Feb 4, 2026
Most people get the timeline wrong
You started semaglutide three days ago. Maybe a week. And you are standing in front of the fridge, stomach growling, wondering if the injection actually did anything at all. The food noise is still there. The cravings have not budged. And every forum post you read says "I lost my appetite on day one." So what gives? Why is your experience different?
Here is the truth nobody tells you upfront. Semaglutide does not flip a switch.
It is not like a painkiller that kicks in within an hour. This is a GLP-1 receptor agonist that works through a gradual biological process, one that involves receptor binding in your brain, changes to gastric emptying speed, and a slow build of steady-state blood concentration over weeks. The appetite suppression is real. Clinical trials prove it. A randomized controlled study of 30 subjects with obesity showed semaglutide reduced total daily energy intake by 24% compared to placebo, with lunch intake dropping by 35%. Those are massive numbers. But they did not happen overnight, and they will not happen overnight for you either.
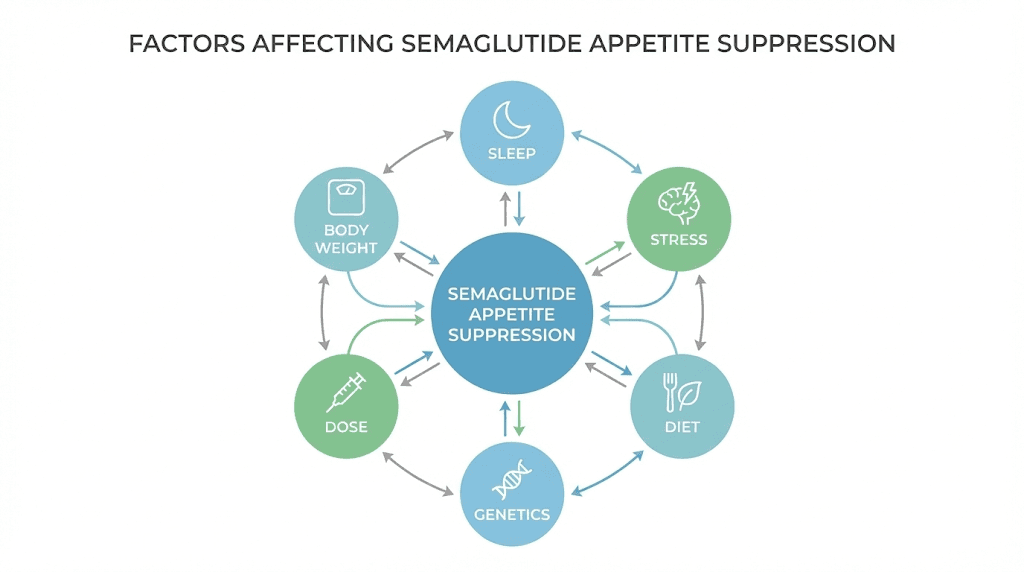
The timeline varies. Some people notice reduced hunger within the first week at 0.25 mg. Others do not feel meaningful appetite changes until they reach 1.0 mg or higher, which takes at least eight weeks with standard dose escalation. Your body weight, your metabolic health, your current dose, your sleep quality, your stress levels, and even your genetics all play a role in how quickly semaglutide suppresses your appetite.
This guide breaks down exactly what happens at each stage, what the research actually shows, and what you can do if the appetite suppression is not kicking in as fast as you expected. SeekPeptides has compiled the most comprehensive timeline available, drawn from clinical data, published studies, and real-world protocols.
How semaglutide actually suppresses your appetite
Before you can understand the timeline, you need to understand the mechanism. Semaglutide is not a stimulant. It is not an appetite suppressant in the traditional sense, like phentermine or caffeine. It works through an entirely different pathway, one that mimics a hormone your body already produces.
GLP-1, or glucagon-like peptide-1, is a gut hormone released after you eat. It signals your brain that food has arrived, triggers insulin release, and slows gastric emptying so food stays in your stomach longer. The problem is that natural GLP-1 breaks down within minutes. Semaglutide is an engineered analog that resists degradation, giving it a half-life of approximately seven days. That is why you only inject once per week.
But the appetite suppression does not come from the gut alone.
Research published in the journal Cell Metabolism identified that semaglutide crosses the blood-brain barrier and accumulates in the area postrema, a region of the brainstem that lacks the typical blood-brain barrier protections. From there, it activates GLP-1 receptors on specific neurons. These include anorexigenic POMC/CART neurons in the hypothalamus, the hunger control center of the brain, and it simultaneously inhibits orexigenic NPY/AgRP neurons that drive hunger. The result is a fundamental shift in how your brain perceives hunger and satiety.
There is more. Semaglutide also affects the reward centers in your brain. A study published in Science Direct found that while semaglutide reduces appetite, it actually increases dopamine signaling during reward collection. This means the medication changes your relationship with food at a neurological level, not just your physical hunger signals. The food noise that so many people describe, that constant background hum of thinking about what to eat next, quiets down because the neural pathways driving those thoughts are being directly modulated.
