Feb 5, 2026
Why tirzepatide fatigue catches so many people off guard
You started tirzepatide expecting weight loss. Maybe better blood sugar control. What you did not expect was the bone-deep exhaustion that hit you three days into your first dose. The kind of tired that coffee cannot fix. The kind that makes you wonder if something is wrong.
You are not imagining it.
Clinical trial data from Eli Lilly shows that fatigue affects between 5% and 7% of people taking Zepbound, the weight loss formulation of tirzepatide. That number climbs with dose. At 5 mg, roughly 5% report it. At 10 mg, 6%. At the highest maintenance dose of 15 mg, fatigue hits 7% of users. And those are just the people who reported it formally in a clinical setting. The real number is almost certainly higher, because many people chalk up their tiredness to poor sleep, stress, or just life, never connecting it to their weekly injection.
But here is the thing that makes peptide-based weight loss fatigue different from ordinary tiredness. It is not random. It follows patterns. It has specific, identifiable causes. And once you understand those causes, you can address most of them directly. This guide covers every mechanism behind tirzepatide-related fatigue, walks you through specific protocols to manage it, explains how peptide adaptation timelines work, and helps you determine when tiredness is normal and when it signals something that needs medical attention. Whether you are new to getting started with peptides or an experienced researcher navigating dose escalation, the information here draws from clinical trial data, FDA prescribing information, and thousands of real-world reports from the SeekPeptides community and beyond.
What the clinical trials actually say about tirzepatide and fatigue
Understanding the data matters. Not the watered-down summaries you find on most health blogs, but the actual numbers from peer-reviewed trials. The SURMOUNT program, which tested tirzepatide for fat loss and obesity, is where most of the fatigue data comes from. Understanding peptide research and clinical studies requires looking at the raw data rather than relying on secondhand summaries.
Fatigue rates across different doses
The FDA prescribing information for Zepbound classifies fatigue broadly. It includes asthenia, which is general weakness. It includes lethargy. It includes malaise, that vague feeling of being unwell. When grouped together under the "fatigue" umbrella, the numbers break down by dose in a clear dose-dependent pattern.
At 5 mg weekly, about 5% of trial participants reported fatigue. At 10 mg, that rose to 6%. At 15 mg, the highest approved maintenance dose, 7% of participants experienced fatigue significant enough to report. Placebo groups reported fatigue at lower rates, confirming the medication itself plays a role beyond what caloric restriction alone would cause.
These percentages might seem small. They are not. In a medication taken by millions of people worldwide, 5% to 7% translates to hundreds of thousands of individuals dealing with meaningful tiredness. If you are one of them, the percentage does not matter much. What matters is understanding why it happens and what to do about it.
The Mounjaro distinction
Here is something most articles miss entirely. Fatigue was not reported as a common side effect in clinical trials for Mounjaro, which is the same molecule, tirzepatide, but approved for weight loss peptide therapy in the context of type 2 diabetes management. The difference likely comes down to dosing protocols and baseline metabolic states. People with type 2 diabetes often start from a place of insulin resistance and elevated blood sugar, where bringing glucose levels under control can actually improve energy. In exit interviews with Mounjaro trial participants, 79% reported increased energy levels over the course of treatment.
That is a remarkable contrast. Same drug. Different populations. Opposite energy outcomes for many people.
SURMOUNT-OSA and the sleep connection
The SURMOUNT-OSA trials added another layer to the fatigue conversation. These studies tested tirzepatide specifically in people with obesity and moderate-to-severe obstructive sleep apnea. The results were striking. Tirzepatide reduced the apnea-hypopnea index, improved sleep quality scores, and significantly reduced daytime sleepiness as measured by the Epworth Sleepiness Scale.
Among treated participants, 71.7% of those classified as non-fatigued at baseline and 69.7% of those classified as fatigued rated their fatigue as "a little better" or "much better" after treatment. For people whose tiredness stems from obesity-related sleep disruption, tirzepatide may actually be the solution, not the cause.
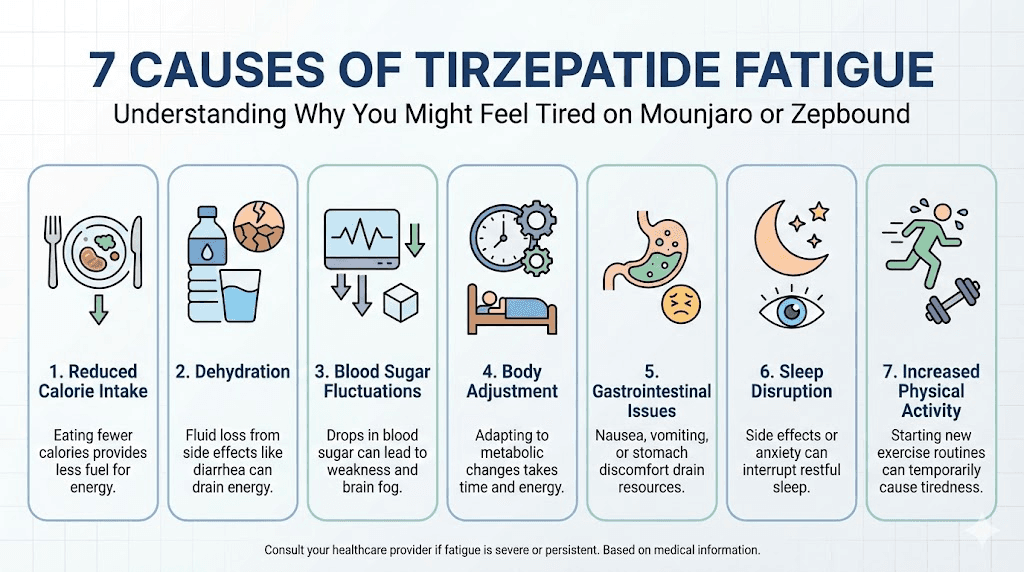
Seven reasons tirzepatide makes you tired
Fatigue on tirzepatide is rarely caused by one thing. It is usually a combination of factors stacking on top of each other. Understanding each mechanism individually helps you target the right solution instead of guessing.
1. The caloric deficit effect
This is the biggest driver of tirzepatide fatigue for most people. And it is the most misunderstood.
Tirzepatide works by activating both GLP-1 and GIP receptors, which dramatically reduces appetite. Research shows that within the first eight weeks of treatment, people start consuming nearly 200 fewer calories at lunch alone compared to baseline. Across all meals and snacks, total daily intake drops substantially. Some people report eating half of what they used to. Others barely manage a full meal per day.
Your body runs on fuel. When fuel intake drops suddenly, energy output drops too. This is basic thermodynamics. Your energy levels depend on adequate caloric intake, and when you go from 2,200 calories to 1,400 calories overnight, your body does not immediately become efficient at pulling from fat stores. There is a transition period. During that transition, you feel it as fatigue, brain fog, and reduced physical performance.
The problem compounds when people do not eat enough protein. Inadequate protein intake below 0.8 grams per kilogram of body weight per day accelerates muscle breakdown, which further reduces metabolic rate and deepens fatigue. Research suggests aiming for 1.2 to 1.6 grams per kilogram daily to preserve lean mass during weight loss. For those doing resistance training, the target rises to 1.6 to 2.2 grams per kilogram.
2. Blood sugar fluctuations
Tirzepatide lowers blood sugar. That is one of its primary mechanisms. But the transition from higher baseline glucose levels to lower, more regulated levels is not always smooth.
When blood sugar drops below what your body is accustomed to, even if the new level is technically healthier, your brain interprets it as a threat. The symptoms include fatigue, shakiness, dizziness, difficulty concentrating, and irritability. This is reactive hypoglycemia, and it is especially common during the first few weeks of treatment and after dose increases.
People who were previously insulin resistant are most susceptible. Their bodies adapted to running on higher glucose levels. Suddenly normalizing those levels feels, paradoxically, like running on empty. The brain uses about 20% of total energy expenditure and relies heavily on glucose. When available glucose drops, cognitive fatigue hits first.
This also matters for anyone combining tirzepatide with other GLP-1 medications or blood sugar lowering drugs. The risk of hypoglycemia and associated fatigue increases significantly with combination therapy. For those exploring peptides to take alongside GLP-1 drugs, understanding these blood sugar dynamics is essential to avoid compounding fatigue issues. Some researchers use peptide stacks for weight loss that include GLP-1 agonists, and each additional compound introduces new variables in blood sugar management.
3. Dehydration and electrolyte imbalance
The gastrointestinal side effects of tirzepatide create a dehydration cascade that many people do not recognize until fatigue is severe. Nausea affects roughly 24% to 31% of users depending on dose. Diarrhea hits 18% to 23%. Vomiting occurs in 8% to 12%. These numbers come directly from the SURMOUNT trials and are consistent across populations studied for both women and men.
