Feb 3, 2026
Six weeks of physical therapy. Steroid injections. Anti-inflammatory medications that upset your stomach. And still, that burning pain shoots down your leg every time you bend forward. If this sounds familiar, you are not alone. Herniated discs affect roughly 2% of the general population at any given time, with the L4-L5 and L5-S1 levels accounting for approximately 95% of lumbar herniations. The conventional treatment path works for many people, with over 85% of acute cases resolving within 8 to 12 weeks of conservative care. But what about the rest? What about the cases that linger for months or years, resisting every standard intervention?
That is where peptides enter the conversation.
Peptides like BPC-157, TB-500, and GHK-Cu have generated serious interest among researchers studying connective tissue repair, nerve regeneration, and inflammation modulation. They are not miracle cures. They are not FDA-approved treatments for disc herniations. But the preclinical data, combined with growing clinical observations, suggests these compounds may support disc healing through mechanisms that conventional treatments simply do not address. SeekPeptides has become the go-to resource for researchers navigating these protocols, and this guide will walk you through everything the current evidence reveals about using peptides for herniated disc recovery.
We will cover the anatomy of disc herniations, the specific peptides being studied, research-backed protocols, realistic timelines, and the critical safety considerations you need to understand before incorporating any peptide into a recovery plan. This is not a surface-level overview. This is the comprehensive reference that brings together the science, the practical protocols, and the honest limitations of peptide therapy for spinal disc injuries.
Understanding herniated discs and why they are so difficult to heal
Before exploring how peptides might help, you need to understand what you are actually dealing with. A herniated disc is not a simple muscle strain. It is a structural failure of one of the most complex and poorly vascularized tissues in the human body, and that lack of blood supply is precisely what makes disc injuries so stubbornly resistant to healing.
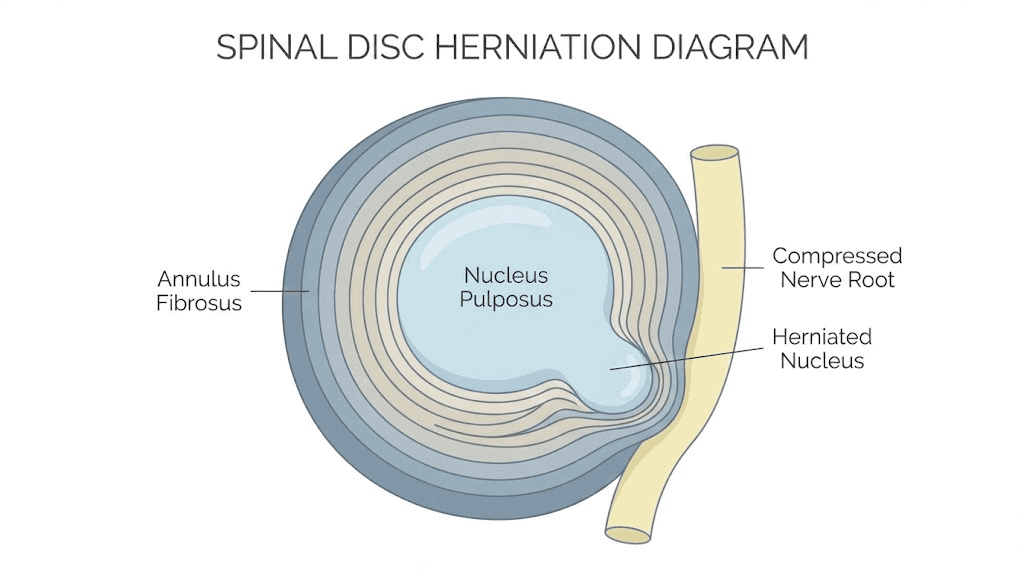
The anatomy of a spinal disc
Each intervertebral disc consists of two main components. The annulus fibrosus forms the outer ring, a complex series of fibrous layers made primarily of type I collagen arranged in alternating diagonal patterns. Think of it like a radial tire, with layers of tough fibers crisscrossing each other for maximum strength. Inside that outer ring sits the nucleus pulposus, a gelatinous core rich in type II collagen, elastin fibers, and a hydrated proteoglycan gel that gives the disc its shock-absorbing properties.
The disc sits between vertebrae, creating the space through which spinal nerves exit. It absorbs compressive forces, allows spinal movement, and distributes mechanical loads across the spine. When functioning properly, it is an engineering marvel.
When it fails, the consequences can be severe.
What actually happens during a herniation
A herniated disc occurs when the nucleus pulposus pushes through a tear or weakness in the annulus fibrosus. This displaced material can compress adjacent nerve roots, triggering pain, numbness, tingling, or weakness in the areas those nerves serve. The severity depends entirely on which nerve gets compressed and how much pressure it is under.
At the L4-L5 level, compression of the L5 nerve root sends pain radiating into the buttock, lateral thigh, lateral calf, and the top of the foot. You might notice weakness in foot dorsiflexion, the ability to pull your toes upward. At L5-S1, the S1 nerve root compression follows a different path, running from the lower back or buttock down the back of the thigh into the calf and heel. People with S1 compression often notice they cannot push off with their toes when walking, or they struggle to rise onto tiptoes on the affected side.
Cervical herniations, though less common, create their own constellation of symptoms. The C5-C6 and C6-C7 levels are most frequently affected, potentially causing arm pain, hand numbness, and grip weakness.
The blood supply problem
Here is the fundamental challenge. Intervertebral discs are the largest avascular structures in the human body. After adolescence, the blood vessels that once supplied nutrients to the disc largely disappear. The disc relies on diffusion, a slow process where nutrients seep in from surrounding tissues through the endplates. This severely limited nutrient supply explains why disc injuries heal so poorly compared to muscle tears or even bone fractures.
Muscles heal in weeks because they have abundant blood supply delivering oxygen, nutrients, and growth factors directly to the injury site. Bones heal in 6 to 8 weeks for the same reason. But discs? They can take months or years, and complete structural restoration is rare with conservative treatment alone.
This is exactly where peptide research becomes relevant. Several peptides being studied have mechanisms that directly address this core problem: they promote new blood vessel formation (angiogenesis), reduce the inflammatory cascade that accelerates disc breakdown, and stimulate the cellular repair processes needed to rebuild damaged disc structures. Understanding these mechanisms is critical before evaluating specific protocols.
The peptides being studied for disc repair
Not all peptides are relevant to herniated disc recovery. The ones generating the most research interest share specific properties: they modulate inflammation, promote tissue regeneration, stimulate collagen synthesis, or support nerve healing. Here are the primary candidates and what the evidence shows for each.
BPC-157: the most studied peptide for disc-related injuries
BPC-157 (Body Protective Compound 157) is a 15-amino-acid peptide derived from a protein found in human gastric juice. It has accumulated the most preclinical evidence among peptides studied for musculoskeletal repair, including data relevant to spinal disc injuries. The peptide has a short half-life of less than 30 minutes and is rapidly metabolized, which means consistent dosing protocols matter significantly.
