptin enhances sexual brain processing and improves psychometric measures of desire in both men and women with HSDD. In men, it increased penile tumescence during sexual stimuli. In women, it enhanced brain activity in desire-related regions and increased self-reported feelings of sexual arousal. PT-141 nasal spray is a more established option for acute libido enhancement, but kisspeptin addresses the hormonal root cause simultaneously.
Can I stack kisspeptin with other peptides?
Kisspeptin acts on the reproductive axis and does not directly interact with tissue repair peptides (like BPC-157 or TB-500), growth hormone secretagogues (like ipamorelin or CJC-1295), or weight loss peptides. Combining kisspeptin with other HPG-axis compounds (hCG, enclomiphene) requires careful planning due to overlapping effects. Check our peptide cycling guide for safe combination strategies.
For researchers serious about optimizing their reproductive health protocols, SeekPeptides offers the most comprehensive resource available, with evidence-based guides, proven protocols, and a community of thousands who have navigated these exact questions.