Each of these symptoms depletes fluids. But they also deplete electrolytes, specifically sodium, potassium, and magnesium. These minerals are essential for cellular energy production and muscle function. When they drop, even mildly, the result is fatigue, weakness, and brain fog that no amount of sleep will fix. The relationship between peptide safety and hydration is direct. Dehydration is one of the most preventable causes of poor outcomes in any peptide protocol.
The problem is that most people respond to nausea by drinking less, not more. They avoid fluids because their stomach feels unsettled. This makes dehydration worse. A cycle develops where GI symptoms cause fluid loss, fluid loss causes fatigue, and fatigue reduces the motivation to stay on top of hydration. Anyone who has dealt with common peptide mistakes will recognize this pattern. It is one of the most frequent errors new users make.
4. Slowed gastric emptying
Tirzepatide slows down how quickly food leaves your stomach. This delayed gastric emptying is actually part of how the drug works. It keeps you feeling full longer, which reduces calorie intake. But it comes with a cost.
When food sits in your stomach longer, your digestive system diverts more resources to processing it. Blood flow shifts toward the gut. The parasympathetic nervous system activates, which is the "rest and digest" branch of your autonomic nervous system. The result is post-meal sluggishness that can last hours, much longer than the typical food coma most people occasionally experience.
Some users describe it as eating a Thanksgiving meal at every sitting. That heavy, weighted-down feeling that makes you want to lie on the couch. Except it happens after eating a small salad and some chicken. The food volume is small, but the gastric processing time is extended, and the physiological response mimics having eaten a much larger meal. This is similar to how injectable versus oral peptide delivery methods affect absorption timing and side effect profiles. The route and mechanism of action determine how your body processes the compound.
5. Metabolic adaptation and the transition period
Your metabolism does not flip a switch from burning primarily glucose to efficiently burning stored fat. There is a transition period that researchers sometimes call metabolic adaptation, and during this phase, energy levels can drop noticeably.
When caloric intake decreases, your body initially responds by slowing metabolic rate. Thyroid function may downregulate slightly. Non-exercise activity thermogenesis, all the fidgeting, pacing, and unconscious movement you do throughout the day, decreases. Your body is conserving energy because it senses reduced fuel availability.
This adaptive response is ancient biology working against modern goals. Your body does not know you are intentionally losing weight. It thinks food is scarce and responds accordingly. The fatigue you feel is partly your body telling you to move less and conserve what it has. Over time, as your metabolism adjusts to lower caloric intake and becomes more efficient at accessing fat stores, this effect diminishes. But the first 4 to 8 weeks can be rough. Understanding peptide cycle planning helps put this timeline in perspective. Most peptide-based protocols have an adaptation curve, and tirzepatide is no exception. The key difference is that the adaptation with fat loss peptides involves metabolic recalibration that takes longer than the adjustment to other peptide categories.
6. Neurological effects of GLP-1 receptor activation
GLP-1 receptors are not just in your gut and pancreas. They exist throughout your brain, including areas that regulate wakefulness, arousal, and energy perception. When tirzepatide activates these receptors, it directly modulates neural circuits involved in how alert or tired you feel.
This is a mechanism most health articles do not discuss. The medication is literally changing brain signaling patterns related to energy and alertness. As your brain adjusts to these new signals, temporary changes in wakefulness are expected. Some people feel more alert once adapted. Others experience a prolonged adjustment period.
Research on GLP-1 receptor agonists shows that the central nervous system effects extend beyond appetite suppression. They influence reward pathways, stress response, and circadian rhythm regulation. All of these can impact how rested or fatigued you feel. The overlap between GLP-1 effects and other nootropic peptides that target brain function is worth noting. Compounds like Semax and Selank work through entirely different mechanisms but also affect alertness and cognitive function. The brain is remarkably sensitive to peptide signaling, which is why fatigue can be such a prominent early effect of GLP-1 agonist therapy.
7. Lean mass loss
This is the mechanism that gets the least attention but may have the most long-term impact on energy. Weight loss from tirzepatide is not 100% fat. A systematic review of tirzepatide research found that lean tissue loss accounts for approximately 20% to 34% of total weight lost.
Muscle is metabolically active tissue. It burns calories at rest. It supports physical function. When you lose it, your baseline metabolic rate drops, your physical capacity decreases, and daily activities that previously felt easy start feeling harder. That subjective experience of everything requiring more effort is a form of fatigue, and it is directly related to losing muscle mass.
The good news from emerging research is that tirzepatide may actually improve muscle quality even as total lean mass decreases. Imaging studies suggest reductions in intramuscular fat infiltration, meaning the muscle you retain functions better. But this does not fully offset the energy impact of losing lean tissue, especially if protein intake is inadequate and resistance training is absent. This is why researchers studying muscle growth peptides are increasingly interested in combining anabolic peptide protocols with GLP-1 therapy. Compounds like IGF-1 LR3 and growth hormone secretagogues such as CJC-1295 or Ipamorelin are being studied for their potential to preserve lean mass during aggressive weight loss. The peptide stacking guide on SeekPeptides covers these combinations in detail, though any stacking decisions should be made with medical guidance.
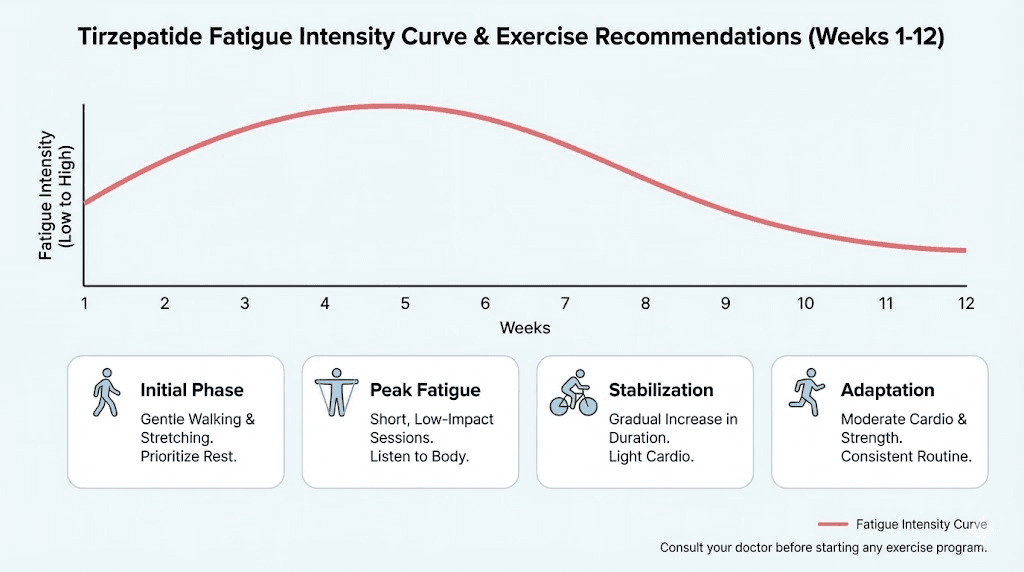
When fatigue appears and how long it typically lasts
Timing matters. Knowing when to expect fatigue and when it should resolve helps you distinguish normal adjustment from something that needs medical attention.
The dose escalation pattern
Tirzepatide uses a gradual dose escalation schedule. You start at 2.5 mg for four weeks, then increase to 5 mg. From there, increases happen in 2.5 mg increments at minimum four-week intervals, up to a maximum of 15 mg weekly.
Fatigue is most common at two specific points. The first is when you start treatment at the initial 2.5 mg dose. The second is each time the dose increases. Many users report that fatigue peaks in the first two to four days after each dose increase, then gradually improves over the next one to three weeks as the body adjusts.
Think of it as a staircase pattern. Each step up in dose brings a temporary spike in fatigue, followed by adaptation. The spike usually diminishes with each successive increase because your body has already partially adapted to the medication mechanisms.
The first four to eight weeks
For most people, the most intense fatigue occurs during the first 4 to 8 weeks of treatment. This window encompasses the initial dose and at least one dose increase. The body is simultaneously adjusting to reduced caloric intake, new blood sugar patterns, altered gastric emptying, and the neurological effects of GLP-1 and GIP receptor activation.
After this initial period, the majority of users report that fatigue diminishes significantly or resolves entirely. The body has adapted to the new metabolic reality. Fat burning pathways become more efficient. Blood sugar stabilization occurs. The digestive system finds its new normal.
But "most people" is not everyone.
When fatigue persists beyond the adjustment period
If you are still experiencing significant fatigue after 8 to 12 weeks at a stable dose, something else may be going on. Persistent fatigue can signal inadequate caloric intake, meaning you have restricted too aggressively and your body is in conservation mode. It can indicate a nutritional deficiency, particularly iron, B12, vitamin D, or magnesium. It can point to dehydration that has become chronic rather than acute.