The mechanisms through which BPC-157 may support disc healing are multiple and interconnected. First, it enhances nitric oxide production, which relaxes blood vessels and improves local circulation. For an avascular structure like a disc, even modest improvements in surrounding blood flow could meaningfully increase nutrient delivery. Second, it stimulates vascular endothelial growth factor (VEGF), promoting the formation of new blood vessels around damaged tissue. Third, and perhaps most relevant, it promotes fibroblast migration and collagen synthesis, the exact cellular processes needed to rebuild the damaged annulus fibrosus.
Research has also shown BPC-157 may alter DNA expression patterns in ways that encourage vascular healing and regeneration. In rat studies, BPC-157 applied immediately after sciatic nerve injury significantly improved the healing process, accelerating axonal regeneration, increasing motor action potentials, and improving functional recovery.
Another rat study examining spinal cord injury found that BPC-157-treated animals showed consistent clinical improvement, including better motor function and earlier resolution of spasticity. Microscopically, the treated animals retained more axons and showed less white matter damage.
Direct disc research, while limited, is emerging. In rats with experimentally induced disc lesions, locally applied BPC-157 increased collagen and blood vessel growth, accelerated healing, and reduced inflammation. BPC-157 also restored nucleus pulposus cells damaged by inflammation, maintained protective proteins, and improved cell survival. Herniated discs treated with BPC-157 showed reduced compression on nerves and faster resolution of neurological symptoms compared to control groups.
For those interested in the broader applications of this peptide, our complete BPC-157 guide covers the full range of research. And if you are evaluating dosing specifics, the BPC-157 5mg dosing guide provides detailed calculations.
TB-500: the systemic tissue repair peptide
TB-500 is a synthetic version of thymosin beta-4, a 43-amino-acid peptide found throughout human tissues. While BPC-157 tends to act more locally near the injection site, TB-500 functions systemically. It circulates through the body, supporting tissue repair wherever damage exists. This systemic action makes it particularly interesting for disc herniations, where the injury site is difficult to access directly.
TB-500 works by regulating cell growth, migration, and attachment, all critical processes for wound healing. It demonstrates significant anti-inflammatory properties through reduction of pro-inflammatory cytokines including TNF-alpha, IL-1 beta, and IL-6. It also suppresses NF-kB activation and modulates macrophage polarization toward an M2 anti-inflammatory phenotype. In simpler terms, it shifts the immune response from tissue destruction toward tissue repair.
When applied around a herniated disc, TB-500 appears to help seal tears in the outer annulus, preventing further disc material from leaking out. It reduces local inflammation, allowing compressed nerves to begin recovering, and promotes new blood vessel formation to improve the circulation and nutrition that discs desperately need for healing.
A study on spinal cord injury in rats found that thymosin beta-4 treatment markedly improved behavioral assessments when administered within days of injury. The numbers of surviving neurons and oligodendrocytes were significantly increased in treated animals compared to controls. This neuroprotective effect is especially relevant for disc herniations where nerve compression is the primary source of symptoms.
The TB-500 benefits guide covers the full spectrum of research applications. For those who have used BPC-157 before and are considering adding TB-500, our BPC-157 vs TB-500 comparison breaks down exactly when each peptide might be more appropriate.
GHK-Cu: the collagen and extracellular matrix rebuilder
GHK-Cu (glycyl-L-histidyl-L-lysine copper complex) is a naturally occurring tripeptide that declines significantly with age. Plasma levels drop from approximately 200 ng/ml at age 20 to around 80 ng/ml by age 60. This decline correlates with decreased healing capacity and reduced tissue regeneration throughout the body.
What makes GHK-Cu particularly relevant for disc repair is its powerful effect on the extracellular matrix, the structural scaffolding that gives tissues their form and function. GHK-Cu stimulates synthesis of type I collagen (structural support), type III collagen (tissue flexibility and repair), glycosaminoglycans, chondroitin sulfate, dermatan sulfate, and the small proteoglycan decorin. Research indicates it can increase collagen production by up to 70% in laboratory studies. The copper component serves as an essential cofactor for lysyl oxidase and lysyl hydroxylase, enzymes critical for proper collagen cross-linking and stability.
For disc repair specifically, GHK-Cu enhances collagen synthesis by chondrocytes, the very cells responsible for maintaining disc structure. It also modulates the activity of metalloproteinases (enzymes that break down extracellular matrix proteins) and their inhibitors, creating a balanced environment where damaged tissue is cleared while new tissue is being built. This dual function, removing scar tissue while replacing it with healthy tissue, is exactly what a damaged disc needs.
GHK-Cu also downregulates pro-inflammatory cytokines like TNF-alpha and IL-6, reduces levels of fibrinogen (involved in inflammation), and blocks NF-kB and p38 MAPK activation. These anti-inflammatory effects help create the conditions necessary for tissue repair rather than continued degradation.
For detailed dosing information, refer to our GHK-Cu dosage guide. Those specifically interested in injection protocols can review the GHK-Cu injection guide.
MOTS-c: the mitochondrial peptide for disc cell survival
MOTS-c is a 16-amino-acid peptide encoded by the mitochondrial genome that has recently emerged as a promising candidate for intervertebral disc degeneration. Disc degeneration is characterized by oxidative-stress-driven apoptosis (cell death) and senescence (cell aging) of nucleus pulposus mesenchymal stem cells. MOTS-c directly addresses these mechanisms.
In a rat model of intervertebral disc degeneration, MOTS-c injection preserved disc height (82.4% versus 58.7% in the untreated group), restored MRI signals indicating improved disc hydration, and reduced histological degeneration scores by 44% compared to untreated controls. These are meaningful numbers that suggest real structural preservation, not just symptom management.
Our MOTS-c benefits guide covers the broader applications of this peptide, and the MOTS-c dosage chart provides specific protocol information. Understanding the potential side effects of MOTS-c is equally important before considering its use.
Other peptides under investigation
Several additional peptides are being studied for disc-related applications, though with less established evidence:
Vasoactive Intestinal Peptide (VIP) has demonstrated the ability to slow disc degeneration progression and improve aggrecan levels in mouse studies. Aggrecan is a critical proteoglycan for maintaining disc hydration and shock-absorbing capacity. However, researchers acknowledge they are far from developing a clinical application.
SB-01 is a synthetic 7-amino-acid peptide in clinical trials that downregulates TGF-beta-1, a growth factor highly expressed in degenerated discs. Abnormal TGF-beta-1 signaling degrades the extracellular matrix and stimulates nerve growth factor, potentially increasing pain. Intradiscal injection of SB-01 represents a first-in-class approach to treating chronic discogenic back pain.
Link-N peptide has shown promise as a cost-efficient therapy for retarding the degenerative process in early-stage disc disease. It targets the disc extracellular matrix directly and may help maintain structural integrity before significant herniation occurs.
Collagen peptides taken orally also deserve mention. While they do not directly target the disc the way injectable peptides might, hydrolyzed collagen peptides provide the raw amino acids, particularly glycine and proline, that the body needs for connective tissue synthesis. Research suggests 5 to 10 grams daily of supplemental glycine (achievable through collagen peptides or bone broth) can help cover the shortfall in modern diets.
