Jan 8, 2026

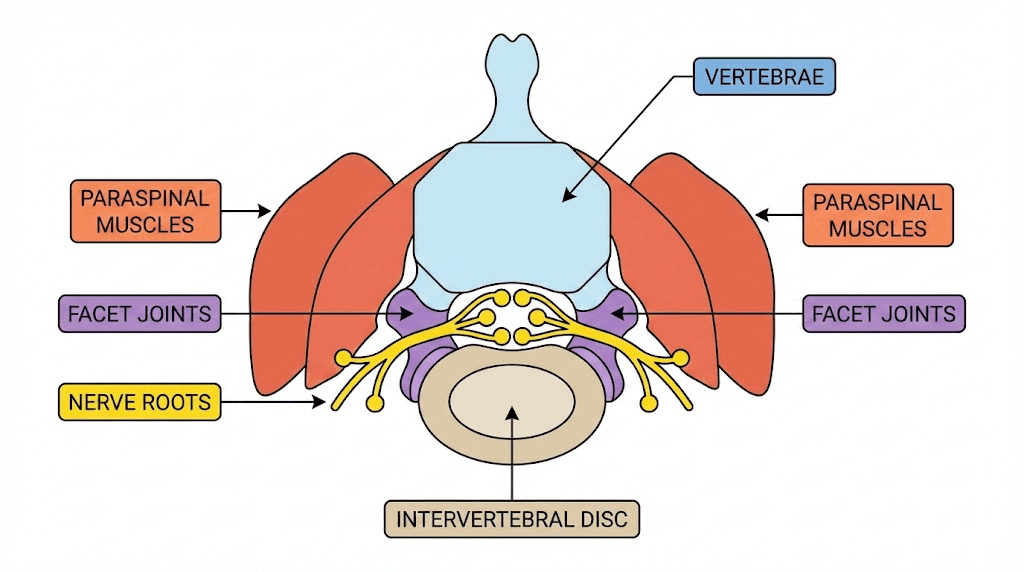
Back pain affects the intricate architecture of your spine, a complex system of vertebrae, intervertebral discs, facet joints, ligaments, muscles, and neural structures that work together to support movement and protect your spinal cord. When any component of this system becomes damaged, inflamed, or degenerative, the resulting pain can range from mild discomfort to debilitating agony that affects every aspect of daily life. Understanding which peptides target specific spinal structures helps researchers develop protocols that address root causes rather than merely masking symptoms.
The spinal column presents unique healing challenges compared to other tissues. Intervertebral discs have minimal blood supply, making nutrient delivery and waste removal difficult. Spinal muscles operate under constant load, rarely getting complete rest for recovery. Nerve tissue heals slowly and can develop sensitization patterns that perpetuate pain long after initial injury resolves. Facet joints experience repetitive stress that accelerates cartilage degradation. Each of these structures requires different therapeutic approaches, and peptides offer targeted mechanisms that conventional treatments often lack.
This guide examines the most effective peptides for back pain based on mechanism of action, tissue specificity, clinical evidence, and practical protocols. We cover BPC-157 for disc and muscle healing, TB-500 for systemic inflammation reduction, GHK-Cu for tissue regeneration, and specialized compounds for nerve pain and spinal degeneration.
Btw, SeekPeptides provides personalized protocol guidance for navigating these complex therapeutic decisions with confidence.
Understanding back pain types and peptide targeting
Effective peptide selection requires understanding the specific tissue causing your back pain. Different structures respond to different peptide mechanisms, and mismatched protocols waste time and resources while potentially missing the actual problem.
Muscular back pain
Muscular back pain involves the paraspinal muscles, quadratus lumborum, multifidus, and other muscles supporting spinal stability. Strains, chronic tension, trigger points, and muscle imbalances create pain patterns that can mimic more serious conditions. Muscular pain typically responds quickly to appropriate treatment because muscles have excellent blood supply and regenerative capacity.
BPC-157 excels for muscular back pain through multiple mechanisms. It accelerates muscle fiber regeneration by upregulating growth factors at injury sites. It modulates nitric oxide systems to improve local blood flow, delivering more nutrients to damaged tissue. It reduces inflammation without the tissue-healing inhibition seen with NSAIDs. Research demonstrates faster recovery from muscle injuries with BPC-157 compared to control groups.
TB-500 complements BPC-157 for muscular issues by promoting cell migration to injury sites and reducing systemic inflammation that can perpetuate muscle guarding patterns. The BPC-157 and TB-500 combination represents the gold standard approach for muscular back pain.