Semaglutide also slows gastric emptying significantly. Food stays in your stomach longer after each meal, which means you physically feel full for extended periods. A 20-week clinical trial of semaglutide 2.4 mg showed a 35% reduction in ad libitum energy intake compared to placebo, driven largely by this combination of central appetite suppression and delayed gastric emptying. Participants reported less hunger, fewer food cravings, better control over eating, and a reduced preference for high-fat, energy-dense foods.
The three pathways working together
Think of semaglutide appetite suppression as a three-pronged system. First, the hypothalamic pathway reduces your baseline hunger by activating satiety neurons and suppressing hunger neurons. Second, the reward pathway reduces cravings and food noise by modifying how your brain responds to food-related thoughts and stimuli. Third, the gastric pathway keeps food in your stomach longer, creating a lasting physical sensation of fullness after meals.
All three pathways need time to reach full effect. The hypothalamic changes depend on steady-state blood levels of semaglutide, which take four to five weeks to establish at any given dose. The reward pathway changes develop more gradually as the brain adapts to altered dopamine signaling. And the gastric emptying effects, while noticeable early, become more pronounced at higher doses. This is why the appetite suppression timeline stretches across weeks and months rather than hours and days.
The dose escalation schedule and why it matters for appetite
Semaglutide for weight management follows a specific dose escalation protocol. You do not start at the full therapeutic dose. There is a medical reason for this, and it directly affects when you will feel appetite suppression.
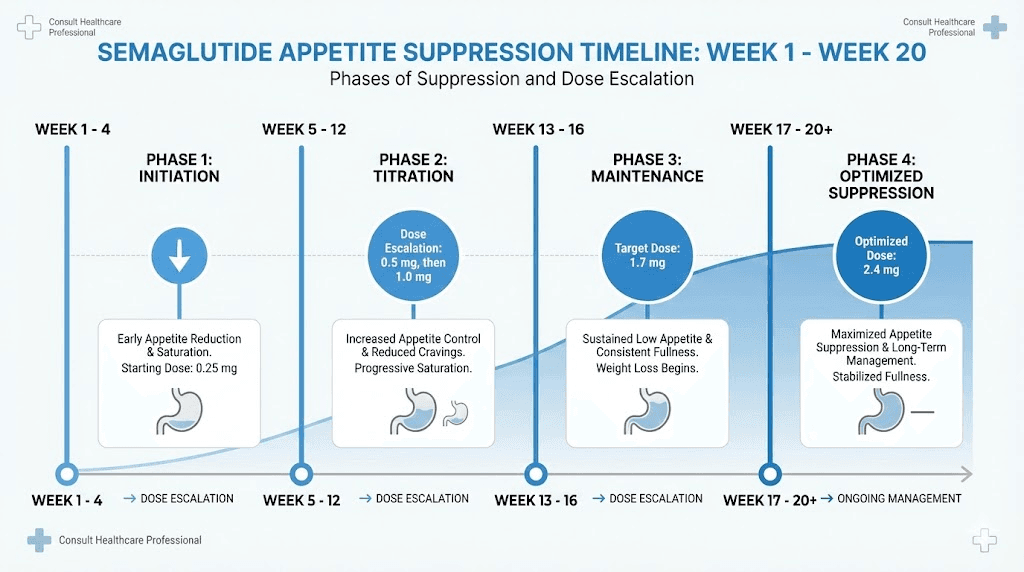
The standard Wegovy schedule looks like this:
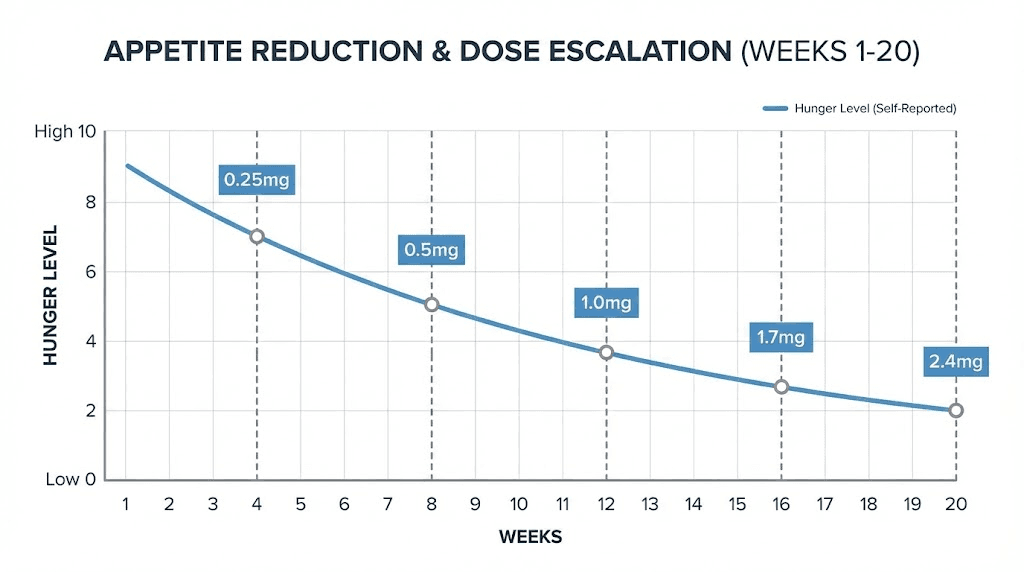
Weeks 1 through 4: 0.25 mg once weekly. This is the initiation dose. Its primary purpose is to let your gastrointestinal system adjust to the medication. Many people experience nausea, and starting low minimizes that. Appetite suppression at this dose ranges from nonexistent to mild. Some people notice slight changes in hunger. Most do not notice anything dramatic.