In some cases, persistent fatigue on tirzepatide reveals a pre-existing condition that was masked or managed before treatment began. Thyroid dysfunction is a common one. So is depression, which sometimes becomes more apparent when the comfort of eating is no longer available as a coping mechanism.
If your fatigue is not improving on the expected timeline, that is not a reason to push through silently. It is a reason to talk to your healthcare provider and investigate the cause. Understanding the difference between normal adaptation and a medical issue is a fundamental part of safe peptide use. You can also consult resources like peptide therapy guides and peptide therapy clinics that specialize in GLP-1 management for additional professional support.
Practical strategies to manage tirzepatide fatigue
Theory is useful. Practical action is better. Here are specific, evidence-based strategies to address each cause of tirzepatide-related fatigue.
Nutrition strategies that actually work
The single most impactful change most people can make is ensuring adequate protein intake. When your appetite is suppressed, every calorie needs to count. Protein should be the non-negotiable foundation of every meal.
Protein targets:
Minimum: 1.2 grams per kilogram of body weight daily
Optimal for fat loss with muscle preservation: 1.4 to 1.6 grams per kilogram daily
If doing resistance training: 1.6 to 2.2 grams per kilogram daily
For a 180-pound person (82 kg), that means 98 to 131 grams of protein daily at minimum, and up to 180 grams if training hard. When you can barely eat 1,200 calories, hitting these targets requires strategic food choices. Lean proteins like chicken breast, fish, Greek yogurt, and egg whites need to be the base of every meal. Protein shakes become tools, not luxuries.
Meal timing matters too. Instead of trying to eat three normal-sized meals that your suppressed appetite will not allow, switch to smaller, more frequent eating occasions. Four to five small protein-rich meals spaced throughout the day keeps blood sugar stable, provides consistent amino acid availability for muscle preservation, and avoids the extreme post-meal fatigue that comes from large meals sitting in a stomach with delayed emptying.
Use our peptide calculator to track dosing precision, and apply the same precision to your nutrition. The peptide cost calculator can also help budget for protein supplements and nutritional support alongside your peptide protocol. Vague intentions like "eat more protein" fail. Specific targets like "40 grams of protein at each of four daily meals" succeed. For a deeper understanding of how peptide dosage calculations translate to real-world protocols, precision is the common thread. The same disciplined approach that ensures accurate peptide reconstitution should apply to your nutrition tracking.
Hydration protocol
Aim for a minimum of 64 ounces (2 liters) of water daily. That is a floor, not a ceiling. If you are experiencing nausea, vomiting, or diarrhea, increase to 80 to 100 ounces. If you exercise, add 16 to 20 ounces for every 30 minutes of activity.
Do not drink large volumes at once. Sip throughout the day. Large boluses of water on a stomach with delayed emptying will worsen nausea and may cause vomiting, which defeats the purpose. Keep a water bottle with you at all times and take small sips every 15 to 20 minutes.
Electrolyte supplementation is not optional when GI side effects are present. Look for electrolyte drinks or supplements that provide sodium, potassium, and magnesium without excessive sugar. Sugar-free electrolyte packets mixed into water twice daily can make a meaningful difference in energy levels within days.
A simple test for hydration status: check your urine color. Pale yellow means adequate hydration. Dark yellow or amber means you need more fluids immediately. This is crude but effective monitoring that requires zero technology. Proper hydration is fundamental to any peptide protocol, whether you are working with tirzepatide, BPC-157, or TB-500. The mixing peptides guide covers reconstitution, but the hydration of your body matters just as much as the hydration of your peptide vial.
Sleep optimization
When your body is running on fewer calories and adapting to new metabolic signals, sleep quality becomes even more critical than usual. Aim for 7 to 9 hours nightly. Not in bed for 7 to 9 hours. Asleep for 7 to 9 hours.
Tirzepatide can improve sleep in some people, particularly those with obesity-related sleep apnea as the SURMOUNT-OSA data showed. But it can also disrupt sleep patterns initially, especially if nausea or GI discomfort occurs at night.
Timing your injection may help. Some users find that injecting in the morning gives GI side effects time to settle before bed. Others prefer evening injections because the initial nausea hits while they sleep through it. There is no universal answer. Experiment to find what works for your body.
Consistent sleep and wake times matter more than total hours in bed. Your circadian rhythm responds to regularity. If you sleep from 11 PM to 7 AM on weekdays and 2 AM to 10 AM on weekends, you are functionally jet-lagged every Monday. Maintain the same schedule regardless of the day, especially while your body adjusts to tirzepatide.
Exercise during the fatigue phase
This seems counterintuitive. You are tired. The last thing you want to do is exercise. But research consistently shows that regular physical activity improves fatigue, even when the fatigue is medication-related.
The key is matching exercise intensity to your current energy capacity.
During peak fatigue (first 2 to 4 weeks): Focus on walking. Twenty to thirty minutes of brisk walking daily is enough to stimulate circulation, improve mood, and maintain basic physical performance. Do not try to maintain your pre-tirzepatide workout intensity. Your body is adapting. Meet it where it is.
As fatigue improves (weeks 4 to 8): Gradually reintroduce resistance training. This is critical for preventing lean mass loss, which itself perpetuates fatigue. Start with two sessions per week focusing on compound movements: squats, deadlifts, rows, presses. Use moderate weights. The goal is muscle preservation, not personal records.
Once adapted (8+ weeks): Return to your normal exercise routine. Many users find they actually have more energy at this stage than they did before starting tirzepatide, because they are carrying less weight, sleeping better, and have more stable blood sugar. Researchers who combine tirzepatide with cardio endurance peptides or athletic performance compounds often report that the energy gains at this stage exceed their pre-treatment baseline. The lighter body, improved insulin sensitivity, and reduced inflammation create an optimal foundation for physical performance.
Tirzepatide fatigue in specific populations
Not everyone experiences tirzepatide fatigue the same way. Age, sex, existing medical conditions, and baseline fitness level all influence how pronounced the tiredness is and how quickly it resolves.
Women over 40
Women in perimenopause and menopause face a compounded fatigue challenge on tirzepatide. Hormonal fluctuations already affect energy levels, sleep quality, and metabolic rate. Adding a caloric deficit on top of declining estrogen and progesterone creates a fatigue picture that can feel overwhelming.
Estrogen supports serotonin production, which influences energy and mood. As estrogen declines, the brain is more sensitive to any additional disruption, including the neurological effects of GLP-1 receptor activation. Peptides for women over 40 require special consideration because of these hormonal interactions. The same dose of tirzepatide may produce more fatigue in a perimenopausal woman than in a man of the same age and weight.
Management for this group includes attention to hormone balance, potentially including hormone replacement therapy alongside tirzepatide. Sleep support becomes critical. Peptides for perimenopause like DSIP and epitalon are being studied for their potential to support sleep and energy in this population, though they should not be combined with tirzepatide without medical supervision.
Men with low testosterone
Obesity itself suppresses testosterone production. As men lose weight on tirzepatide, testosterone levels often improve. But during the initial weight loss phase, the caloric deficit can temporarily further suppress testosterone, especially if protein intake is inadequate and exercise is absent.
Low testosterone causes fatigue, decreased motivation, reduced muscle mass, and poor sleep. These symptoms overlap almost entirely with tirzepatide adaptation effects, making it impossible to distinguish the two without blood work. Men experiencing severe fatigue on tirzepatide should request a full testosterone panel including total testosterone, free testosterone, and SHBG. If levels are low, TRT-related peptide protocols or direct hormone replacement may be necessary alongside the weight loss medication.
People with existing sleep disorders
If you already have poor sleep, adding tirzepatide-related fatigue creates a dangerous combination. Sleep deprivation impairs insulin sensitivity, increases hunger hormones, promotes fat storage, and causes cognitive dysfunction. It directly undermines the goals of tirzepatide treatment.
The good news, as the SURMOUNT-OSA data showed, is that tirzepatide can improve sleep apnea dramatically. But it takes time for weight loss to reach the point where airway obstruction improves. During the gap between starting treatment and achieving meaningful weight reduction, sleep quality may initially worsen before improving.
Researchers interested in DSIP peptide for sleep support or pineal peptides for circadian rhythm regulation are exploring options to bridge this gap. These are research-grade compounds, not approved sleep aids, but they represent the kind of targeted approach that addresses the specific sleep-energy connection during GLP-1 therapy.
Athletes and highly active individuals
Athletes and fitness enthusiasts face a unique version of tirzepatide fatigue. Their caloric demands are higher due to training. When appetite is profoundly suppressed, the gap between energy expenditure and intake widens dramatically. An athlete burning 3,000 calories daily who can only eat 1,500 is in a 1,500-calorie deficit, far more aggressive than what the medication was designed to create.