The BPC-157 and TB-500 combination: why researchers stack them for disc injuries
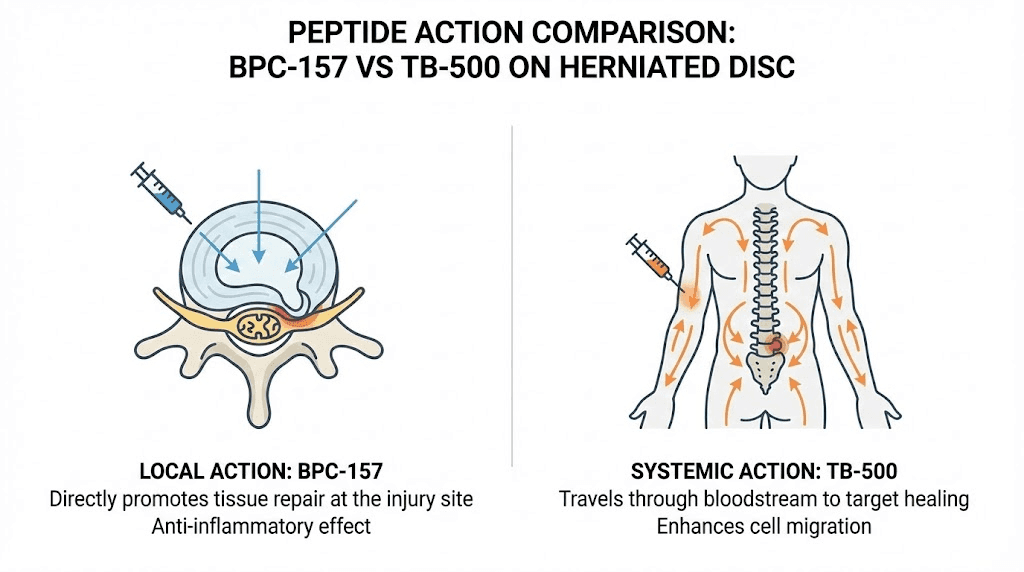
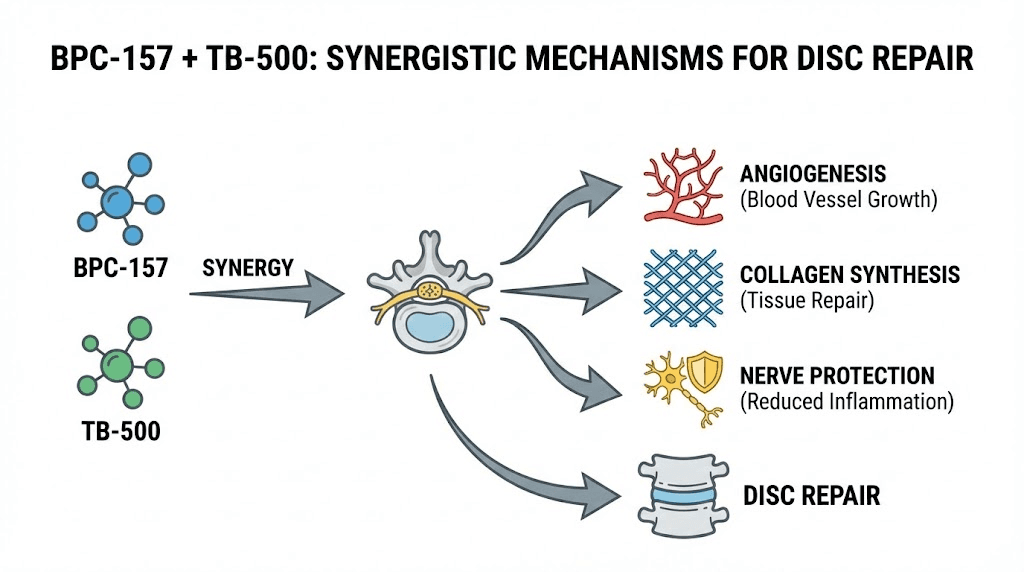
While each peptide shows meaningful effects individually, the combination of BPC-157 and TB-500 has generated particular interest among researchers studying connective tissue repair. The rationale is straightforward: these peptides work through complementary mechanisms, and together they may address more aspects of disc healing than either can alone.
BPC-157 excels at local tissue protection and repair. It concentrates its effects near the administration site, promoting collagen synthesis, reducing local inflammation, and stimulating growth factors directly in damaged tissue. TB-500, by contrast, works systemically. It improves overall circulation to injured areas, promotes cell migration from distant locations, and reduces systemic inflammation that can perpetuate the injury cycle.
When combined, they form what researchers describe as a synergistic healing strategy. BPC-157 handles the structural integrity of the target tissue while TB-500 improves the vascularity and cellular recruitment needed to support that repair. The combination activates cellular regeneration through multiple pathways simultaneously, exceeding what either compound achieves individually.
Our detailed BPC-157 and TB-500 stacking guide covers the specifics of combining these peptides. Understanding proper peptide reconstitution is essential before beginning any protocol, and our bacteriostatic water guide explains the preparation process in detail.
Why the combination matters for disc injuries specifically
Consider the specific challenges of disc repair:
The disc lacks blood supply. TB-500 promotes angiogenesis systemically, potentially creating new microvascular networks in the tissue surrounding the disc. Meanwhile, BPC-157 stimulates VEGF locally, encouraging blood vessel formation right where it is needed most.
The annulus fibrosus needs collagen repair. BPC-157 directly stimulates fibroblast migration and collagen synthesis at the injury site. GHK-Cu, if added to the stack, further enhances this process through its effects on multiple types of collagen and extracellular matrix components.
Nerve compression causes the symptoms. Both BPC-157 and TB-500 demonstrate neuroprotective effects. BPC-157 accelerates axonal regeneration, while TB-500 supports neuronal survival and reduces neuroinflammation. Together, they may help compressed nerves recover more quickly even as the disc itself heals.
Inflammation perpetuates the cycle. Both peptides reduce pro-inflammatory cytokines, but through different pathways. This multi-pathway anti-inflammatory approach may be more effective than either peptide alone at breaking the inflammation-degeneration cycle that characterizes chronic disc injuries.
For those interested in exploring peptide stacking strategies more broadly, our comprehensive guide covers the principles that apply across different combinations. And understanding how many peptides you can take simultaneously helps prevent overcomplicated protocols.
Research-backed protocols for herniated disc recovery
Understanding which peptides might help is only half the equation. The other half is knowing how to use them properly. Dosing too low produces no effect. Dosing too high wastes material and increases risk. Timing matters. Administration route matters. Duration matters. Here are the protocols supported by current research and clinical observations.