Learn more about fast injury healing protocols and peptide strength protocol benefits for muscle recovery.
Disc-related back pain
Intervertebral disc problems, including herniation, bulging, degeneration, and annular tears, cause some of the most challenging back pain conditions. Discs consist of a gel-like nucleus pulposus surrounded by the fibrous annulus fibrosus. When the annulus tears or weakens, the nucleus can bulge or herniate, potentially compressing spinal nerves. Disc tissue has extremely limited blood supply, making natural healing slow and often incomplete.
BPC-157 shows particular promise for disc healing because it stimulates angiogenesis, the formation of new blood vessels, potentially improving nutrient delivery to avascular disc tissue. Animal studies demonstrate reduced disc degeneration markers and improved disc height with BPC-157 treatment. The peptide also modulates inflammatory cytokines that accelerate disc breakdown.
GHK-Cu supports disc health through its ability to stimulate collagen synthesis and glycosaminoglycan production, key components of healthy disc tissue. Copper peptides also demonstrate anti-inflammatory effects that may slow degenerative processes.
Explore peptides for bone and cartilage repair for related information on structural healing.
Facet joint and arthritic back pain
Facet joints connect vertebrae and allow spinal movement. Like other synovial joints, facets can develop osteoarthritis, inflammation, and cartilage degradation. Facet-mediated pain typically worsens with extension movements and prolonged standing. It often occurs alongside disc degeneration as part of overall spinal aging.
Peptide approaches for facet joint pain focus on cartilage protection and regeneration. BPC-157 demonstrates chondroprotective effects in multiple studies, potentially slowing cartilage breakdown while supporting repair. Peptides for joint pain often include GHK-Cu for its ability to stimulate fibroblasts and support extracellular matrix production.
Anti-inflammatory peptides like KPV may help control the inflammatory cascade that drives facet arthritis progression. The KPV dosage guide provides specific protocols for inflammatory conditions.
Nerve-related back pain
Radicular pain, sciatica, and other nerve-mediated back pain conditions present unique challenges. Compressed or irritated nerves create burning, shooting, or electric sensations that can travel down the legs. Nerve tissue heals slowly, and chronic compression can lead to persistent pain even after structural problems resolve.
BPC-157 shows neuroprotective properties in research, potentially supporting nerve healing while reducing neuroinflammation. Some researchers combine BPC-157 with peptides that have direct neurological effects. Selank demonstrates anxiolytic and potentially analgesic properties that may help with pain perception modulation.
Pinealon and other neurological peptides warrant consideration for chronic nerve pain, though evidence remains more limited compared to tissue-healing peptides.
Best peptides for back pain ranked by effectiveness
Based on mechanism of action, available research, and practical experience from the peptide community, these peptides offer the most promise for back pain conditions.
BPC-157: the cornerstone peptide for back pain
BPC-157 stands as the most versatile and well-researched peptide for back pain of virtually any origin. This pentadecapeptide, derived from human gastric juice, demonstrates remarkable healing properties across multiple tissue types relevant to spinal health.
Mechanisms for back pain:
BPC-157 upregulates growth factors including VEGF, EGF, and others that accelerate tissue repair. It modulates the nitric oxide system, improving blood flow to injured areas. The peptide demonstrates anti-inflammatory effects through multiple pathways without inhibiting the healing process like traditional NSAIDs. Research shows accelerated healing of tendons, ligaments, muscles, and potentially nerve tissue.
Back pain applications:
Muscle strains and chronic tension respond well to BPC-157 through enhanced regeneration and reduced inflammation. Disc problems may benefit from improved angiogenesis and collagen synthesis. Ligament injuries affecting spinal stability show accelerated healing in research. Nerve-related pain may improve through neuroprotective mechanisms.
Dosing for back pain:
Standard protocols involve 250-500mcg twice daily via subcutaneous injection. Some researchers inject near the pain site for local effects, while others use systemic administration. Duration typically ranges from four to twelve weeks depending on condition severity and chronicity. The BPC-157 dosage calculator helps determine appropriate protocols.
What to expect:
Initial improvements often appear within one to two weeks, with inflammation reduction typically preceding structural healing. Acute injuries may resolve within four to six weeks. Chronic conditions often require eight to twelve weeks or longer for significant improvement. Some researchers cycle BPC-157, taking breaks to allow natural healing mechanisms to consolidate gains.