Weeks 5 through 8: 0.5 mg once weekly. The first real step up. This is where some people start noticing reduced hunger, smaller portions feeling satisfying, and the beginning of food noise reduction. But for many, it is still subtle. Your body is building toward steady-state levels, and the optimal therapeutic concentration has not been reached yet.
Weeks 9 through 12: 1.0 mg once weekly. A significant inflection point. Clinical data from the STEP trials shows meaningful appetite suppression becomes consistent around this dose for most people. The 12-week crossover study that measured actual food intake used 1.0 mg as the maintenance dose and found the 24% reduction in daily energy intake at this level. This is often where people say "it clicked."
Weeks 13 through 16: 1.7 mg once weekly. Appetite suppression deepens further. People at this dose commonly report that they forget to eat, that meals feel like a chore, and that the constant mental focus on food has largely disappeared. The therapeutic effects are becoming well established.
Week 17 and beyond: 2.4 mg once weekly. The full maintenance dose for weight management. Maximum appetite suppression for most users. Studies show the combination of reduced hunger, altered food preferences, and enhanced satiety reaches its peak at this dose. Long-term data from the STEP 1 trial showed participants maintained significant appetite reduction through week 68 at this dose level.
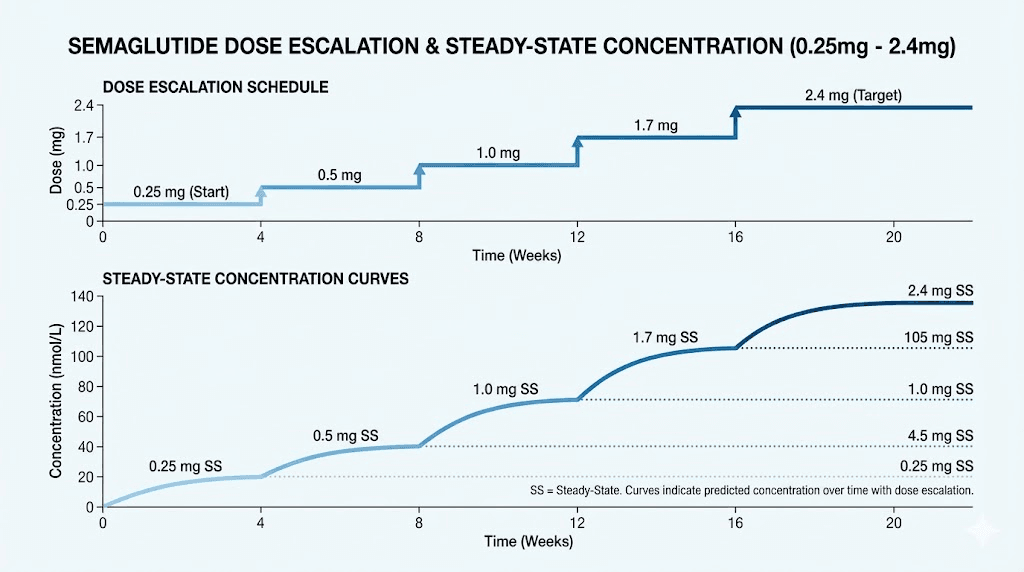
Why steady-state concentration matters
Here is a detail most articles skip. Semaglutide has a half-life of approximately seven days. That means it takes about four to five weeks of consistent weekly injections at the SAME dose for blood levels to stabilize. This is called reaching steady state. Before steady state, you are still building up the drug in your system. The appetite effects are inconsistent. Some days feel better than others. You might have strong appetite suppression on days two and three after injection, then feel it wear off by day six or seven.
Once steady state is reached, the levels remain more consistent throughout the week. The appetite suppression becomes more reliable, more even, less of a roller coaster. This is why the minimum timeline for meaningful effects is four to five weeks at any given dose, and why many people do not experience the full benefit until they have been at their maintenance dose for at least a month.