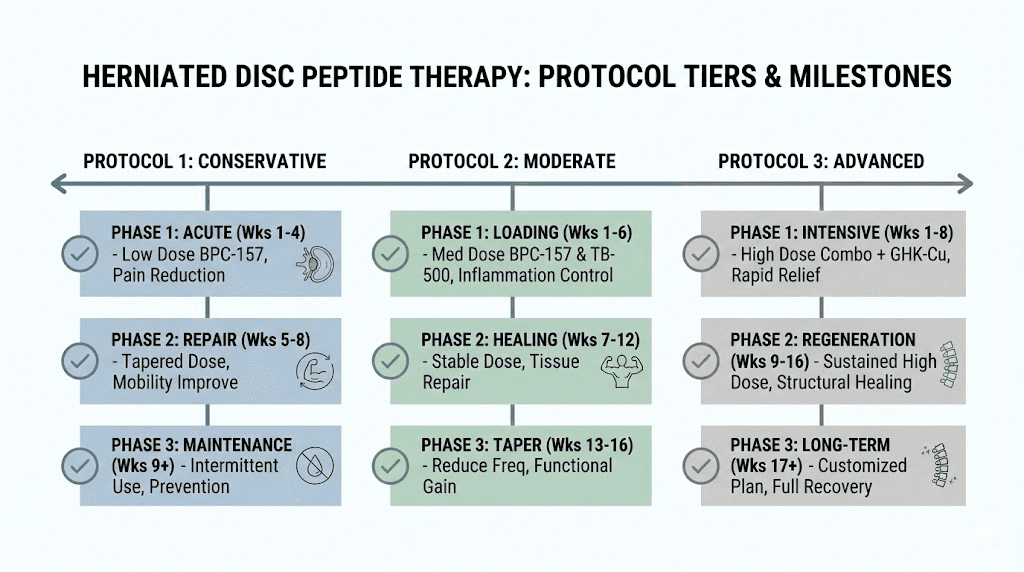
Protocol 1: BPC-157 focused approach (mild to moderate herniations)
Goal: Reduce inflammation, promote disc tissue repair, and support nerve recovery for herniations causing moderate pain and functional limitation.
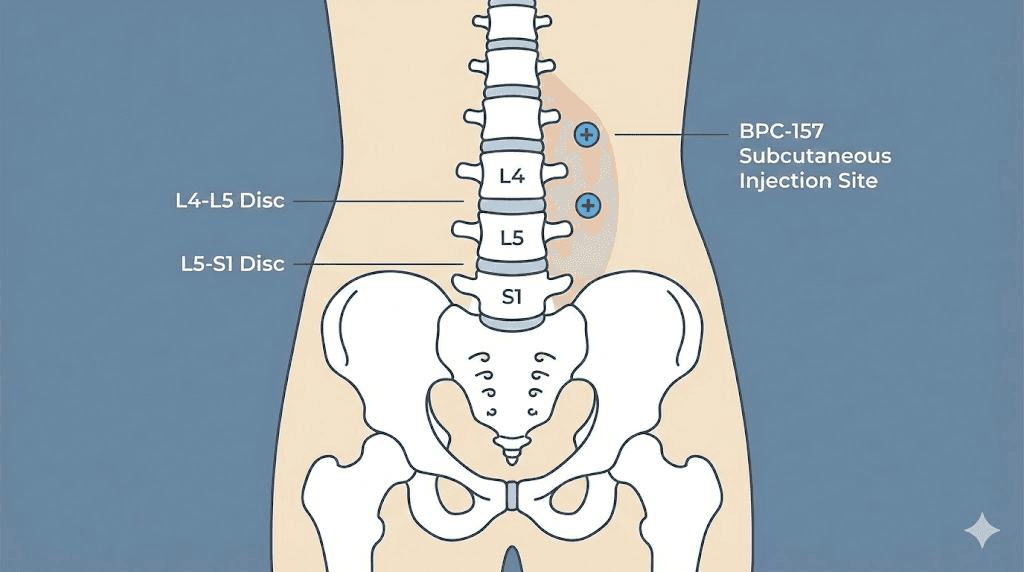
Dosage: 200 to 300 mcg administered subcutaneously twice daily (morning and evening). Research shows efficacy at ranges from 1 to 10 mcg per kg body weight. For a 80 kg person, this translates to 80 to 800 mcg per day. Most protocols target the middle of this range.
Administration site: Subcutaneous injection as close to the affected spinal segment as practical. For lumbar herniations, this typically means injecting in the lower back area on either side of the spine. The goal is to get the peptide as close to the target tissue as possible, since BPC-157 acts primarily locally.
Duration: 4 to 6 weeks for an initial course. Some researchers extend to 8 weeks for more severe cases.
Expected timeline:
Week 1 to 2: Initial reduction in inflammation and pain
Week 2 to 4: Meaningful improvement in nerve-related symptoms (reduced radiating pain, improved sensation)
Week 4 to 6: Continued structural healing, further functional improvement
Post-protocol: Maximum benefits from a single course typically manifest by week 8 to 12 as tissue remodeling continues
Use the SeekPeptides peptide calculator to determine exact dosing based on your vial concentration and desired dose. Proper reconstitution technique is essential for accurate dosing. Our guide on how much bacteriostatic water to add walks through the calculations step by step.
Protocol 2: BPC-157 plus TB-500 combination (moderate to severe herniations)
Goal: Comprehensive disc repair combining local tissue protection with systemic healing support for more significant herniations or cases that have not responded to single-peptide approaches.
BPC-157 dosage: 250 to 300 mcg subcutaneously twice daily near the affected disc level.
TB-500 dosage: Initial loading phase of 4 to 8 mg per week for the first 4 to 6 weeks, typically split into 2 to 3 injections per week. Followed by a maintenance phase of 2 to 4 mg per week for an additional 2 to 4 weeks.
TB-500 administration: Subcutaneous injection. Unlike BPC-157, injection site for TB-500 is less critical since it acts systemically. Abdominal subcutaneous injection is commonly used for convenience.
Duration: 6 to 8 weeks total. The loading phase is critical for establishing circulating levels of TB-500.
Expected timeline:
Week 1 to 3: Reduction in inflammation, improved mobility, some pain relief
Week 3 to 6: Significant improvement in nerve symptoms, increased functional capacity
Week 6 to 12: Continued tissue remodeling, disc structural improvements
Month 3 to 6: Full benefits of the protocol become apparent as remodeled tissue matures
Understanding proper peptide storage is critical during multi-week protocols. Reconstituted peptides have limited shelf life, and our guide on how long reconstituted peptides last in the fridge helps you plan accordingly. For powder storage, see our guide on peptide powder shelf life.
Protocol 3: comprehensive stack (severe or chronic herniations)
Goal: Maximum regenerative support for severe herniations, chronic disc degeneration, or cases being managed alongside other treatments to avoid surgery.
BPC-157: 250 to 300 mcg subcutaneously twice daily near the affected level.
TB-500: 5 mg per week split into 2 to 3 doses for 6 weeks, then 2 to 3 mg per week for 4 weeks maintenance.
GHK-Cu: Added for its extracellular matrix rebuilding properties. Typical research dosing for GHK-Cu is outlined in our dosage chart. The peptide can be administered subcutaneously, with some researchers using it in the same protocol alongside BPC-157 and TB-500.
Oral collagen peptides: 10 to 15 grams daily to provide raw materials for connective tissue repair.
Duration: 8 to 12 weeks for the injectable components, with oral collagen continued long-term.
This is an advanced protocol that requires careful planning. Our guide on cycling different peptides explains how to structure multi-peptide approaches. The peptide cycle planning guide provides the framework for designing your own protocol timeline.
Administration and practical considerations
Getting the protocol right on paper is one thing. Executing it properly is another entirely. Small errors in preparation, storage, or administration can undermine an otherwise well-designed protocol. Here are the practical details that matter.
Reconstitution and preparation
Both BPC-157 and TB-500 come as lyophilized (freeze-dried) powders that must be reconstituted with bacteriostatic water before use. This is not a complicated process, but it requires precision. Using sterile technique is non-negotiable. Contaminating a vial introduces bacteria that will degrade the peptide and potentially cause infection.