Read the comprehensive guide on how to take BPC-157 and learn about BPC-157 alternatives for additional options.
TB-500: systemic healing support
TB-500, the synthetic version of Thymosin Beta-4, provides systemic healing support that complements BPC-157's more localized effects. Originally studied for cardiac tissue repair, TB-500 demonstrates broad healing properties relevant to back pain conditions.
Mechanisms for back pain:
TB-500 promotes cell migration to injury sites through actin modulation. It reduces inflammation throughout the body, addressing systemic inflammatory states that perpetuate chronic pain. The peptide demonstrates tissue remodeling effects that may help reorganize scar tissue. It supports angiogenesis, improving blood supply to healing tissues.
Back pain applications:
Chronic muscular tension often involves systemic inflammation that responds to TB-500's broad anti-inflammatory effects. Large muscle injuries benefit from enhanced cell migration to injury sites. Post-surgical recovery may accelerate with TB-500's tissue remodeling properties. The peptide helps address the systemic component of chronic pain conditions.
Dosing for back pain:
Loading phase protocols typically involve 2-2.5mg twice weekly for four to six weeks. Maintenance dosing drops to 2mg once weekly or less frequently. Total cycle length commonly ranges eight to twelve weeks. The TB-500 dosage calculator provides specific guidance.
Synergy with BPC-157:
The BPC-157 and TB-500 combination leverages complementary mechanisms. BPC-157 provides targeted local healing while TB-500 creates a systemic pro-healing environment. This stack represents the most common approach for serious back injuries. Learn more about TB-500 benefits and the BPC-157 vs TB-500 comparison.
GHK-Cu: tissue regeneration and anti-aging
GHK-Cu, a copper-binding tripeptide, supports tissue regeneration through mechanisms particularly relevant to degenerative back conditions. While most commonly associated with skin rejuvenation, GHK-Cu demonstrates effects on deeper connective tissues.
Mechanisms for back pain:
GHK-Cu stimulates collagen synthesis, supporting the structural proteins in discs, ligaments, and joint capsules. It promotes glycosaminoglycan production, key components of healthy cartilage and disc tissue. The peptide demonstrates anti-inflammatory effects and antioxidant properties. It may help reset dysfunctional gene expression patterns associated with chronic degeneration.
Back pain applications:
Degenerative disc disease may benefit from enhanced collagen and proteoglycan synthesis. Facet joint arthritis could improve through cartilage-supporting mechanisms. Age-related spinal changes might slow with regular GHK-Cu protocols. Post-injury healing may enhance through improved tissue quality.
Dosing for back pain:
Injectable protocols typically range from 1-2mg daily or every other day. Topical application offers limited penetration for deep spinal structures. Cycles commonly run eight to twelve weeks. GHK-Cu combines well with BPC-157 and TB-500 without receptor competition.
Understanding how long GHK-Cu lasts and copper peptide storage requirements ensures product integrity.
KPV: anti-inflammatory specialist
KPV, a tripeptide derived from alpha-melanocyte stimulating hormone, offers potent anti-inflammatory effects that may benefit inflammatory back pain conditions.
Mechanisms:
KPV modulates inflammatory cytokines including TNF-alpha and interleukins. It penetrates cells to exert direct anti-inflammatory effects. The peptide demonstrates particular potency for gut inflammation but shows systemic effects as well.
Back pain applications:
Inflammatory arthritis affecting the spine may respond to KPV's cytokine modulation. Chronic inflammatory states perpetuating pain cycles could benefit. Autoimmune-related back conditions might improve with regular protocols.
Dosing:
Protocols typically involve 200-400mcg daily via subcutaneous injection. Some researchers use oral or intranasal administration. The KPV dosage guide covers administration options. Consider timing recommendations for optimal effects.
Selank: pain perception modulation
Selank approaches back pain from a different angle, modulating the neurological perception of pain rather than directly healing tissue. This nootropic peptide may help break chronic pain cycles.
Mechanisms:
Selank demonstrates anxiolytic effects that reduce pain-related anxiety and fear-avoidance behaviors. It modulates GABA and serotonin systems involved in pain processing. The peptide shows potential for reducing central sensitization, a key driver of chronic pain.
Back pain applications:
Chronic pain with significant psychological overlay may benefit from Selank's anxiolytic properties. Central sensitization syndromes could improve through neurotransmitter modulation. The peptide may enhance response to physical therapy by reducing fear-avoidance.