The result is not just tiredness. It is impaired recovery, decreased performance, increased injury risk, and potential overtraining syndrome. Injury recovery depends on adequate nutrition, and a severe caloric deficit compromises the body capacity to repair training-induced damage.
Athletes on tirzepatide may need to consciously override appetite suppression and eat beyond satiety. Liquid calories from protein shakes, smoothies with added nut butter and olive oil, and calorie-dense recovery meals become essential tools. The peptide dosing guide principle of "minimum effective dose" applies here. Athletes should use the lowest dose that achieves their fat loss goals while still allowing adequate fueling for training.
The role of micronutrient deficiencies in tirzepatide fatigue
When you eat less food, you get fewer nutrients. This obvious fact has serious implications that many prescribers gloss over.
Iron deficiency
Reduced food intake means reduced iron intake. Iron is essential for oxygen transport via hemoglobin. When iron drops, oxygen delivery to muscles and the brain decreases. The primary symptom is fatigue, often accompanied by pale skin, cold hands and feet, and breathlessness during mild exertion.
Women of reproductive age are particularly vulnerable because they already lose iron through menstruation. Adding a caloric deficit on top of existing marginal iron status can push levels into deficiency territory quickly.
If fatigue is accompanied by these symptoms, request a ferritin test from your healthcare provider. Serum ferritin below 30 ng/mL, even if technically within "normal" range, is associated with fatigue symptoms. Optimal levels for energy are typically above 50 ng/mL.
Vitamin B12
B12 is involved in energy metabolism at the cellular level. It supports red blood cell formation and neurological function. Deficiency causes fatigue, weakness, and cognitive difficulties that can mimic or amplify tirzepatide-related tiredness.
People taking metformin alongside tirzepatide for diabetes management are at increased risk of B12 deficiency because metformin impairs B12 absorption. This is a drug interaction that directly contributes to fatigue in people on combination therapy.
Supplementation with brain-supporting nutrients including B12, either as oral supplements or sublingual forms, can address this cause of fatigue. Many compounded formulations of GLP-1 agonists now include B12 for this reason.
Vitamin D
Vitamin D deficiency is already epidemic in the general population, affecting an estimated 35% to 40% of adults. Reduced food intake further decreases dietary vitamin D sources. The symptoms of deficiency, fatigue, muscle weakness, mood changes, overlap almost perfectly with tirzepatide side effects, making it easy to blame the medication for what is actually a nutritional problem.
Ask your provider to check 25-hydroxyvitamin D levels. Optimal levels for energy and muscle function are 40 to 60 ng/mL. If you are below 30, supplementation of 2,000 to 5,000 IU daily (depending on your starting level) can meaningfully improve energy within 4 to 6 weeks.
Magnesium
Magnesium participates in over 300 enzymatic reactions, including energy production in every cell of your body. GI side effects like diarrhea deplete magnesium rapidly. Reduced food intake limits dietary magnesium. The result is a double hit that can cause persistent fatigue, muscle cramps, and poor sleep.
Supplementation with magnesium glycinate (200 to 400 mg at bedtime) serves double duty. It supports energy production and improves sleep quality. Avoid magnesium oxide, which has poor absorption and can worsen diarrhea. The same attention to supplement quality that applies to peptide storage applies to your micronutrient supplements. Cheap, poorly formulated products waste money and may not address deficiencies effectively.
Tirzepatide fatigue versus other medication side effects
Not all tiredness on tirzepatide is from the tirzepatide itself. Other factors and medications can layer on top of the medication effects, creating a compounding fatigue picture that is difficult to untangle without systematic thinking.
Tirzepatide versus semaglutide fatigue
Both semaglutide and tirzepatide can cause fatigue, but the mechanisms and patterns differ slightly. Semaglutide activates only GLP-1 receptors. Tirzepatide activates both GLP-1 and GIP receptors. The dual agonism of tirzepatide produces more pronounced appetite suppression and faster weight loss, which can lead to a more dramatic caloric deficit and potentially more acute fatigue during the initial adjustment period.
However, the GIP receptor activation in tirzepatide may actually support better energy metabolism compared to pure GLP-1 agonists. GIP plays a role in fat metabolism and energy homeostasis that GLP-1 alone does not address. Over time, this dual mechanism may result in better energy levels once the body has adapted, though head-to-head fatigue comparisons between the two drugs are limited.
If you have tried semaglutide and experienced significant fatigue, switching to tirzepatide or vice versa may produce different energy outcomes. Everyone metabolizes these drugs differently, and the receptor activation profiles create distinct physiological responses. People transitioning between medications should understand how long semaglutide takes to suppress appetite versus tirzepatide, as the timelines differ and fatigue patterns will shift accordingly. Using the semaglutide dosage calculator can help ensure appropriate dosing if you switch between these medications.
Medication interactions that worsen fatigue
Tirzepatide does not exist in isolation. Many people take it alongside other medications that also cause fatigue.
Antihypertensives like beta-blockers (metoprolol, atenolol) are well-known for causing fatigue. When combined with tirzepatide-induced caloric restriction, the energy impact can be significant. If you started blood pressure medication around the same time as tirzepatide, the fatigue may be partially or entirely from the antihypertensive, not the weight loss drug.
Antihistamines cause drowsiness in many people. If you take diphenhydramine, cetirizine, or similar medications regularly, they may be contributing to fatigue that gets attributed to tirzepatide.
Metformin can cause B12 depletion as mentioned above, but it also causes its own GI symptoms and fatigue. The combination with tirzepatide can amplify both the GI and energy-related side effects.
Thyroid medications require dose adjustment when body weight changes significantly. If you take levothyroxine and lose 20 or more pounds on tirzepatide, your thyroid medication dose may now be wrong. Both over-treatment and under-treatment cause fatigue. This is one of the most commonly missed causes of persistent tiredness during weight loss.
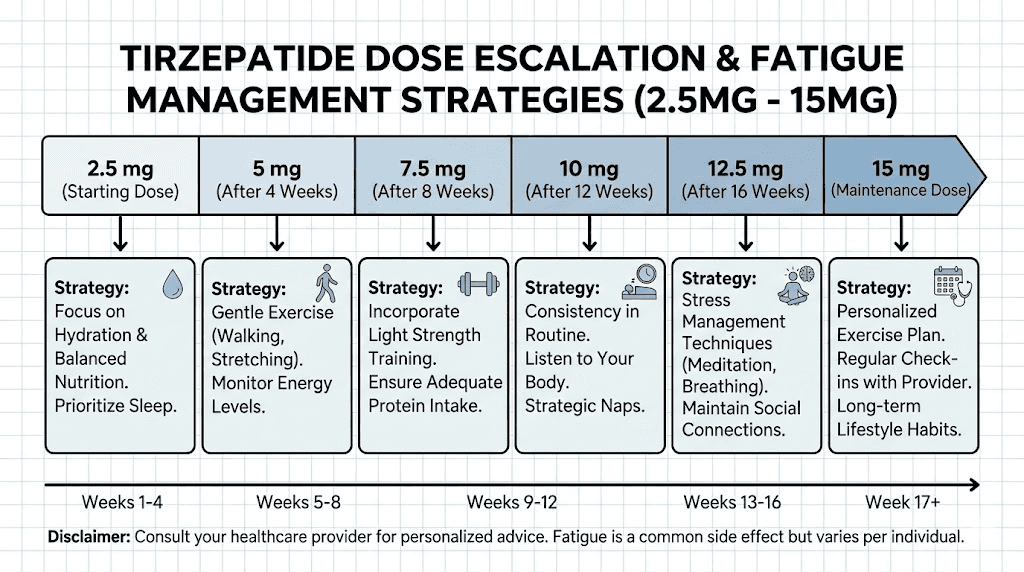
Specific protocols for managing fatigue at each dose level
Different doses create different challenges. Here are targeted strategies for each stage of the tirzepatide dose escalation.
At 2.5 mg (starting dose, weeks 1 to 4)
This is the lowest therapeutic dose, used primarily for tolerability assessment. Fatigue at this dose is usually mild but can still surprise people who expected no side effects from such a low dose.
Focus areas:
Establish hydration habits now, before higher doses make GI symptoms more pronounced
Track protein intake for at least one week to establish a baseline
Begin or maintain light exercise (walking 20 to 30 minutes daily)
Get bloodwork done if you do not have recent results (ferritin, B12, vitamin D, metabolic panel)
Start an electrolyte supplement if experiencing any nausea or GI symptoms
The goal at this stage is building habits that will protect you at higher doses. Think of it as laying foundation before building the house.
At 5 mg (first maintenance dose option)
This is where many people first feel genuine fatigue. The appetite suppression becomes more noticeable, and the caloric deficit deepens.