The step-by-step mixing guide walks through the entire process. Key points include: use an alcohol swab on the vial stopper before each draw, inject bacteriostatic water slowly down the side of the vial (never directly onto the powder), and gently swirl rather than shake to dissolve. Our peptide reconstitution calculator handles the math, so you know exactly how much water to add for your desired concentration.
Once reconstituted, peptides must be refrigerated. Not frozen. Not left at room temperature. Refrigerated at 2 to 8 degrees Celsius (36 to 46 degrees Fahrenheit). Our guide on post-reconstitution storage covers the specifics. Most reconstituted peptides maintain potency for 3 to 4 weeks when stored properly, though some researchers report usable potency for up to 6 weeks. Understanding room temperature stability matters for those who travel or have storage challenges.
Injection technique for spinal applications
For lumbar disc herniations, subcutaneous injection in the lower back region is the standard research approach for self-administered protocols. This is distinct from intradiscal injection, which requires fluoroscopy or ultrasound guidance and must be performed by a qualified medical professional.
Subcutaneous injection means the peptide goes into the fat layer just beneath the skin, not into muscle. Using an insulin syringe with a short (8mm or less) needle is typical. The injection site should be cleaned with an alcohol swab, the skin pinched to create a fold, and the needle inserted at a 45-degree angle. Rotate injection sites to prevent tissue irritation from repeated injections in the same spot.
For those new to peptide injections, our complete injection guide covers everything from needle selection to proper technique. The peptide injection pen guide reviews options for those who prefer pen-style delivery systems. And for those who want to understand the broader landscape of administration routes, our comparison of oral peptide capsules versus injections explains why most researchers prefer injection for disc-related protocols.
Injection site considerations for different disc levels
Where you inject BPC-157 matters because of its primarily local action. For lumbar herniations (L4-L5 or L5-S1), inject subcutaneously in the lower back, approximately 1 to 2 inches lateral to the spine at the affected level. For cervical herniations (less common but possible), the injection would be in the posterior neck region, though cervical protocols should always involve medical supervision.
TB-500 does not require proximity to the injury because it works systemically. Standard subcutaneous injection in the abdominal area is sufficient. GHK-Cu can be administered near the affected area similar to BPC-157, though some researchers rotate between local and systemic injection sites.
What to expect during a protocol
Mild soreness at the injection site is the most common experience, typically resolving within minutes to hours. Fewer than 5% of people report temporary numbness or tingling from the injection itself (distinct from herniation symptoms). Serious adverse effects are very rare in published literature.
However, it is critical to understand that these peptides are not FDA-approved for any indication. In fact, the FDA designated BPC-157 as a Category 2 bulk drug substance, meaning it cannot be compounded by commercial pharmaceutical companies due to insufficient safety evidence in humans. Despite this, BPC-157 products continue to be sold as research chemicals or dietary supplements, which are not subject to FDA regulatory oversight. Our guide on peptide safety and risks provides essential context.
Understanding the current legal status of peptides is also important. While possession is not illegal (they are not DEA-scheduled substances), the regulatory landscape continues to evolve. Our peptide regulation news article tracks the latest developments.
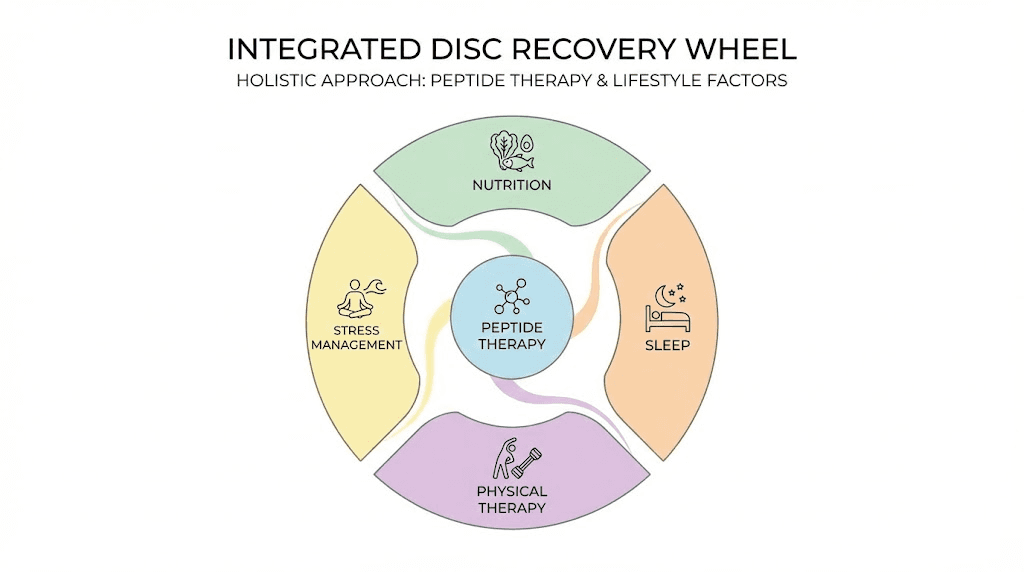
Supporting your disc recovery beyond peptides
Peptides are not standalone treatments. They are tools that may enhance the body natural healing processes. But those processes need the right environment to function optimally. Nutrition, movement, sleep, and stress management all play critical roles in disc recovery, and neglecting them can undermine even the most well-designed peptide protocol.
Nutritional support for disc healing
The intervertebral disc is made primarily of collagen and proteoglycans. To rebuild these structures, the body needs adequate raw materials.
Collagen and glycine: The modern diet is chronically deficient in glycine, an amino acid essential for collagen synthesis. Research suggests supplementing with 5 to 10 grams daily through collagen peptide supplements, bone broth, or pure glycine powder. Hydrolyzed collagen peptides have the advantage of high bioavailability and targeted amino acid profiles for connective tissue repair.
Vitamin C: Essential cofactor for collagen synthesis. Without adequate vitamin C, collagen cross-linking is impaired regardless of how much raw material is available. Combining vitamin C with peptide protocols is a strategy many researchers employ to maximize connective tissue repair.
Omega-3 fatty acids: Reduce systemic inflammation through multiple pathways. For disc herniations where inflammation drives both pain and degeneration, omega-3s provide baseline anti-inflammatory support that complements the anti-inflammatory effects of peptides.
Glucosamine and chondroitin: These are the building blocks of proteoglycans that give the disc its hydrated, shock-absorbing properties. Supplementation may support the repair processes that peptides are stimulating at the cellular level.
Magnesium: Involved in over 300 enzymatic reactions, including collagen synthesis and muscle relaxation. Deficiency is common and can exacerbate muscle spasm and pain around a herniated disc.
Movement and physical therapy
Complete rest is not the answer for most disc herniations. While acute severe symptoms may require short periods of reduced activity, prolonged rest actually slows healing and leads to deconditioning that makes recurrence more likely.
Isometric core exercises strengthen the muscles that support and stabilize the spine without imposing excessive load on the disc. McKenzie extension exercises have evidence supporting their use for posterior disc herniations. Walking, particularly at a comfortable pace, promotes disc nutrition through the pumping action that drives fluid exchange.