Week-by-week timeline of appetite changes
Based on clinical trial data, published research, and documented patient experiences, here is what to expect at each phase of semaglutide treatment. Remember that individual variation is significant. This is a general guide, not a guarantee.
Week 1: the adjustment period
You have just taken your first 0.25 mg injection. Some people feel a slight reduction in appetite within the first few days. Others feel nothing at all. Both responses are normal.
What is actually happening inside your body is important to understand. The semaglutide is beginning to bind to GLP-1 receptors, but blood levels are still very low. You are nowhere near steady state. The drug is starting to slow gastric emptying slightly, which may cause mild nausea or a feeling of fullness after meals that lasts longer than usual. But the central nervous system effects, the brain-level appetite suppression, have barely begun.
If you feel slightly less hungry, great. If you feel no different, that is equally normal and does not mean the medication will not work for you. The 0.25 mg dose exists primarily for tolerability, not efficacy.
Weeks 2 through 4: building the foundation
By week two, some people notice subtle changes. Not dramatic appetite loss, but small shifts. Maybe you leave food on your plate without thinking about it. Maybe the afternoon snack craving is a little quieter. Maybe you eat dinner and feel satisfied sooner than usual. These are early signs that the GLP-1 pathway is engaging.
By the end of week four, you are approaching steady state at the 0.25 mg dose. If you are going to feel anything at this dose level, this is when it becomes most noticeable. But keep perspective. The 0.25 mg dose is one-tenth of the full therapeutic dose. Any appetite changes at this point are a bonus, not the expectation.
Common experiences during weeks two through four include slightly smaller portions feeling sufficient, reduced interest in snacking between meals, occasional nausea (particularly after fatty meals), and a vague sense that food is less interesting than before. None of these are dramatic. They are subtle. And that subtlety is normal.
Weeks 5 through 8: the first real shift
You have moved to 0.5 mg. Things start to change. The jump from 0.25 to 0.5 doubles your dose and typically produces the first clear appetite suppression that most people can confidently identify. You are not just eating slightly less. You are actively noticing that you are less hungry.
This is also when many people first experience the "food noise" reduction. That constant background mental chatter about what to eat, when to eat, what sounds good for dinner, whether there are snacks in the pantry, it starts to quiet down. For people who have dealt with food obsession, emotional eating, or binge eating tendencies, this change can feel profound. Some describe it as mental clarity around food for the first time in their lives.
Gastric emptying is noticeably slower now. Meals keep you full for hours. If you eat a reasonable lunch at noon, you might not feel genuinely hungry until 6 or 7 PM. This natural extension of satiety makes caloric reduction almost effortless for many people.
Weight loss typically becomes measurable during this phase. Clinical data suggests people lose an average of 2% of body weight per month during the first six months, and weeks five through eight is often when that trajectory becomes visible on the scale.
Weeks 9 through 12: the inflection point
At 1.0 mg, semaglutide appetite suppression hits a meaningful stride. This is the dose used in the landmark crossover study that showed 24% reduction in total daily energy intake and 35% reduction in lunch consumption. The research is clear: 1.0 mg produces reliable, measurable appetite suppression in most people with obesity.
What does that feel like in practice? People at this dose commonly report that they can eat half of what they used to and feel completely satisfied. Portion sizes shrink dramatically without willpower or effort. Food preferences shift, often away from greasy, high-calorie options and toward lighter, simpler meals. The clinical data backs this up. Subjects on semaglutide showed reduced explicit liking for high-fat, non-sweet foods and reduced implicit wanting for high-fat foods overall.
By week 12, if you have been consistent with injections and dose escalation, you should be experiencing clear appetite suppression. Not everyone will feel it to the same degree, but the vast majority of people notice significant changes by this point. If you have reached week 12 at the correct dose and still feel no appetite change whatsoever, that is worth discussing with your prescriber.
Weeks 13 through 16: deepening the effect
The 1.7 mg dose further amplifies everything. Hunger becomes almost irrelevant for many people. The challenge at this point often shifts from "I am still hungry" to "I need to remember to eat enough." Caloric intake drops substantially, and maintaining adequate protein intake becomes a conscious effort.
Side effects may increase at this dose. Nausea, constipation, and occasional stomach discomfort are more common. But for most people, the trade-off is worth it because the appetite suppression is now unmistakable. There is no ambiguity. You know the medication is working.
Weeks 17 through 20: full therapeutic effect
At 2.4 mg, you have reached the maximum recommended dose for weight management. Steady state at this dose takes another four to five weeks, meaning the full effect of the 2.4 mg dose is not reached until approximately weeks 21 through 22. But by week 17, you are already experiencing powerful appetite suppression from the accumulated weeks at escalating doses.
The STEP 1 trial, published in the New England Journal of Medicine, showed that participants on semaglutide 2.4 mg lost an average of 14.9% of body weight by week 68. The appetite suppression that drives this weight loss is well established by week 20, and participants described it as sustainable and consistent.