Practical considerations:
Selank typically complements tissue-healing peptides rather than replacing them. It addresses the neurological component while BPC-157 and TB-500 address structural issues. Intranasal administration offers convenience.
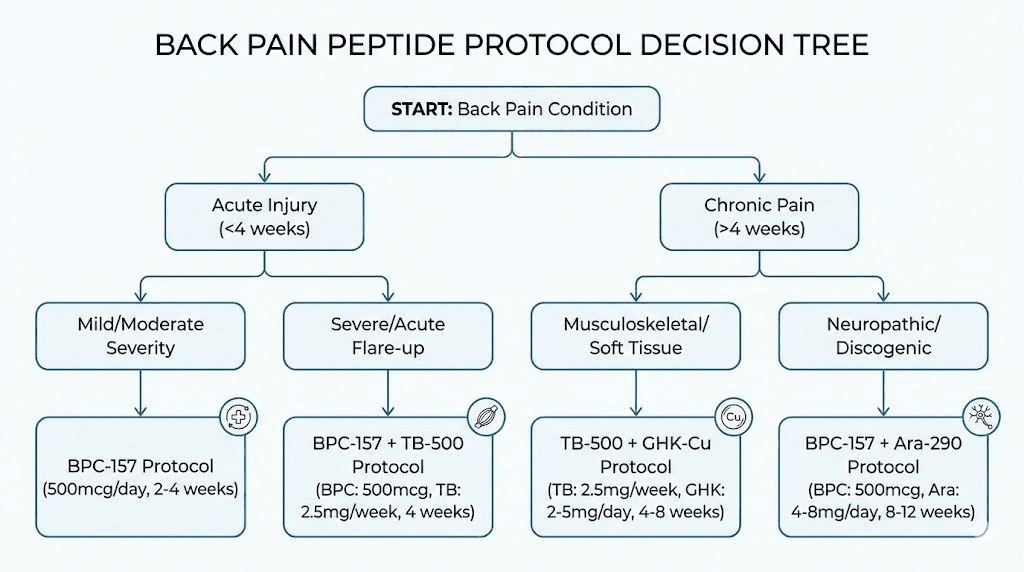
Peptide protocols for specific back pain conditions
Different back pain conditions require tailored approaches. These protocols provide starting points for common presentations.
Protocol 1: acute muscle strain (beginner)
Goal: Rapid recovery from acute paraspinal muscle strain or spasm
Peptides:
BPC-157: 250mcg twice daily, subcutaneous near injury site when possible
Duration: 4-6 weeks typically sufficient for acute strains
Why this works: BPC-157's muscle-regenerating properties accelerate the natural healing timeline. Twice-daily dosing maintains stable tissue levels. Local injection may enhance effects at the injury site. Single-peptide protocols keep things simple for beginners.
Expected timeline:
Days 1-3: Continued acute symptoms, peptide beginning to accumulate
Days 4-7: Inflammation reduction often noticeable, pain decreasing
Week 2-3: Significant improvement in most acute strains
Week 4-6: Return to normal function, consider tapering
Complementary approaches: Gentle movement, avoiding complete rest. Ice for first 48-72 hours, then heat. Gradual return to activity as pain allows.
Cost estimate: $80-150 per month depending on source and quality
Learn about getting started with peptides and common peptide mistakes beginners make.
Protocol 2: chronic muscular back pain (intermediate)
Goal: Address long-standing muscular tension, trigger points, and chronic strain patterns
Peptides:
BPC-157: 500mcg twice daily for enhanced effect
TB-500: 2.5mg twice weekly during loading, then 2mg weekly
Duration: 8-12 weeks for chronic conditions
Why this works: Higher BPC-157 dosing addresses stubborn chronic issues. TB-500 reduces systemic inflammation perpetuating muscle guarding. The combination works synergistically through complementary mechanisms. Extended duration allows cumulative healing.
Expected timeline:
Week 1-2: Initial subtle improvements, possible temporary increase in awareness of issues
Week 3-4: Noticeable reduction in chronic tension patterns
Week 5-8: Progressive improvement, better response to stretching and exercise
Week 8-12: Significant resolution, establishing new baseline
Complementary approaches: Physical therapy or targeted stretching. Trigger point therapy or massage. Core strengthening as pain allows. Postural correction addressing root causes.
Cost estimate: $200-350 per month
Explore the peptide stack calculator and peptide stacks guide for combination protocols.