Focus areas:
Increase protein intake to 1.2 to 1.4 grams per kilogram of body weight
Add a B-complex vitamin supplement if not already taking one
Introduce resistance training twice per week if energy permits
Monitor hydration strictly, aiming for pale yellow urine at all times
If fatigue is severe, eat more calorically dense foods rather than trying to increase food volume
Many people stay at 5 mg as their maintenance dose if they are losing weight effectively and tolerating the medication well. If fatigue is manageable at this level, there may be no need to increase further.
At 10 mg
Appetite suppression intensifies further. The risk of inadequate caloric and protein intake increases. Fatigue at this dose is more likely to have a significant caloric deficit component.
Focus areas:
Increase protein target to 1.4 to 1.6 grams per kilogram
Consider adding a calorie-dense protein shake (protein powder blended with nut butter, banana, olive oil) to ensure minimum caloric intake
Increase resistance training to three sessions weekly if tolerated
Add magnesium glycinate 200 to 400 mg at bedtime if not already supplementing
Monitor body composition if possible, not just scale weight
At this dose, the people who struggle most are those who have not established the nutritional and exercise foundations recommended at lower doses. Playing catch-up is harder than building proactively.
At 15 mg (maximum dose)
The highest approved maintenance dose produces the most weight loss but also the most side effects, including fatigue at 7% incidence. Appetite may be profoundly suppressed.
Focus areas:
Nutritional counseling may be beneficial at this dose, as self-managing adequate nutrition becomes challenging with severe appetite suppression
Protein targets of 1.6 grams per kilogram or higher become critical
Consider tracking all food intake for at least two weeks to identify exactly how much you are consuming
Regular bloodwork every 3 months to monitor for developing deficiencies
If fatigue is severely impacting quality of life, discuss dose reduction with your provider
Not everyone needs 15 mg. If you are achieving your weight loss goals at a lower dose with better energy, the highest dose is not necessarily better. SeekPeptides members discuss this balance between efficacy and side effects extensively, and the consensus is that the best dose is the one that produces results without significantly impairing quality of life. The same minimum-effective-dose principle guides BPC-157 dosing, GHK-Cu dosing, and virtually every other peptide protocol. More is not always better. The right dose is the one that achieves your goals with the fewest side effects.
The muscle preservation connection
We touched on lean mass loss as a cause of fatigue. It deserves deeper exploration because it is the most actionable factor and the one with the most long-term consequences.
What the research shows about tirzepatide and lean mass
A systematic review published in 2025 examining tirzepatide effects on skeletal muscle mass found that lean tissue loss accounts for 20% to 34% of total weight lost during treatment. In the SURMOUNT-3 trial, participants lost significant amounts of lean mass alongside fat mass, even with lifestyle modifications.
The SURPASS-3 MRI substudy, published in The Lancet Diabetes and Endocrinology, provided a more nuanced picture. While total lean mass decreased, the composition of remaining muscle actually improved. Intramuscular fat infiltration decreased, suggesting better muscle quality. This means the muscle you keep functions better, even if there is less of it.
But better quality muscle at reduced quantity still means lower total metabolic capacity. And lower metabolic capacity means the body produces less energy at rest. For a person who has lost 15% of their lean mass alongside their fat loss, daily activities genuinely require a higher percentage of their maximal capacity. That is not psychological. It is physiological fatigue.
Why resistance training is non-negotiable
The research is clear. Pairing weight loss therapy with resistance training significantly reduces lean mass loss. The mechanical stimulus of lifting weights sends a signal to your muscles that they are needed. Without that signal, the body is happy to catabolize muscle along with fat to meet its energy needs during a caloric deficit.
This is not optional advice for people concerned about fatigue. It is the single most effective intervention for maintaining energy levels during significant weight loss.
A basic muscle preservation protocol:
Frequency: 3 sessions per week, minimum
Focus: Compound movements (squats, deadlifts, bench press, rows, overhead press)
Volume: 3 to 4 sets of 8 to 12 repetitions per exercise
Intensity: Moderate to heavy, challenging but maintainable
Progression: Increase weight or reps weekly when possible
Protein timing: 30 to 40 grams of protein within 2 hours of training
If you have never done resistance training, start with bodyweight exercises or machine-based exercises. The barrier to entry is zero. The payoff for energy and fatigue management is enormous.
Tracking the right metrics
Stop obsessing over scale weight alone. The scale cannot tell you whether you lost fat or muscle. It cannot tell you why you are tired.
Better metrics during tirzepatide treatment:
Body composition measurements (DEXA scan, bioimpedance scale, or even waist-to-hip ratio)
Strength benchmarks (can you lift what you lifted last month?)
Energy diaries (rate energy 1 to 10 daily to track trends)
Grip strength (a reliable proxy for overall muscle function)
Walking speed (declining walking speed correlates with lean mass loss)
If your weight is going down but your strength is maintained and energy is stable, you are losing primarily fat. If your weight drops while strength declines and fatigue increases, you are losing too much muscle. The intervention is more protein and more resistance training, not necessarily lower doses. The fat burning peptide guides for men and belly fat peptide resources discuss this body composition distinction in detail. Weight is a poor proxy for health outcomes. Composition, the ratio of fat to lean mass, tells the real story.
When tirzepatide fatigue actually improves energy
We have spent most of this guide discussing fatigue as a problem. But for a significant percentage of users, tirzepatide ultimately improves energy levels. Understanding why helps put the temporary fatigue phase in perspective.
Weight reduction and energy
Carrying excess weight is physically exhausting. Every pound of excess body weight increases the mechanical load on joints, the cardiovascular demand of movement, and the metabolic cost of daily activities. A person carrying 80 extra pounds uses significantly more energy to walk up stairs, get dressed, or even breathe than someone at a healthy weight.
As tirzepatide drives weight loss, this burden decreases. People who lose 30, 50, or 80 pounds consistently report that they have more energy than they have had in years. Activities that left them winded become easy. Stairs are no longer obstacles. Walking is enjoyable instead of painful.
This energy improvement is real and substantial, but it takes time. The initial fatigue from caloric restriction, metabolic adaptation, and medication adjustment comes first. The energy payoff comes after the body has adapted and the weight has come off. Patience is required.
Blood sugar stabilization
Chronically elevated blood sugar, even at levels that do not meet the diagnostic threshold for diabetes, causes persistent low-grade fatigue. The insulin resistance that accompanies excess weight means glucose is less efficiently used by cells. Cells starve even in the presence of abundant circulating glucose.
Tirzepatide dramatically improves insulin sensitivity and normalizes blood sugar. Once this stabilization occurs, many people experience a clarity and energy they had forgotten was possible. The 79% of Mounjaro trial participants who reported increased energy were likely experiencing the benefit of normalized glucose metabolism.
Improved sleep quality
Obesity is the primary risk factor for obstructive sleep apnea, a condition that fragments sleep and causes profound daytime fatigue. Many people with OSA do not know they have it. They just know they are always tired, no matter how much they sleep.
As tirzepatide drives weight loss, sleep apnea improves. Airway obstruction decreases. Sleep becomes more restorative. Daytime alertness improves. The SURMOUNT-OSA trial data confirms this with hard numbers: significant reductions in apnea severity, improved sleep quality scores, and reduced daytime sleepiness.
If you have unexplained fatigue that predates tirzepatide use, undiagnosed sleep apnea might be the root cause. Safety-conscious weight loss that addresses the underlying condition could be the most effective fatigue treatment available.
Reduced systemic inflammation
Excess adipose tissue is not inert. It is an active endocrine organ that produces inflammatory cytokines like TNF-alpha, IL-6, and CRP. Chronic low-grade inflammation causes fatigue that mimics depression, often described as feeling heavy, sluggish, or unmotivated.
Weight loss reduces inflammatory markers. Multiple studies show that tirzepatide treatment lowers CRP and other inflammation biomarkers. As inflammation decreases, the fatigue associated with it resolves. This benefit accumulates over months and becomes one of the most appreciated long-term effects of treatment.
Red flags that mean you should contact your doctor
Most tirzepatide fatigue is manageable and temporary. Some fatigue signals something more serious. Know the difference.
Fatigue with these symptoms requires medical evaluation
Severe dizziness or lightheadedness upon standing. This can indicate significant dehydration, electrolyte imbalance, or hypotension. It is not normal adaptation and needs assessment.
Heart palpitations or irregular heartbeat. Electrolyte imbalances, particularly potassium and magnesium, can cause cardiac rhythm disturbances. Fatigue combined with palpitations is a warning sign that should not be ignored.
Inability to perform daily activities. If fatigue is so severe that you cannot work, drive safely, or care for yourself, the medication may need dose adjustment or temporary discontinuation. This level of impairment exceeds normal adaptation.