This is also where long-term patterns emerge. Eating habits have fundamentally changed. Portions are smaller. Cravings are minimal. The relationship with food has shifted from obsessive to functional. Many people describe eating as something they do because they need to, not because they want to, which is a radical change for anyone who has struggled with weight.
Months 5 through 12: maintenance and stabilization
After approximately 20 weeks, the appetite suppression becomes second nature. You have established new eating patterns. Your body has fully adapted to the medication. Weight loss continues but slows, typically from about 2% per month to about 1% per month after the sixth month.
The appetite effects remain stable for most people. However, some experience a gradual return of hunger as their body adapts. This is not tolerance in the classical sense, but rather the body finding a new equilibrium. If hunger starts to return noticeably, it may be worth discussing with your prescriber whether the dose needs adjustment or whether lifestyle factors are contributing.
Factors that affect how quickly semaglutide suppresses your appetite
Not everyone follows the same timeline. Research shows significant individual variability in semaglutide response. Here are the factors that influence how fast you will experience appetite suppression.
Starting body weight and BMI
People with higher starting body weight often require higher doses to achieve meaningful appetite suppression. This is a matter of drug distribution. Semaglutide distributes throughout the body, and a larger body means the same dose produces a lower concentration per kilogram of body weight. Someone weighing 120 kg will have lower blood concentrations at 0.5 mg than someone weighing 80 kg.
This does not mean semaglutide will not work for heavier individuals. It means the therapeutic dose may need to be higher, and the timeline to meaningful appetite suppression may extend further into the dose escalation schedule. Clinical trials enrolled participants with BMIs ranging from 27 to 45+, and the medication showed efficacy across the full range, but the magnitude of effect correlated with reaching adequate therapeutic doses.
Metabolic health and insulin resistance
People with type 2 diabetes or significant insulin resistance may experience semaglutide differently. The medication was originally developed for diabetes management, and its glucose-regulating effects interact with appetite pathways in complex ways. Some diabetic patients report earlier appetite changes because semaglutide improves blood sugar stability, which reduces the hunger spikes caused by glucose fluctuations.
Conversely, severe insulin resistance may blunt some of the central appetite effects initially, as the metabolic environment needs to stabilize before the brain-level changes fully manifest.
Genetic factors
Variability in GLP-1 receptor expression and post-receptor signaling creates meaningful differences in individual response. Some people have more GLP-1 receptors in their hypothalamus. Some have more efficient downstream signaling pathways. Research published in Frontiers in Endocrinology noted that genetic polymorphisms may impact therapeutic outcomes, though specific predictive markers have not yet been clinically validated.
This explains why two people at the same dose, same weight, and same health status can have dramatically different appetite responses. It is not about effort or willpower. It is about biology.
Sleep quality
This one surprises people. Poor sleep dramatically increases hunger hormones, specifically ghrelin, and reduces satiety hormones like leptin. If you are sleeping poorly, you are fighting against semaglutide with your own endocrine system. Studies show that sleep deprivation can increase caloric intake by 300 to 400 calories per day, which can partially or completely offset semaglutide appetite suppression.
People who prioritize seven to nine hours of quality sleep consistently report faster and stronger appetite suppression from semaglutide. This is not a minor factor. It is one of the biggest modifiable variables in your control.
Stress and cortisol
Chronic stress elevates cortisol, which encourages fat storage and drives cravings for high-calorie comfort foods. Cortisol-driven hunger operates through different pathways than the ones semaglutide targets. This means you can have semaglutide suppressing your hypothalamic hunger signals while cortisol simultaneously drives you toward the cookie jar through the stress-response pathway.
Managing stress through exercise, meditation, therapy, or lifestyle changes amplifies semaglutide effectiveness. Ignoring chronic stress partially undermines it.
Diet composition
What you eat matters for how well semaglutide works. High-protein, high-fiber diets enhance the satiety effects of GLP-1 receptor agonists. Protein triggers additional satiety hormones (PYY, CCK) that work alongside semaglutide. Fiber slows gastric emptying further, compounding the delayed emptying effect of the medication. Together, they create a synergistic effect that makes appetite suppression stronger and longer-lasting.
Conversely, liquid calories, highly processed foods, and low-protein diets partially bypass semaglutide mechanisms. Liquid calories empty from the stomach faster, reducing the gastric fullness benefit. Ultra-processed foods are engineered to override satiety signals. And low-protein diets miss the complementary hormonal support that protein provides.
Medication interactions
Certain medications can counteract semaglutide appetite effects. Antipsychotics, some antidepressants, insulin, sulfonylureas, corticosteroids, and beta-blockers are known to promote weight gain or increase appetite through various mechanisms. If you are taking any of these while on semaglutide, the appetite suppression may be delayed or partially blunted.
This does not mean you should stop other medications. It means you should have realistic expectations about the timeline and discuss potential interactions with your prescriber.