Protocol 3: disc herniation or bulge (intermediate-advanced)
Goal: Support disc healing and reduce nerve irritation from herniated or bulging discs
Peptides:
BPC-157: 500mcg twice daily, emphasis on lumbar subcutaneous injection
TB-500: 2.5mg twice weekly loading, 2mg weekly maintenance
GHK-Cu: 1-2mg daily for collagen and tissue support
Duration: 12-16 weeks minimum for disc healing
Why this works: BPC-157 promotes angiogenesis that may improve disc nutrition. TB-500 reduces inflammation contributing to nerve irritation. GHK-Cu supports collagen synthesis for annular healing. Extended duration respects slow disc healing timelines.
Expected timeline:
Week 1-4: Inflammation reduction, potential nerve symptom improvement
Week 4-8: Progressive healing, reduced radicular symptoms
Week 8-12: Structural improvements developing, continued symptom reduction
Week 12-16: Consolidation of gains, assessment for continued protocol
Important notes: Disc herniations vary enormously in severity. Some require surgical intervention regardless of peptide use. Monitor for red flag symptoms including progressive weakness, bowel or bladder changes, or worsening neurological deficits. Peptides support but do not replace appropriate medical evaluation.
Cost estimate: $300-500 per month
Read about peptides for bone and cartilage repair for related structural healing information.
Protocol 4: degenerative disc disease and facet arthritis (advanced)
Goal: Slow degenerative processes and support tissue quality in chronic spinal degeneration
Peptides:
BPC-157: 500mcg twice daily ongoing
GHK-Cu: 2mg daily for tissue regeneration
KPV: 300mcg daily for anti-inflammatory effects
Optional: TB-500 2mg weekly for systemic support
Duration: Extended protocols, potentially cycling on and off
Why this works: Degenerative conditions require ongoing support rather than acute treatment. BPC-157 provides baseline healing stimulation. GHK-Cu addresses collagen and matrix degradation central to degeneration. KPV modulates chronic inflammation driving progression. Multiple pathways offer comprehensive approach.
Expected timeline:
Month 1-2: Inflammation management, symptomatic improvement
Month 3-6: Potential slowing of degenerative markers, quality of life improvement
Month 6-12: Assessment of structural changes, protocol optimization
Ongoing: Maintenance protocols as needed, cycling strategies
Complementary approaches: Anti-inflammatory nutrition. Appropriate exercise for spinal health. Weight management to reduce spinal load. Ergonomic optimization.
Cost estimate: $400-600 per month during active phases
Learn about peptides for anti-aging and Epithalon benefits for longevity-focused approaches.
Peptide comparison table for back pain
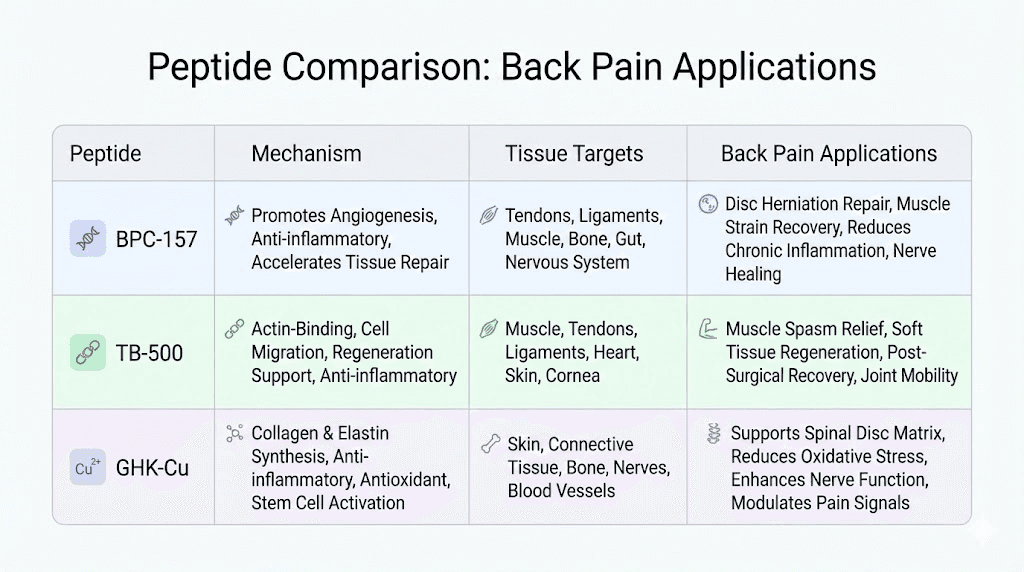
This table compares key peptides for back pain across important factors:
Peptide | Primary Mechanism | Best For | Dose Range | Onset | Cost/Month |
|---|---|---|---|---|---|
BPC-157 | Tissue healing, angiogenesis | All back pain types | 250-500mcg 2x daily | 1-2 weeks | $80-150 |
TB-500 | Cell migration, anti-inflammatory | Chronic pain, large injuries | 2-2.5mg 2x weekly | 2-4 weeks | $120-200 |
GHK-Cu | Collagen synthesis, regeneration | Degeneration, disc disease | 1-2mg daily | 4-8 weeks | $100-180 |
KPV | Anti-inflammatory cytokine modulation | Inflammatory conditions | 200-400mcg daily | 1-3 weeks | $80-150 |
Selank | Pain perception, anxiolytic | Chronic pain, central sensitization | 200-400mcg daily | Days to weeks | $60-120 |
BPC-157 remains the foundation for most back pain protocols due to its versatility across tissue types. TB-500 adds systemic support for more serious or chronic conditions. GHK-Cu provides specialized support for degenerative conditions. KPV and Selank address specific aspects of inflammatory and chronic pain presentations.