Avoid lumbar hyperextension exercises, heavy axial loading (squats, deadlifts) during the acute phase, and any movement that reproduces radiating symptoms. The goal is to maintain activity within pain-free ranges while the disc heals.
Peptides may support faster recovery from physical therapy sessions by reducing inflammation and promoting tissue repair between sessions. This is an area where the BPC-157 and TB-500 combination may be particularly useful, as the injury recovery peptide guide discusses in detail.
Sleep and recovery
Growth hormone release peaks during deep sleep, and growth hormone is a critical driver of tissue repair throughout the body. Poor sleep quality directly impairs healing. For disc herniation recovery, optimizing sleep is not optional, it is fundamental.
Sleeping position matters too. Side sleeping with a pillow between the knees reduces torsional stress on the lumbar spine. Sleeping on the back with a pillow under the knees maintains the natural lumbar curve. Stomach sleeping is generally the worst position for disc herniations and should be avoided.
Some researchers have explored peptides that support sleep quality, such as DSIP (delta sleep-inducing peptide) and pineal peptides. While these are not disc-specific, optimizing sleep quality can enhance the overall recovery environment. The DSIP dosage guide covers protocols for those interested.
What the research actually shows: an honest assessment
It would be irresponsible to present peptide therapy for herniated discs without being transparent about the current state of evidence. Here is what we know, what we do not know, and where the gaps are.
What the evidence supports
BPC-157 has demonstrated tissue-protective, anti-inflammatory, and regenerative effects across multiple animal studies. Specific to spinal applications, it has shown benefits in sciatic nerve repair, spinal cord injury recovery, and preliminary disc lesion models. The mechanisms are well-characterized: angiogenesis, collagen synthesis, inflammation reduction, and neuroprotection.
TB-500 has demonstrated neuroprotective effects in spinal cord injury models, with treated animals showing significantly more neuronal and oligodendrocyte survival. Its systemic anti-inflammatory and cell migration properties are well-established in the literature.
GHK-Cu is the most well-characterized of the three in terms of extracellular matrix effects. Its ability to stimulate collagen synthesis, glycosaminoglycan production, and balanced tissue remodeling is supported by multiple studies. The age-related decline in natural GHK-Cu levels provides a logical rationale for supplementation.
MOTS-c has the most direct disc-specific evidence, with rat studies showing preserved disc height and reduced degeneration scores. The 44% reduction in histological degeneration scores is a clinically meaningful finding.
What the evidence does not yet support
Here is where honesty matters most.
There are no large-scale, randomized, double-blind, placebo-controlled human clinical trials of BPC-157, TB-500, or GHK-Cu specifically for herniated disc repair. The closest we have are animal studies, small case series, and clinical observations from practitioners who incorporate peptides into multimodal treatment plans.
The claim that "over 75% of patients achieve significant pain relief without surgery" with peptide therapy comes from clinical observations, not controlled trials. Without proper controls, it is impossible to separate the peptide effect from natural healing (remembering that 85% of acute herniations resolve on their own), placebo effects, concurrent treatments, and time.
Dosing protocols for disc herniations are extrapolated from studies on other tissues and from clinical experience. Optimal doses specifically for disc repair have not been established through dose-finding studies.
Long-term safety data from human use is limited. While the preclinical safety profile appears favorable (few adverse effects reported in animal studies), this does not guarantee the same in humans, especially with prolonged use.
The honest takeaway
Peptides for herniated disc recovery represent a promising but early-stage area of research. The mechanisms are biologically plausible. The animal data is encouraging. Clinical observations from practitioners are positive. But robust human clinical evidence specifically for disc herniations is still developing.
This does not mean peptides do not work for disc injuries. It means the evidence is not yet strong enough to make definitive claims. Any researcher considering peptides for a disc herniation should do so with informed expectations, ideally under the guidance of a knowledgeable healthcare provider, and as part of a comprehensive recovery plan that includes proven interventions like physical therapy and lifestyle optimization.
SeekPeptides members get access to the latest research updates, detailed protocol guides, and a community of experienced researchers who share real-world outcomes from their protocols. This kind of peer-to-peer knowledge is especially valuable in a field where controlled trial data is limited.
Comparing peptides to conventional treatments for herniated discs
To put peptide therapy in perspective, it helps to understand how it compares with the treatments most commonly used for disc herniations. Each approach has strengths and limitations. The question is not which is "best" in the abstract, but which combinations make the most sense for a given situation.
NSAIDs and oral medications
Non-steroidal anti-inflammatory drugs (ibuprofen, naproxen, diclofenac) are the first-line treatment for herniation-related pain. They reduce inflammation and provide analgesic effects. However, they work only while you take them, do nothing to promote tissue repair, and carry risks of gastrointestinal, cardiovascular, and renal side effects with prolonged use.
Muscle relaxants address the spasm component but do not treat the underlying disc pathology. Oral corticosteroids (prednisone) provide short-term anti-inflammatory benefit but have significant side effect profiles with repeated courses, including bone density loss, immune suppression, and metabolic disruption.
Peptides, by contrast, aim to reduce inflammation while simultaneously promoting tissue repair. They do not merely mask symptoms. They attempt to address the underlying structural damage. This fundamental difference in mechanism is why peptides have generated such interest despite the limitations of current evidence.
Epidural steroid injections
Epidural steroid injections deliver corticosteroids directly to the area around the compressed nerve root. They can provide significant short-term pain relief (weeks to months) and are useful as a bridge while the disc heals naturally. However, they do not repair disc tissue, benefits are temporary, and repeated injections carry risks including nerve damage, infection, and further weakening of surrounding tissues.
Some practitioners are now combining epidural steroid injections with peptide therapy, using the steroid to provide immediate symptom relief while the peptides work on tissue repair over weeks to months. This multimodal approach leverages the strengths of each intervention while mitigating their individual limitations.
Physical therapy
Physical therapy is the gold standard of conservative treatment and has the strongest evidence base. It strengthens supporting muscles, improves spinal mechanics, and creates the movement patterns that promote disc health long-term. The limitation is that physical therapy cannot directly stimulate the cellular repair processes within the disc itself.
Peptides and physical therapy may be particularly complementary. The peptides support cellular repair and reduce inflammation, while physical therapy provides the mechanical loading that drives nutrient diffusion into the disc and strengthens the muscular support system. Several practitioners report that patients using peptides alongside physical therapy progress faster than those doing physical therapy alone, though this observation awaits controlled study.
Surgery
Surgical options include microdiscectomy (removal of the herniated disc material), laminectomy (removal of bone to relieve pressure), and spinal fusion (permanently joining two or more vertebrae). Surgery is generally reserved for cases with progressive neurological deficits, cauda equina syndrome (a surgical emergency), or persistent symptoms despite 6 to 12 months of conservative treatment.
Surgery success rates are generally good for pain relief (70 to 90% improvement in leg pain symptoms), but come with risks: infection, nerve damage, disc reherniation (5 to 15% recurrence rate after microdiscectomy), and adjacent segment disease with fusion (20 to 30% develop problems within 10 years). Once disc material is removed, it does not regenerate.
Peptide therapy is being explored by some researchers as a potential alternative to surgery for cases that have not responded to other conservative treatments but do not have absolute surgical indications. It is also being investigated as a post-surgical adjunct to support healing and reduce reherniation risk. These are logical applications given the mechanisms involved, but both require further study.