Persistent vomiting or diarrhea lasting more than 48 hours. Extended GI symptoms create dangerous dehydration and electrolyte depletion. When these accompany fatigue, medical intervention is needed.
New onset of cold intolerance, hair loss, or significant constipation. These symptoms alongside fatigue suggest thyroid dysfunction, which can be triggered or unmasked by rapid weight loss. Thyroid function testing is warranted.
Mental health changes. If fatigue is accompanied by persistent sadness, loss of interest in activities, feelings of worthlessness, or thoughts of self-harm, seek medical attention immediately. These may indicate depression that has developed or worsened during treatment.
Fatigue that worsens over time instead of improving. Normal adaptation fatigue improves. Fatigue that gets progressively worse despite following management strategies suggests an underlying cause that needs investigation.
Blood work to request
If fatigue persists beyond the expected adaptation window, ask your healthcare provider for the following tests:
Complete blood count (screens for anemia)
Ferritin (iron stores, not just serum iron)
Vitamin B12
25-hydroxyvitamin D
Comprehensive metabolic panel (electrolytes, kidney function, liver function)
TSH and free T4 (thyroid function)
Fasting glucose and HbA1c (blood sugar trends)
Magnesium (often not included in standard panels)
These tests cover the most common correctable causes of persistent fatigue during tirzepatide treatment. Many are inexpensive and widely available. The information they provide can mean the difference between suffering through unnecessary fatigue and resolving it quickly with targeted intervention.
Comparing tirzepatide fatigue to other weight loss medication fatigue
Tirzepatide is not the only weight loss medication that causes fatigue. Understanding how it compares helps put the side effect in context.
Tirzepatide versus semaglutide (Wegovy/Ozempic)
Semaglutide is a pure GLP-1 receptor agonist, while tirzepatide activates both GLP-1 and GIP receptors. In terms of fatigue specifically, there are no direct head-to-head comparisons from clinical trials. However, the indirect evidence suggests similar fatigue profiles, with most tiredness occurring during dose escalation and resolving with adaptation.
The key difference may be in the magnitude of caloric deficit. Tirzepatide typically produces more weight loss than semaglutide at equivalent timepoints, which means a potentially larger caloric deficit and more pronounced initial fatigue. But the additional GIP receptor activation may support more efficient fat metabolism, potentially improving energy once adapted.
For those weighing options between semaglutide dosing and tirzepatide, fatigue profiles should be considered alongside efficacy, cost, and other side effects. Neither medication is clearly better or worse for fatigue in all cases.
Tirzepatide versus retatrutide
Retatrutide is a triple agonist that activates GLP-1, GIP, and glucagon receptors. It is still in clinical development, but early trial data shows even more pronounced weight loss than tirzepatide, which raises the possibility of more significant caloric deficit-related fatigue. The glucagon receptor activation could theoretically either worsen or improve energy levels, as glucagon promotes glycogen breakdown and fat oxidation, potentially providing more available fuel. Understanding the retatrutide dosage chart helps frame the dose-response relationship.
Until phase 3 trials provide detailed adverse event data, any comparison between retatrutide and tirzepatide fatigue is speculative. But the general principle applies: the more aggressive the weight loss, the more likely short-term fatigue during adaptation. The retatrutide buying guide covers what is currently known about this compound, including its side effect profile compared to existing GLP-1 drugs. For researchers considering cagrilintide for weight loss or cagrilintide with semaglutide, the fatigue considerations are similar. Any compound that creates a significant caloric deficit will produce some degree of adaptation fatigue.
Tirzepatide versus older weight loss medications
Older medications like phentermine actually increase energy through stimulant effects. But that energy comes at the cost of increased heart rate, blood pressure, insomnia, and potential dependency. The "energy" from stimulants is borrowed, not generated. Comparing the peptide approach to weight loss with stimulant-based approaches reveals fundamentally different philosophies: peptides work with your body biology to change hunger signaling and metabolic patterns, while stimulants override fatigue signals without addressing underlying causes.
Tirzepatide fatigue, while unpleasant, does not carry these cardiovascular risks. It is a temporary adaptation effect, not a structural consequence of the drug mechanism. Once through the adjustment period, most users find sustainable, genuine energy improvements that stimulant-based drugs cannot provide. Some researchers exploring tesofensine for weight management are interested in compounds that provide mild stimulant effects alongside appetite suppression, though the long-term safety profile of such approaches remains under investigation.
The broader comparison between peptides versus other compound classes applies here. Peptide-based approaches tend to have more manageable side effect profiles with temporary adaptation periods, while other compound classes may have more immediate effects but also carry more significant long-term risks. The legal status of peptides and their regulatory framework also reflects this safety distinction, as approved GLP-1 medications like tirzepatide have undergone extensive clinical testing for both efficacy and safety.
The science of how your body adapts to tirzepatide over time
Understanding adaptation at the biological level helps explain why fatigue is temporary for most people and why the long-term energy outcome is typically positive.
Metabolic flexibility and fat oxidation
Your body has two primary fuel sources: glucose from carbohydrates and fatty acids from stored fat. Most people eating a standard diet rely primarily on glucose. When tirzepatide reduces caloric intake, glucose availability drops and the body must increase its reliance on fat oxidation.
The ability to efficiently switch between these fuel sources is called metabolic flexibility. People with obesity and insulin resistance typically have poor metabolic flexibility. Their bodies are locked into glucose burning and struggle to access fat stores efficiently. This is partly why the initial caloric deficit feels so draining. The body needs fuel, has plenty stored as fat, but cannot access it quickly enough.
Over weeks of treatment, metabolic flexibility improves. Enzymes involved in fat oxidation upregulate. Mitochondrial function adapts. The body becomes progressively better at using its own fat stores for energy. This transition is one of the primary reasons fatigue diminishes over time. You are literally becoming a more efficient machine. The fuel is there, and your body is finally learning to use it.
Research on MOTS-c peptide has shown similar metabolic flexibility improvements, as MOTS-c directly influences mitochondrial energy production. The overlap between GLP-1 therapy effects and mitochondrial peptide research is an active area of scientific investigation that may yield combination protocols in the future.
Hormonal adaptation
Tirzepatide affects multiple hormonal systems beyond insulin and glucagon. Ghrelin, the hunger hormone, initially may remain elevated even as appetite is suppressed, creating a confusing signal where the body biochemically "wants" food but the brain does not register the desire. This hormonal mismatch contributes to fatigue in the early weeks.
Leptin, the satiety hormone, is produced by fat cells. As fat mass decreases, leptin levels drop. The brain interprets falling leptin as starvation, triggering conservation responses that include fatigue, reduced thermogenesis, and mood changes. This is the same mechanism that makes all diets increasingly difficult over time, and it applies to tirzepatide-assisted weight loss as well.
Cortisol, the stress hormone, may also be elevated during the adaptation phase. The physiological stress of caloric restriction, combined with the stress of adapting to a new medication, creates a cortisol response that contributes to fatigue, disrupted sleep, and water retention. As the body stabilizes on treatment, cortisol typically normalizes, and the fatigue associated with it resolves.
For those interested in how different peptides influence hormone balance, the hormonal cascade during tirzepatide adaptation illustrates just how interconnected these systems are. Adjusting one hormone pathway inevitably affects others, which is why a holistic approach to managing side effects, rather than targeting fatigue alone, produces better outcomes.
Gut microbiome changes
This is a newer area of research, but evidence is emerging that GLP-1 agonists alter the gut microbiome. Changes in bacterial populations can influence energy metabolism, inflammation, neurotransmitter production, and even mood. The gut-brain axis is a bidirectional communication pathway, and when the gut environment shifts rapidly, as it does with altered eating patterns and delayed gastric emptying, the effects extend well beyond digestion.
Some researchers hypothesize that part of the fatigue during tirzepatide adaptation is microbiome-mediated. As bacterial populations shift in response to changed eating patterns, they produce different metabolites, some of which may temporarily impair energy production. As the microbiome reaches a new equilibrium, this effect resolves. The role of peptides for gut health in supporting microbiome transitions is an area where compounds like KPV and BPC-157 are generating particular interest. BPC-157, which is derived from human gastric juice, has documented effects on gut mucosal integrity and may support gut health during the disruptive early phase of GLP-1 therapy.
Real-world strategies from the tirzepatide community
Clinical trial data tells you what happens on average. Real-world experience fills in the details that trials miss.
Injection timing experiments
Many users find that the day and time of their weekly injection influences their fatigue pattern. Common approaches include:
Friday evening injection. This is the most popular timing reported in online communities. The logic: peak side effects, including fatigue, hit Saturday and Sunday when you can rest. By Monday, the worst has passed and you can function at work.
Monday morning injection. Some users prefer to get the injection over with at the start of the week, finding that the mild fatigue on Monday and Tuesday is manageable with caffeine and activity, and they feel progressively better through the week.