The peptide calculator helps determine appropriate dosing, while the peptide cost calculator assists with budgeting across different protocols.
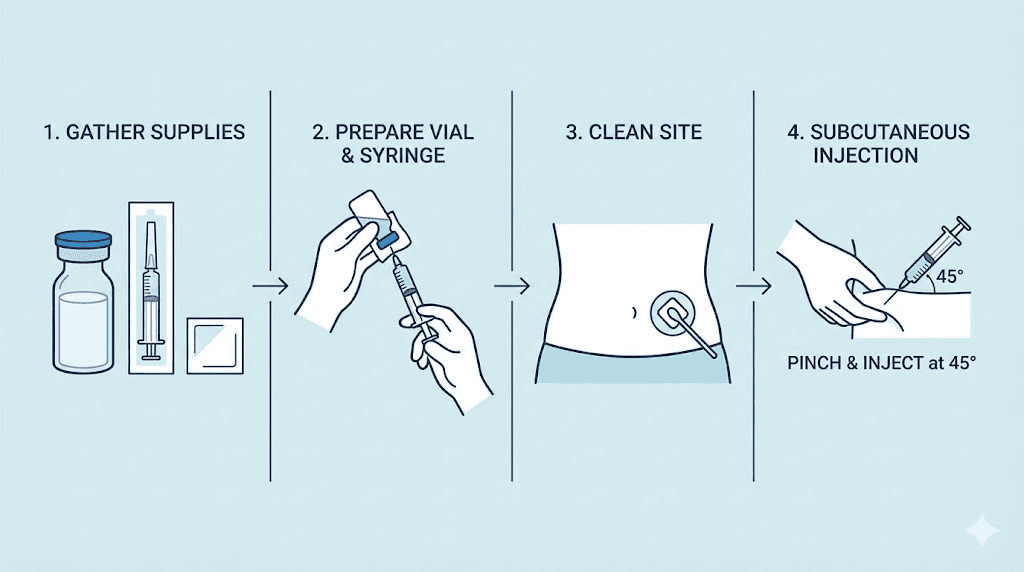
Administration and practical considerations
Proper administration ensures peptide effectiveness and safety. Back pain protocols involve consistent dosing over extended periods, making practical considerations important.
Injection technique for back pain
Subcutaneous injection remains the standard administration route for most back pain peptides. The peptide injections guide covers technique in detail.
Injection site selection:
For systemic effects, standard abdominal subcutaneous injection works well. Some researchers prefer injecting closer to the affected area for BPC-157, such as the lower back subcutaneous tissue for lumbar issues. Evidence for local versus systemic injection effectiveness remains debated. Rotate injection sites to prevent lipohypertrophy regardless of location.
Timing considerations:
BPC-157 typically divides into twice-daily dosing for stable tissue levels. TB-500 requires only twice-weekly administration due to longer biological activity. Morning and evening dosing works for most peptides. Food timing matters less for tissue-healing peptides than for GH secretagogues.
Reconstitution and storage
Proper peptide handling maintains potency throughout your protocol. The peptide reconstitution calculator ensures accurate preparation.
Key points:
Use bacteriostatic water for reconstitution, not sterile water. Store reconstituted peptides in the refrigerator. Most reconstituted peptides remain stable for 4-6 weeks when properly stored. Learn about how long reconstituted peptides last in the fridge and general peptide storage guidelines.