Hydration
Dehydration can masquerade as hunger. When your body needs water, it sometimes sends hunger signals instead of thirst signals. If you are not drinking adequate water (generally 2 to 3 liters per day), you may interpret dehydration cues as persistent hunger and assume semaglutide is not working when the actual problem is simple fluid intake.
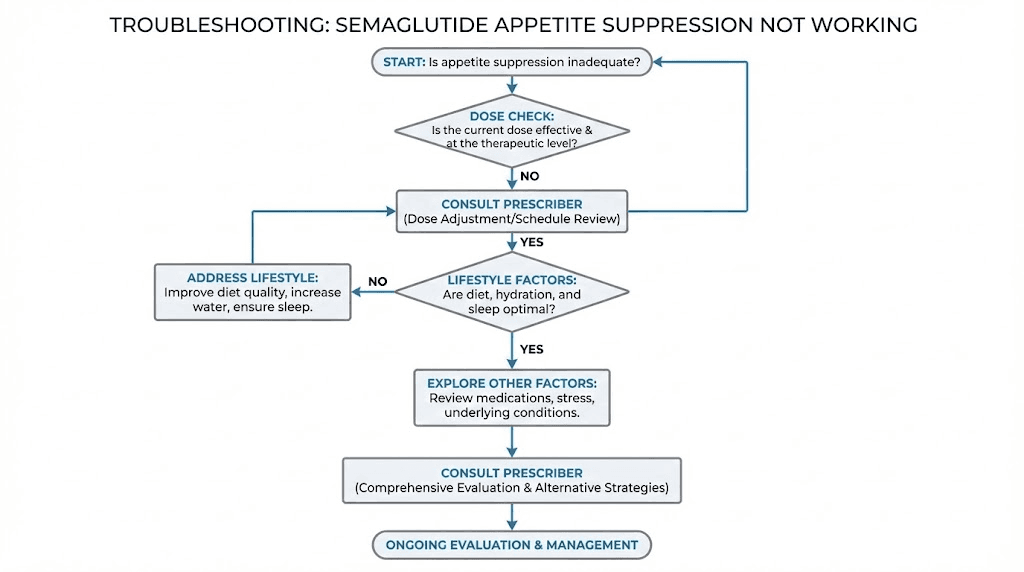
What to do if semaglutide is not suppressing your appetite
You have been on semaglutide for several weeks. Maybe longer. And the appetite suppression everyone talks about has not materialized. You are still hungry. Still thinking about food. Still eating the same amounts. Before you conclude the medication does not work for you, run through this troubleshooting checklist.
Check your timeline expectations
First, be honest about where you are in the dose escalation. If you are still at 0.25 mg or 0.5 mg, you simply may not have reached a therapeutic dose yet. The landmark study showing 24% energy intake reduction used 1.0 mg. Many people do not experience meaningful appetite suppression until 1.0 mg or higher. Patience through the early escalation phases is essential.
Have you been at your current dose for at least four weeks? Steady state takes four to five weeks at each dose level. If you just increased your dose last week, you have not given it enough time to build to full effect.
Evaluate your injection technique
Improper injection technique can reduce absorption. Subcutaneous injections need to go into fatty tissue, typically in the abdomen, thigh, or upper arm. If you are injecting too shallow (intradermally) or too deep (intramuscularly), the absorption kinetics change, and you may not be getting the full dose effectively.
Make sure you are:
Pinching the skin to create a fold of fatty tissue
Inserting the needle at a 45 to 90 degree angle
Holding the needle in place for 5 to 10 seconds after injection
Rotating injection sites to avoid lipodystrophy
Storing the medication properly (refrigerated, away from light)
Assess your sleep
Are you getting seven to nine hours of quality sleep consistently? Sleep deprivation is one of the most common and most underestimated saboteurs of semaglutide effectiveness. Ghrelin, the hunger hormone, increases by 15 to 28% after just one night of poor sleep. If you are chronically sleep deprived, your hunger hormones may be overpowering semaglutide signaling.
Track your sleep for two weeks. If you are consistently getting less than seven hours or experiencing poor sleep quality (frequent waking, difficulty falling asleep, early morning awakening), addressing this may unlock the appetite suppression you have been waiting for.
Audit your diet composition
Are you eating enough protein? High protein intake (25 to 30 grams per meal minimum) triggers additional satiety hormones that work synergistically with semaglutide. If your meals are heavy on refined carbohydrates and light on protein and fiber, you are making appetite suppression harder than it needs to be.
Aim for 1.2 to 1.6 grams of protein per kilogram of body weight per day. Distribute it across meals. Include vegetables and whole grains for fiber. This dietary foundation amplifies semaglutide effects significantly.
Distinguish physical hunger from emotional eating
This is critical. Semaglutide targets physical hunger signals. It suppresses the hormonal and neural pathways that create the sensation of physiological hunger. But it cannot erase decades of emotional eating patterns, habitual eating, or eating triggered by boredom, stress, anxiety, or social situations.