Bedtime injection. A smaller group reports success with injecting just before bed. They sleep through the initial side effect peak and wake up with manageable symptoms the next day.
There is no single best time. The right timing depends on your work schedule, exercise routine, and individual response patterns. What matters is being intentional about it rather than randomly choosing a time.
The "energy food" approach
When appetite is suppressed and you can only eat small amounts, choosing the right foods becomes disproportionately important. Community members who manage fatigue well tend to prioritize:
Calorie-dense protein sources: Nuts, nut butters, full-fat Greek yogurt, salmon, eggs with yolks. These deliver more fuel per bite than high-volume, low-calorie foods like salads.
Complex carbohydrates: Sweet potatoes, oats, quinoa, brown rice. These provide sustained energy without the blood sugar spike and crash of simple carbohydrates. When you can only eat a small amount, making those carbs slow-digesting matters.
Strategic caffeine: Most users find moderate caffeine intake (200 to 300 mg daily, equivalent to 2 to 3 cups of coffee) helps manage fatigue without worsening nausea. The key is timing it away from meals to avoid GI interaction, and not relying on it as a substitute for adequate nutrition and sleep.
The supplement stack that helps
Based on both research evidence and widespread community experience, a targeted supplement approach can meaningfully reduce tirzepatide fatigue:
Electrolyte supplement (sugar-free, containing sodium, potassium, magnesium): daily, twice daily if GI symptoms are present
Magnesium glycinate (200 to 400 mg): at bedtime, for energy production and sleep quality
Vitamin B complex: daily, for energy metabolism support
Vitamin D3 (2,000 to 5,000 IU): daily, based on tested levels
Iron (if ferritin is low): as directed by healthcare provider, not taken with calcium or coffee
Omega-3 fatty acids (2 to 3 grams combined EPA/DHA): for inflammation reduction and brain function
This is not a list of expensive specialty supplements. These are basic, widely available, evidence-supported nutrients that address the specific deficiency risks created by reduced food intake during tirzepatide treatment. For researchers who also use other peptides alongside their GLP-1 therapy, understanding how many peptides you can take at once helps frame the total supplement and peptide load. The peptide stack calculator can help plan combinations, while the nutritional supplements above address the metabolic consequences that no amount of peptide optimization can overcome without adequate nutrition.
Mental health, fatigue, and the emotional side of treatment
Not all fatigue is physical.
Tirzepatide changes your relationship with food. For many people, food was a coping mechanism, a source of comfort, a stress reliever, a social connector. When appetite is profoundly suppressed, these emotional functions of eating are disrupted. The resulting emotional exhaustion can manifest as physical tiredness.
Emotional eating withdrawal
This is not a term you will find in clinical literature, but it describes a real phenomenon. When the food-reward pathway is blunted by GLP-1 receptor agonism, people who relied on food for emotional regulation find themselves without a primary coping tool. The emotional energy required to navigate this transition, to develop new coping mechanisms and process emotions without the buffer of food, is real and depleting.
If you find that your fatigue is accompanied by sadness, irritability, a sense of loss around food, or difficulty finding pleasure in activities you previously enjoyed, the tiredness may have a significant emotional component. This does not mean tirzepatide is causing depression. It means the medication has removed a coping tool, and you need to build new ones.
Therapy, particularly cognitive behavioral therapy, can be remarkably effective during this transition. Many weight loss clinics now recommend psychological support alongside medication for exactly this reason. Researchers exploring peptides for anxiety and mood support are studying how compounds like Selank and Semax might support emotional resilience during weight loss transitions, though these remain research compounds and should not replace professional mental health support.
Decision fatigue and food planning
There is a paradox to eating on tirzepatide. You are less hungry, but you need to be more strategic about what you eat. Every meal needs to count nutritionally. This requires planning, grocery shopping, meal preparation, and constant decision-making about food choices that optimize limited appetite.
This cognitive load is genuinely fatiguing. People who previously ate intuitively (or impulsively) now need to track protein, plan meals, ensure adequate calories, and time their eating around medication effects. The mental energy this requires is non-trivial, especially in the first months of treatment.
Simplification helps. Choose 4 to 5 reliable, protein-rich meals you enjoy and rotate through them. Reduce decisions by meal-prepping on weekends. Use a simple tracking method rather than an elaborate system. Reduce the cognitive load so it does not compound the physical fatigue.
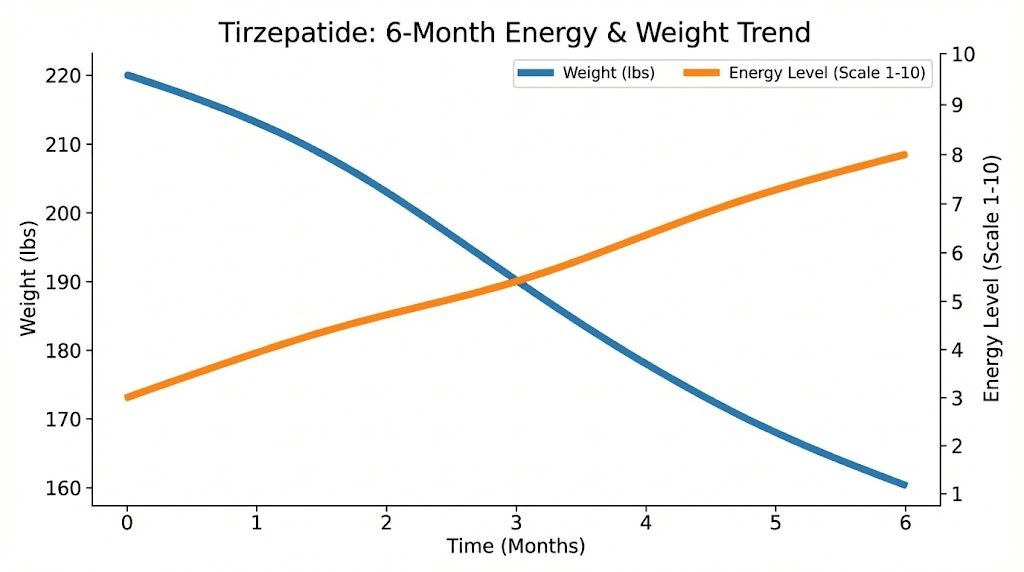
Long-term energy outlook on tirzepatide
The fatigue discussion is dominated by short-term experiences because that is when fatigue is most acute. But the long-term energy picture on tirzepatide is significantly more positive than the early weeks suggest.
What happens after 6 months
By the 6-month mark, most users who have maintained treatment report substantially improved energy compared to their pre-treatment baseline. The reasons compound over time.
Significant weight has been lost, reducing the physical burden of daily movement. Blood sugar is stabilized, providing consistent fuel to cells. Inflammation markers have decreased. Sleep quality has improved, especially if sleep apnea was present. Cardiovascular fitness has improved because exercise is easier at a lower body weight. Mood has often improved from accomplishing meaningful health goals.
The 6-month version of most tirzepatide users bears little resemblance to the 6-week version. Patience through the initial fatigue phase is rewarded with genuine, sustainable improvements in energy and vitality. This mirrors the experience many people have with other peptide before and after transformations, where the early weeks are challenging but the long-term outcomes justify the investment. The peptide transformation process, regardless of which compound is involved, rarely follows a linear improvement curve. There are setbacks, plateaus, and adaptation challenges before the benefits fully emerge.
What happens if you stop tirzepatide
This is relevant to the fatigue discussion because some people consider stopping the medication specifically because of tiredness. It is important to understand what happens next.
Weight regain after discontinuing tirzepatide is common and well-documented. In the SURMOUNT-1 extension study, participants who stopped tirzepatide regained approximately two-thirds of their lost weight within one year. With weight regain comes the return of obesity-related fatigue, inflammation, insulin resistance, and potentially sleep apnea.
Stopping the medication to avoid temporary fatigue often trades a short-term problem for a long-term one. The fatigue from carrying excess weight is chronic and worsening. The fatigue from tirzepatide adaptation is temporary and improving. Understanding alternatives to Ozempic and other fat burning peptides can help if tirzepatide is not tolerable, but switching to a different GLP-1 agonist will likely produce similar adaptation fatigue. The mechanism is fundamentally about caloric restriction, not specific to any one drug.
For researchers exploring how long peptides take to work, the timeline for tirzepatide energy improvement follows a similar pattern: initial adjustment, progressive improvement, and eventual benefit that exceeds baseline.
Maintenance phase energy
Once you reach your goal weight or a stable dose you plan to maintain long-term, the energy picture typically stabilizes at a level significantly better than pre-treatment. The caloric deficit narrows as your body requires fewer calories at a lower weight. The adaptation period is complete. Nutritional strategies are established. Exercise is easier and more effective.