Understanding whether peptides expire helps avoid using degraded products.
Sourcing quality peptides
Peptide quality directly impacts results. Low-quality or mislabeled products waste money and may cause harm. The best peptide vendors guide helps identify reliable sources.
Quality indicators:
Third-party testing with publicly available results. HPLC purity analysis showing greater than 98% purity. Mass spectrometry confirming correct molecular weight. Transparent business practices and customer service. The guide to reading peptide testing results helps evaluate quality documentation.
Research vendor reputation through community feedback. Prime Peptides reviews and similar comparisons provide useful information.
Combining peptides with conventional treatments
Peptides work alongside rather than replacing appropriate medical care. Understanding interactions and complementary approaches optimizes outcomes.
Peptides and physical therapy
Physical therapy remains foundational for back pain regardless of peptide use. Peptides may enhance physical therapy outcomes by accelerating tissue adaptation to therapeutic exercise and reducing pain that limits participation.
BPC-157's healing properties potentially allow more aggressive rehabilitation progression. TB-500's anti-inflammatory effects may reduce post-exercise soreness that sometimes limits therapy intensity. The combination allows researchers to participate more fully in physical therapy programs.
Practical integration:
Continue prescribed physical therapy alongside peptide protocols. Inform treating therapists about your approach if comfortable. Monitor for enhanced recovery that might allow faster progression. Avoid pushing too hard based solely on reduced pain, respect tissue healing timelines.
Peptides and anti-inflammatory medications
NSAIDs and peptides have different risk-benefit profiles. While NSAIDs provide symptomatic relief, research suggests they may impair tissue healing, particularly in muscle and tendon injuries. Peptides aim to enhance healing rather than merely mask symptoms.
Considerations:
Some researchers reduce NSAID use when starting peptide protocols. Others use NSAIDs for acute flares while relying on peptides for ongoing support. BPC-157 demonstrates protective effects against NSAID-induced gut damage, potentially allowing safer NSAID use when needed. Discuss medication changes with healthcare providers.
Peptides and spinal injections
Epidural steroid injections, facet blocks, and similar procedures provide targeted relief for specific back pain conditions. Peptides work through different mechanisms and may complement interventional procedures.
Practical integration:
Timing considerations exist when combining peptides with steroid injections. Some researchers pause peptides briefly around injection procedures, others continue unchanged. No clear consensus exists on optimal integration. Consider that steroids suppress inflammation while peptides aim to resolve underlying issues.
When peptides are not enough
Peptides have limitations. They cannot address severe structural abnormalities requiring surgery. They do not replace proper diagnosis of potentially serious conditions. Red flags requiring medical evaluation include progressive weakness, bowel or bladder dysfunction, unexplained weight loss, fever, or worsening symptoms despite treatment.
Explore peptide safety and risks and peptide legality for important context.
Lifestyle factors that enhance peptide effectiveness
Peptides work within the context of overall health. Optimizing lifestyle factors amplifies peptide benefits for back pain.
Sleep and recovery
Tissue healing occurs primarily during sleep. Growth hormone release peaks during deep sleep, enhancing repair processes. Poor sleep quality undermines peptide effectiveness by limiting the body's capacity to execute healing programs.
Optimization strategies:
Prioritize seven to nine hours of quality sleep. Address sleep disturbances from back pain, recognizing the bidirectional relationship. Consider sleep position optimization for spinal alignment. Some peptides like GH secretagogues may enhance sleep quality. The Ipamorelin and CJC-1295 combination often improves sleep as a side benefit.
Nutrition for tissue healing
Tissue repair requires adequate building blocks. Protein provides amino acids for collagen and muscle synthesis. Specific nutrients support healing pathways that peptides activate.
Key nutritional factors:
Adequate protein intake, typically 0.7-1g per pound of body weight during healing. Vitamin C supports collagen synthesis that GHK-Cu and BPC-157 stimulate. Zinc supports tissue repair and immune function. Omega-3 fatty acids provide anti-inflammatory support complementing peptide effects. Adequate hydration supports nutrient delivery and waste removal.
Movement and exercise
Appropriate movement supports healing rather than hindering it. Complete rest often worsens back pain outcomes compared to gradual activity. Peptides may allow earlier return to movement by reducing pain and accelerating tissue repair.