If you find yourself eating despite not feeling physically hungry, semaglutide may actually be working perfectly. The medication has done its job by removing the physical hunger. What remains is behavioral, psychological, or emotional eating that requires different interventions, therapy, mindfulness, habit restructuring, or addressing underlying anxiety.
Talk to your prescriber about dose adjustment
If you have been through the full escalation to 2.4 mg, maintained that dose for at least four weeks, addressed sleep and diet and stress, and still experience minimal appetite suppression, you are in the minority but you are not alone. Some people genuinely need higher doses or different medications. The recently studied semaglutide 7.2 mg dose showed a 20.7% average weight reduction after 72 weeks in the STEP UP trial, significantly outperforming the 2.4 mg dose.
Alternatively, your prescriber may consider switching to tirzepatide, which targets both GLP-1 and GIP receptors and may produce stronger appetite suppression for some individuals. Or combining semaglutide with cagrilintide, an amylin receptor agonist that works through complementary pathways, as studied in the REDEFINE 1 trial showing over 20% weight loss in the majority of participants using the combination.
The clinical evidence on semaglutide appetite suppression
Let us get specific with the numbers. Vague claims do not help anyone. Here is exactly what the published research shows about semaglutide and appetite.
The Blundell 2017 crossover study
This is the most detailed study specifically measuring semaglutide appetite effects. Published by Blundell and colleagues, it was a 12-week, randomized, double-blind, placebo-controlled crossover trial. Thirty subjects with obesity (BMI 30 to 45) were randomized, and 28 completed both treatment periods.
Key findings:
Total daily ad libitum energy intake decreased by approximately 24% with semaglutide versus placebo (a reduction of 3,036 kJ per day)
Lunch meal intake decreased by approximately 35% (a reduction of 1,255 kJ)
Evening meal intake decreased by 753 kJ
Evening snack intake decreased by 1,028 kJ
Meal duration at lunch was reduced by 1.5 minutes
Fasting appetite suppression scores significantly improved
Subjects reported less hunger, fewer food cravings, and better control of eating
Preference for high-fat, non-sweet foods decreased significantly
Weight loss averaged 5.0 kg over 12 weeks (versus 1.0 kg weight gain on placebo)
Fat mass loss was three times greater than lean mass loss
Nausea ratings were similar between semaglutide and placebo groups, which is important. It means the appetite suppression was not just because people felt sick. The appetite reduction was genuine, driven by changes in hunger signaling and food reward, not nausea.
The STEP 1 trial
Published in the New England Journal of Medicine, STEP 1 enrolled 1,961 adults with BMI 30+ (or 27+ with at least one weight-related comorbidity). Participants received semaglutide 2.4 mg or placebo for 68 weeks alongside lifestyle intervention.
Results:
Average weight loss: 14.9% of body weight with semaglutide versus 2.4% with placebo
69% to 79% of participants achieved 10% or greater weight loss
Appetite suppression was a primary driver of weight loss
Improvements in all cardiometabolic risk factors
Semaglutide vs tirzepatide
Tirzepatide targets both GLP-1 and GIP receptors, creating a dual-action approach. In head-to-head comparison, tirzepatide tends to produce greater weight loss, with the SURMOUNT-1 trial showing up to 22.5% weight loss at the highest dose compared to semaglutide 14.9%. The tirzepatide dose escalation follows a similar gradual approach.
Semaglutide vs cagrilintide combination
The combination of cagrilintide and semaglutide (CagriSema) targets three pathways simultaneously. The REDEFINE 1 trial showed that over 20% of participants achieved more than 20% weight loss with the combination. Cagrilintide adds amylin-mediated satiety on top of semaglutide GLP-1 effects.
The role of food noise reduction
Appetite suppression is not just about reduced hunger. One of the most impactful effects of semaglutide is what patients call "food noise reduction," the silencing of constant thoughts about food.
For people who have never experienced food noise, this concept seems foreign. But for those who have struggled with weight, food noise is a constant companion. It is thinking about lunch before breakfast is over. It is walking through a store and being drawn to the snack aisle despite having no hunger. It is lying in bed at night running through what to eat tomorrow.
Semaglutide quiets this noise by changing the neural reward pathways that generate those thoughts. When GLP-1 receptors in the brain reward system are activated by semaglutide, the motivation to seek food-related rewards decreases. Food becomes less interesting at a subconscious level.
The food noise reduction typically begins around weeks four through eight, becomes clearly noticeable by weeks eight through twelve, and reaches its full extent at the maintenance dose.