Many long-term users describe their energy at the maintenance phase as "better than I have felt in years" or "back to how I felt in my twenties." This is the endpoint the temporary fatigue is working toward. It is worth remembering during the difficult early weeks. The longevity peptide research community has long understood that short-term discomfort during a protocol often precedes long-term benefit. The principle applies to weight loss and muscle gain programs just as it does to anti-aging and recovery protocols. Investing through the difficult adaptation phase yields returns that compound over time.
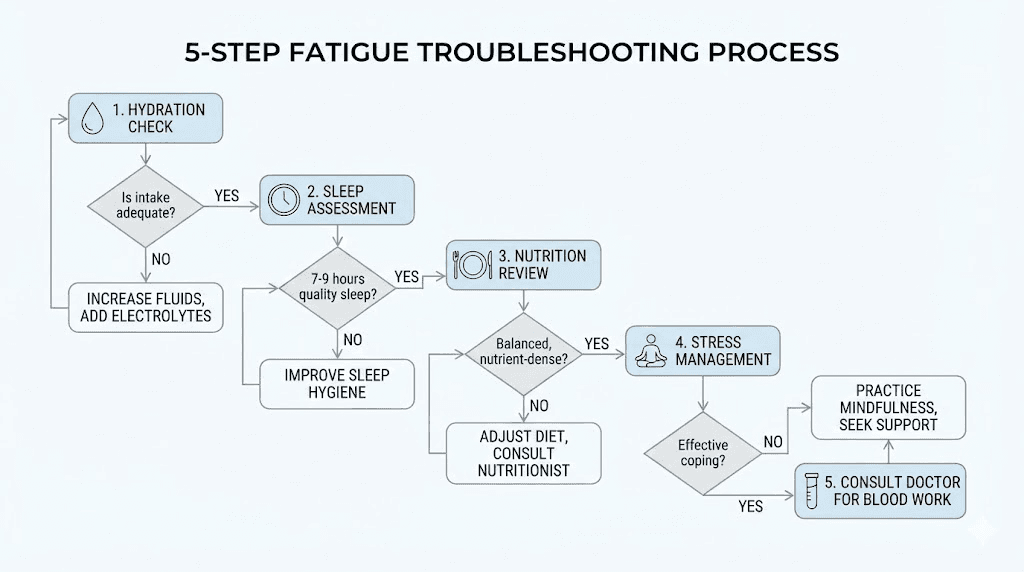
A step-by-step fatigue troubleshooting guide
When fatigue hits, you need a systematic approach, not random interventions. Follow this decision tree in order.
Step 1: Rule out dehydration (check first, always)
Check urine color. If dark yellow or amber, drink 16 to 20 ounces of water with electrolytes immediately. Wait 2 hours. If fatigue improves even slightly, dehydration was a contributing factor. Increase baseline fluid intake by 20% and add an electrolyte supplement.
This step alone resolves or significantly improves fatigue for approximately 30% of people. It costs nothing, has no risks, and takes minimal effort. Every peptide reconstitution guide emphasizes the importance of proper dilution. Apply the same thinking to your body. You need adequate hydration to function.
Step 2: Assess caloric and protein intake
Track everything you eat for 3 days. Calculate daily protein intake. If below 1.2 grams per kilogram body weight, this is almost certainly a major contributor to your fatigue. Increase protein immediately through strategic food choices or supplementation.
If total caloric intake has dropped below 1,200 calories daily (for women) or 1,500 calories (for men), you are likely in too aggressive a deficit. Your body is in conservation mode. You need to eat more, even though your appetite says otherwise. Use calorie-dense, nutrient-dense foods to bring intake up without requiring large food volumes.
Step 3: Evaluate sleep quality
Are you actually sleeping 7 to 9 hours? Not in bed for that long, but asleep? If sleep is disrupted by nausea, GI discomfort, or other factors, address those first. Experiment with injection timing. Consider whether undiagnosed sleep apnea might be contributing.
Step 4: Check for medication interactions
Review all current medications with your pharmacist. Beta-blockers, antihistamines, certain antidepressants, and metformin can all contribute to fatigue independently. If you started any new medication around the same time as tirzepatide, it may be the actual cause or a significant contributor.
Step 5: Get blood work
If steps 1 through 4 do not resolve the fatigue, blood work is the next step. Request the panel listed earlier in this guide. Ferritin, B12, vitamin D, thyroid function, and a comprehensive metabolic panel will cover the most common correctable causes. Bring the results to your provider and discuss targeted interventions based on what the numbers show.
This systematic approach prevents the common mistake of throwing random supplements at the problem without understanding the root cause. It is the same disciplined methodology that SeekPeptides applies to every peptide dosage protocol: identify the variable, measure it, and adjust specifically.
Frequently asked questions
How long does tirzepatide fatigue typically last?
Most people experience the worst fatigue during the first 4 to 8 weeks of treatment, particularly during dose escalation. Fatigue typically peaks in the first 2 to 4 days after starting or increasing a dose, then gradually improves over 1 to 3 weeks. If fatigue persists beyond 8 to 12 weeks at a stable dose, consult your healthcare provider to investigate other potential causes like nutritional deficiencies or thyroid dysfunction.
Does the fatigue get worse at higher doses?
Clinical data shows a dose-dependent relationship. Fatigue affects approximately 5% of people at 5 mg, 6% at 10 mg, and 7% at 15 mg. However, many people find that their body adapts more quickly to each subsequent dose increase because the underlying mechanisms (caloric deficit, metabolic adaptation) are already partially adjusted. The first dose increase tends to be the hardest. Understanding peptide dosing principles helps frame why gradual escalation exists: it gives your body time to adapt before adding more stimulus.
Will caffeine help with tirzepatide fatigue?
Moderate caffeine intake (200 to 300 mg daily) can provide temporary relief, but it does not address the underlying causes. Caffeine can also worsen dehydration and potentially increase nausea in some people. Use it strategically as a bridge while implementing the foundational strategies of adequate nutrition, hydration, and exercise, rather than as a primary solution.
Is tirzepatide fatigue different from semaglutide fatigue?
The fatigue mechanisms are similar, as both involve caloric deficit, metabolic adaptation, and GLP-1 receptor effects. The main difference is that tirzepatide often produces a larger caloric deficit due to stronger appetite suppression, which can cause more acute initial fatigue. However, the dual GLP-1/GIP agonism of tirzepatide may support better energy metabolism once adapted. Individual responses vary significantly between the two medications.
Should I reduce my tirzepatide dose if fatigue is severe?
If fatigue severely impacts your ability to function in daily life, discuss dose adjustment with your prescriber. Options include staying at a lower maintenance dose, extending the interval between dose increases, or temporarily reducing the dose. The lowest effective dose that achieves your health goals while maintaining quality of life is the right dose. Not everyone needs to reach 15 mg.
Can I take supplements to prevent tirzepatide fatigue?
Targeted supplementation can meaningfully reduce fatigue. Evidence supports electrolyte supplements (especially if experiencing GI side effects), magnesium glycinate (200 to 400 mg), B-complex vitamins, vitamin D3 (based on tested levels), and iron (if ferritin is low). These address the specific nutritional gaps created by reduced food intake and GI-related losses during treatment.
Does tirzepatide fatigue mean the medication is not working for me?
No. Fatigue is a common and usually temporary adjustment effect, not a sign of treatment failure. In fact, appetite suppression, which drives the caloric deficit that causes fatigue, is one of the primary mechanisms through which the medication produces weight loss. Fatigue during dose escalation often correlates with effective appetite suppression and active weight loss. Think of it like the initial soreness after starting a new exercise program. The discomfort signals that the stimulus is working, not that something is wrong. The fundamentals of peptide therapy apply here: most effective compounds have an adaptation period before benefits fully emerge.
Will exercise make tirzepatide fatigue worse?
During the acute fatigue phase, intense exercise can worsen tiredness. However, moderate exercise, particularly walking and light resistance training, actually improves fatigue in most people. Start with low-intensity activity and gradually increase as your body adapts. Resistance training specifically is critical for preserving muscle mass, which helps maintain metabolic rate and long-term energy levels. Athletes exploring safe muscle growth peptides alongside their tirzepatide protocol should prioritize exercise timing around injection days to minimize the impact of peak side effects on training quality.
External resources
PMC: Effects of tirzepatide on skeletal muscle mass systematic review
PMC: Association between tirzepatide and fatigue in SURMOUNT-OSA
For researchers serious about understanding every aspect of their peptide protocol, SeekPeptides provides comprehensive guides, detailed protocols, and a community of experienced researchers who have navigated these exact questions. From dosage calculations to safety protocols, the platform covers everything you need to make informed decisions about your peptide research.
In case I do not see you, good afternoon, good evening, and good night. Join SeekPeptides.