Exercise considerations:
Gentle movement during acute phases, avoiding complete immobilization. Progressive loading as pain allows, respecting tissue healing timelines. Core strengthening to address root causes of many back pain conditions. Avoiding activities that consistently worsen symptoms during healing phases.
Learn about peptides for muscle growth and peptides for athletic performance for exercise-related applications.
Timeline expectations for back pain improvement
Understanding realistic timelines prevents discouragement and helps assess whether protocols are working.
Acute injuries
Fresh muscle strains, acute disc flares, and new injuries typically respond fastest to peptide protocols.
Week 1: Peptides accumulating in tissue, initial anti-inflammatory effects beginning. Symptoms may continue or even temporarily increase as inflammation mobilizes.
Week 2-3: Noticeable reduction in acute symptoms for most researchers. Pain decreasing, movement improving. Inflammation visibly reduced.
Week 4-6: Significant healing in uncomplicated muscle strains. Continued improvement in disc-related issues. Return to most normal activities for simple injuries.
Week 6-8: Resolution of most acute muscular issues. Continued healing for more complex injuries. Assessment point for protocol continuation.
Chronic conditions
Long-standing back pain, degenerative conditions, and chronic patterns require patience and extended protocols.
Month 1: Initial stabilization, possible subtle improvements. Setting foundation for cumulative benefits. Some researchers notice nothing significant initially.
Month 2-3: More noticeable improvements becoming apparent. Chronic tension patterns beginning to shift. Better response to physical therapy and exercise.
Month 3-6: Substantial improvement for many chronic conditions. Quality of life notably better. Functional capacity increasing.
Month 6-12: Continued gains for degenerative conditions. Assessment of long-term management strategies. Protocol optimization based on response.
Read about how long peptides take to work for general timeline guidance and peptides before and after results for realistic expectations.
Factors affecting response time
Individual variation in peptide response depends on multiple factors.
Injury severity and duration: Longer-standing issues require longer treatment. More severe structural damage heals more slowly regardless of peptide use.
Age: Younger researchers typically respond faster due to higher baseline regenerative capacity. Older individuals may need extended protocols.
Overall health: Metabolic health, nutritional status, and inflammatory load affect healing capacity. Optimizing these factors enhances peptide response.
Peptide quality: Substandard products produce substandard results. Quality sourcing matters enormously.
Protocol adherence: Consistent dosing produces better results than sporadic use. Peptides require sustained presence for optimal effects.
Safety considerations specific to back pain protocols
While tissue-healing peptides generally demonstrate favorable safety profiles, back pain protocols involve specific considerations.
Monitoring during protocols
Extended protocols warrant periodic assessment. Basic monitoring includes tracking symptom changes, watching for unexpected effects, and assessing whether the protocol continues providing benefit.
What to monitor:
Pain levels using consistent rating scales. Functional capacity for daily activities. Range of motion and movement quality. Sleep quality, which often improves with effective protocols. Any unexpected symptoms or reactions.
When to stop or modify protocols
Discontinue or modify protocols if symptoms worsen progressively, if new neurological symptoms develop, if allergic reactions occur, or if significant side effects emerge. Most researchers tolerate tissue-healing peptides well, but individual reactions vary.
Side effect profiles
BPC-157: Generally well-tolerated. Occasional reports of headache, dizziness, or nausea, typically mild and transient. Injection site reactions possible with any injectable.
TB-500: Fatigue reported by some during loading phases. Occasional headache. Generally well-tolerated at standard doses.
GHK-Cu: Minimal side effects reported. Potential for injection site irritation. Theoretical concerns about promoting growth in existing cancers, though evidence is limited.
KPV: Generally well-tolerated. Occasional mild drowsiness. Few reported side effects at standard doses.
Review peptide safety and risks for comprehensive safety information.
How SeekPeptides supports back pain research
SeekPeptides provides comprehensive resources for researchers exploring peptide approaches to back pain and other conditions.
The peptide dosage calculator helps determine appropriate starting doses based on individual factors. The peptide stack calculator assists with combining multiple compounds safely and effectively.
Educational resources including the getting started with peptides guide help newcomers navigate the learning curve. The how peptides work resource explains fundamental mechanisms.
The peptide cost calculator helps budget for extended protocols that back pain conditions often require. Quality vendor comparisons guide sourcing decisions.
SeekPeptides remains committed to providing evidence-based guidance for peptide research across applications including injury healing, muscle growth, and anti-aging.
Helpful resources
May your spine stay aligned, your discs stay hydrated, and your back pain stay resolved. Join SeekPeptides.