Treatment | Pain relief timeline | Tissue repair | Duration of benefit | Risk profile |
|---|---|---|---|---|
NSAIDs | Hours to days | None | While taking only | GI, cardiovascular, renal |
Epidural steroids | Days to weeks | None | Weeks to months | Moderate |
Physical therapy | Weeks to months | Indirect | Long-term with maintenance | Very low |
Peptide therapy | 1 to 4 weeks | Direct (in research) | Potentially lasting | Low (limited data) |
Microdiscectomy | Days to weeks | None (removes tissue) | Long-term for most | Surgical risks |
Spinal fusion | Months | None | Permanent (with trade-offs) | Significant |
For additional perspective on how peptides compare with other treatment modalities, our guide on peptides versus TRT provides a framework for thinking about peptide therapy in the broader context of regenerative medicine. Understanding the difference between peptides and steroids is also important, as many people conflate the two.
Common mistakes researchers make with disc-related peptide protocols
After reviewing thousands of discussions about peptide use for spinal injuries, certain mistakes come up repeatedly. Avoiding these common errors can mean the difference between a successful protocol and a disappointing one.
Mistake 1: injecting too far from the affected disc
BPC-157 acts primarily locally. Injecting it in the abdomen for a lumbar disc herniation significantly reduces its concentration at the target tissue. The peptide needs to be administered as close to the affected level as practically possible for maximum effect. While some systemic absorption occurs with any subcutaneous injection, proximity to the target matters for BPC-157.
Mistake 2: stopping the protocol too early
Disc tissue heals slowly, much slower than muscle or even bone. A 2-week course of BPC-157 may reduce inflammation and provide some pain relief, but it is unlikely to produce meaningful structural repair. Most protocols run 4 to 6 weeks minimum, with some extending to 8 to 12 weeks for more severe injuries. Stopping because symptoms improved at week 2 means abandoning the protocol before the structural repair phase has completed.
Mistake 3: using peptides as a standalone treatment
Peptides support healing. They do not replace the need for proper rehabilitation. A researcher who uses BPC-157 and TB-500 but skips physical therapy, eats poorly, sleeps badly, and returns to heavy lifting too soon will likely be disappointed. Peptides work best as part of a comprehensive recovery strategy.
Mistake 4: poor reconstitution and storage
Using tap water instead of bacteriostatic water. Shaking the vial vigorously (denaturing the peptide). Leaving reconstituted peptides at room temperature for hours. Reusing needles. These preparation errors degrade the peptide and can introduce contaminants. Our common peptide mistakes guide covers the full list of errors to avoid.
Mistake 5: unrealistic expectations
Peptides are not going to regrow a completely degenerated disc or reverse decades of spinal wear. They may support the healing of a herniation, reduce inflammation, and promote nerve recovery. Setting expectations appropriately prevents disappointment and ensures you evaluate results objectively. Review our realistic peptide timeline guide for perspective on what to expect and when.
Mistake 6: sourcing low-quality peptides
The peptide market includes products of wildly varying quality. Some contain less peptide than labeled. Some contain degradation products. Some contain contaminants. Third-party testing is the minimum standard for quality assurance. Our peptide testing labs guide explains how to verify what you are using, and the vendor comparison guide reviews sourcing options.
Specific disc levels and peptide considerations
Not all disc herniations are identical, and the specific level affected can influence protocol decisions. Here is what to consider for the most common herniation locations.
L4-L5 herniations
The L4-L5 junction is one of the most mobile segments of the lumbar spine, making it particularly vulnerable to disc herniation. Compression of the L5 nerve root causes pain radiating from the buttock down the lateral leg to the top of the foot, with potential weakness in foot dorsiflexion.
For L4-L5 herniations, BPC-157 injections should target the lower lumbar region approximately at the level of the iliac crest (top of the hip bone), which corresponds roughly to the L4-L5 level. The neuroprotective effects of both BPC-157 and TB-500 are particularly relevant here, as L5 nerve compression can cause foot drop if not addressed.
L5-S1 herniations
The L5-S1 level bears the most mechanical stress in the spine, the transition point where the flexible lumbar spine meets the rigid sacrum. S1 nerve compression causes pain down the back of the leg to the heel, with potential weakness in plantar flexion (pushing off with the toes).
This level often presents the greatest challenge because of the high mechanical loads it endures. Protocols for L5-S1 herniations may benefit from the longer durations (8+ weeks) and the comprehensive stack approach that combines BPC-157 local action with TB-500 systemic support and GHK-Cu extracellular matrix rebuilding.
Cervical herniations
Cervical disc herniations (most commonly C5-C6 and C6-C7) require extra caution due to the proximity of the spinal cord. While peptide protocols are similar in principle, cervical applications should only be pursued under direct medical supervision. The consequences of complications in the cervical spine are more severe than in the lumbar region.
TB-500, with its systemic action, may be particularly useful for cervical herniations since it does not require injection near the sensitive cervical structures. BPC-157 can be administered in the posterior neck region but requires precision and experience.
Multiple level herniations
Some individuals have herniations at more than one level. For multi-level involvement, the systemic effects of TB-500 become even more valuable, as it supports healing throughout the body rather than at a single site. BPC-157 injections can be split between levels if needed, though the total daily dose should remain within standard protocol ranges.
For broader context on how peptides address different types of pain and injury, see our guides on the best peptides for pain, peptides for joint pain, and peptides for tendon repair. Understanding the broader injury recovery landscape helps contextualize disc-specific protocols within the wider research picture.
Monitoring progress and adjusting protocols
Starting a peptide protocol is not a set-and-forget situation. Meaningful disc recovery requires ongoing assessment and willingness to adjust the approach based on response. Here is how experienced researchers track their progress.
Pain tracking
Use a simple 0 to 10 numeric rating scale, recorded at the same time each day (morning and evening are ideal). Track both back pain and radiating pain separately, as they can improve at different rates. A downward trend over weeks is more meaningful than day-to-day fluctuations.
Functional milestones
Functional improvements often tell you more than pain scores alone:
Walking distance without symptom increase
Sitting tolerance (minutes before symptoms worsen)
Ability to perform previously limited activities
Sleep quality (reduced nighttime symptoms indicate improvement)
Medication usage (decreasing NSAID use is a positive sign)
When to adjust the protocol
If there is no improvement after 3 to 4 weeks on a BPC-157 only protocol, consider adding TB-500 for systemic support. If a BPC-157 plus TB-500 combination is not producing results after 4 to 6 weeks, the comprehensive stack with GHK-Cu may be worth exploring. If no protocol produces meaningful improvement, it is time for medical reassessment, as the herniation may require a different intervention entirely.
Worsening symptoms, new weakness, or changes in bowel or bladder function require immediate medical attention regardless of any peptide protocol. These can indicate cauda equina syndrome, a surgical emergency.
Post-protocol maintenance
After completing an initial protocol, some researchers use lower-frequency maintenance dosing (BPC-157 once daily or every other day, TB-500 once weekly) for an additional 4 to 6 weeks. Others cycle off completely and reassess before deciding whether additional courses are needed. Our peptide dosing guide covers maintenance strategies in detail.
Long-term disc health requires ongoing attention to the factors that caused or contributed to the herniation in the first place. Core strengthening, proper lifting mechanics, maintaining healthy body weight, staying active, and avoiding prolonged sitting all reduce the risk of recurrence. Peptides may give the disc a healing boost, but lifestyle factors determine whether that healing is maintained.
Cost considerations and practical planning
Peptide protocols for disc herniations are not covered by insurance, and costs can add up over multi-week protocols. Understanding the financial commitment upfront helps with planning and prevents interrupted protocols due to budget constraints.
BPC-157 at research-grade quality typically runs between $30 to $60 per 5mg vial. At 250 mcg twice daily, a single vial lasts approximately 10 days. A 6-week protocol requires roughly 4 to 5 vials.
TB-500 is typically priced at $40 to $80 per 5mg vial. At loading doses of 5 mg per week, one vial lasts one week. A 6-week loading phase plus 4-week maintenance phase requires approximately 8 to 10 vials.
Our peptide cost guide provides current pricing data, and the peptide cost calculator helps estimate total protocol costs based on your specific dosing plan. Understanding cost helps you plan complete protocols rather than cutting them short due to unexpected expenses. The peptide therapy cost guide provides a broader perspective on what to budget for comprehensive peptide research.
Who should not use peptides for disc herniations
Peptide therapy is not appropriate for everyone, and certain situations require alternative approaches or additional medical oversight.
Cauda equina syndrome: If you experience sudden onset of bowel or bladder dysfunction, bilateral leg weakness, or saddle anesthesia (numbness in the groin and inner thighs), this is a surgical emergency. No peptide protocol is appropriate. Seek immediate emergency medical care.
Progressive neurological deficits: If weakness is worsening despite treatment, medical evaluation is essential. Peptides may support recovery after the acute threat is addressed, but they should not delay necessary surgical intervention.
Active infections: Peptide therapy during active infections is not recommended, as the immune-modulating effects could theoretically interfere with the body response to the infection.
Cancer history: Some peptides promote cell growth and angiogenesis. While there is no direct evidence that BPC-157 or TB-500 promote cancer growth, individuals with active cancer or recent cancer history should discuss any peptide use with their oncologist.
Pregnancy and breastfeeding: There is insufficient safety data for peptide use during pregnancy or lactation. These populations should avoid peptide therapy until more data is available.
Children and adolescents: The safety profile of these peptides in developing bodies has not been established.
For a comprehensive understanding of safety considerations, our peptide safety and risks guide covers contraindications, interactions, and monitoring recommendations in detail. The getting started with peptides guide provides a structured introduction for those new to peptide research.
The future of peptide therapy for disc repair
The field of peptide therapy for spinal disc repair is evolving rapidly. Several developments suggest we are still in the early chapters of this story.
Injectable peptide hydrogels: Researchers have developed self-assembling peptide hydrogels that can be injected directly into the nucleus pulposus. These hydrogels form a gel with mechanical properties comparable to native disc tissue within seconds to minutes. They essentially provide a structural scaffold while promoting cellular repair. This represents a significant advance over systemic or subcutaneous peptide delivery.
SB-01 clinical trials: The synthetic peptide SB-01, which targets TGF-beta-1 signaling in degenerated discs, is currently in clinical trials. This is one of the first peptide-based therapies for disc disease to reach human clinical trials, and its outcomes will significantly influence the field.
MOTS-c disc research: The direct evidence of MOTS-c preserving disc height and reducing degeneration in animal models positions it as one of the most promising candidates for future clinical development specifically targeting disc disease.
Combination biomaterial approaches: Researchers are exploring peptide-glycosaminoglycan hybrid hydrogels that combine the regenerative properties of peptides with the structural properties of the disc extracellular matrix. These injectable biomaterials could potentially replace the nucleus pulposus while promoting surrounding tissue repair.
Staying current with these developments matters. SeekPeptides tracks the latest peptide research and studies as they are published, providing members with timely updates that help inform protocol decisions.
Frequently asked questions
Can peptides actually heal a herniated disc or just reduce symptoms?
The honest answer is both, potentially. Peptides like BPC-157 and TB-500 have mechanisms that address both symptom reduction (anti-inflammatory effects) and structural repair (collagen synthesis, angiogenesis, extracellular matrix remodeling). Animal studies show actual tissue repair, not just symptom masking. However, human clinical trials specifically for disc herniations are limited, so definitive claims about disc healing in humans cannot yet be made.
How long does it take for peptides to work on a herniated disc?
Most researchers report initial symptom improvement within 1 to 4 weeks, depending on severity and protocol. Structural repair takes significantly longer, typically 2 to 6 months for meaningful tissue remodeling. Our peptide timeline guide provides detailed expectations across different applications. Disc herniations, being in avascular tissue, generally fall on the longer end of the spectrum.
Should I use BPC-157 or TB-500 for a herniated disc?
For mild to moderate herniations, BPC-157 alone may be sufficient due to its strong local tissue repair effects. For more severe cases or when systemic inflammation is significant, combining both provides broader coverage. The BPC-157 vs TB-500 comparison helps determine which approach suits your specific situation. Many researchers find the combination more effective than either peptide alone.
Can I use peptides alongside physical therapy for my herniated disc?
Yes, and many researchers consider this the optimal approach. Physical therapy provides the mechanical loading and strengthening that promotes disc health, while peptides support the cellular repair processes. They address different aspects of recovery and are generally considered complementary rather than conflicting.
Are peptides safe to use for spinal conditions?
BPC-157 and TB-500 have shown favorable safety profiles in preclinical research, with few adverse effects reported. However, they are not FDA-approved for any human therapeutic use, and long-term safety data is limited. Our safety guide provides comprehensive information. Always consult a qualified healthcare provider before starting any peptide protocol, especially for spinal conditions.
Where should I inject BPC-157 for a lumbar herniated disc?
Subcutaneous injection in the lower back, approximately 1 to 2 inches lateral to the spine at the affected level, is the standard research approach. BPC-157 acts primarily locally, so proximity to the injured disc matters. This is different from intradiscal injection, which requires medical guidance and imaging. Our injection guide covers proper subcutaneous technique.
Can peptides help me avoid surgery for a herniated disc?
Some clinical practitioners report that peptide therapy, combined with physical therapy and lifestyle modifications, has helped patients avoid surgery. However, this has not been confirmed in controlled clinical trials. Peptides should not delay necessary surgical intervention, especially in cases with progressive neurological deficits or cauda equina syndrome. They are best viewed as one component of a comprehensive conservative treatment strategy.
How do peptides for disc repair compare to steroid injections?
Epidural steroid injections provide faster symptom relief but do not promote tissue repair. Peptides take longer to show effects but may support actual structural healing. Some practitioners combine both approaches, using steroids for immediate relief while peptides work on longer-term repair. The mechanisms are fundamentally different: steroids suppress inflammation temporarily, while peptides aim to modulate inflammation while promoting regeneration.
External resources
For researchers serious about optimizing their herniated disc recovery protocols, SeekPeptides offers the most comprehensive resource available, with evidence-based guides, proven protocols, and a community of thousands who have navigated these exact questions. Members access detailed dosing protocols, stacking guides, and ongoing research updates that keep you informed as the science evolves.