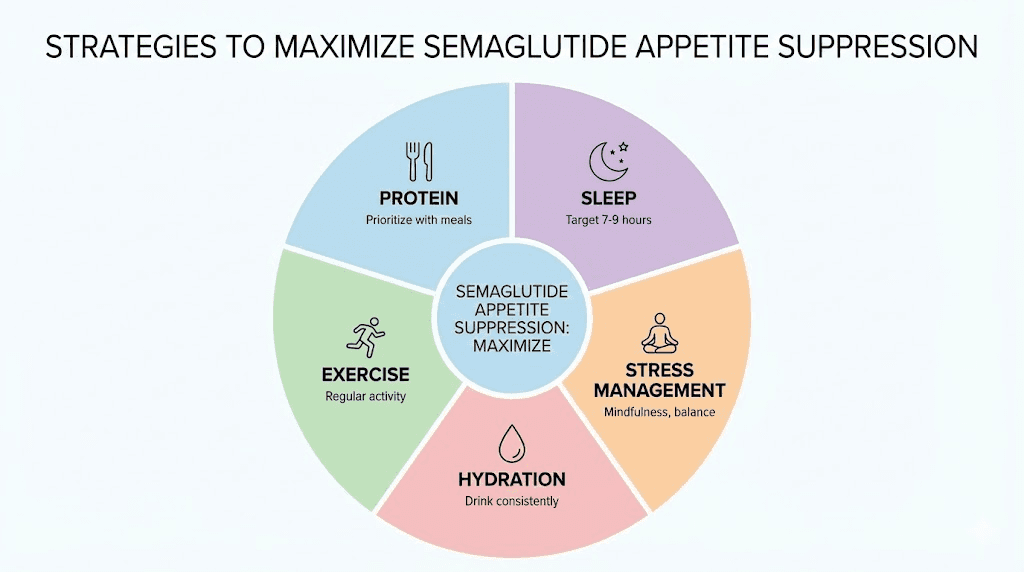
Maximizing semaglutide appetite suppression
You want the appetite suppression to be as strong and as fast as possible. These evidence-based strategies help.
Prioritize protein at every meal. Protein triggers satiety hormones PYY and CCK that work alongside semaglutide GLP-1 effects. Aim for 25 to 30 grams per meal. Choose high-quality protein sources.
Eat fiber-rich foods. Fiber slows gastric emptying further, compounding semaglutide effects and supporting gut health.
Stay hydrated. Drink 2 to 3 liters of water daily.
Optimize sleep. Seven to nine hours of quality sleep is non-negotiable. Sleep deprivation increases ghrelin by 15 to 28%.
Exercise consistently. Regular physical activity independently suppresses appetite and helps preserve muscle during weight loss.
Manage stress proactively. Chronic stress drives cortisol-mediated eating through pathways that semaglutide does not directly target.
Avoid liquid calories. Liquid calories pass through the stomach much faster than solid food, partially bypassing the gastric fullness mechanism.
Eat mindfully. Semaglutide enhances natural satiety signals, but you need to be present enough to notice them.
Common misconceptions about semaglutide appetite suppression
Myth: appetite suppression starts immediately. The drug needs to build up over weeks. Set your expectation for four to twelve weeks.
Myth: if you are hungry, semaglutide is not working. Semaglutide reduces hunger. It does not eliminate it.
Myth: nausea means it is working. Nausea ratings were similar between semaglutide and placebo groups. Nausea is a side effect, not a measure of efficacy.
Myth: you cannot overeat on semaglutide. You absolutely can. The medication is a powerful tool, not an impenetrable barrier. It works best when combined with conscious eating habits.
Long-term appetite patterns on semaglutide
Months 3 through 6: Peak appetite suppression for most people. Maximum fat loss.
Months 6 through 12: Appetite may return slightly as the body finds new equilibrium. Weight loss slows from about 2% to 1% per month.
Year 2+: Appetite suppression maintained at meaningful but less dramatic levels. The STEP extensions showed weight regain occurs if discontinued.
If you stop semaglutide: Appetite returns to near pre-treatment levels within weeks. The STEP 1 extension showed two-thirds of lost weight regained within a year. Planning for long-term use or maintaining weight loss habits is essential.
Compounded semaglutide considerations
Many people access semaglutide through compounding pharmacies. Dosing calculations require converting between milligrams and units, creating opportunities for error. Quality varies between pharmacies. The reconstitution process, proper storage, and correct reconstitution protocols are critical.
Use the SeekPeptides semaglutide dosage calculator to verify your dose calculations.
Special populations
Type 2 diabetes: Maximum Ozempic dose is 2.0 mg versus 2.4 mg for Wegovy. Blood sugar stabilization can independently reduce hunger spikes.
Women versus men: Women may notice appetite suppression varies with menstrual cycle. Menopausal women may experience complex interactions with metabolic changes.
Older adults: Maintaining adequate protein intake is especially important to prevent sarcopenia.
Related peptide protocols
Semaglutide belongs to the peptide class. The amylin receptor pathway represents a complementary approach. Cagrilintide targets hunger through different mechanisms. The CagriSema combination leverages both pathways.
For preserving muscle during weight loss, BPC-157 and TB-500 stacking supports tissue repair. MOTS-c improves mitochondrial function. IGF-1 LR3 supports anabolic signaling. The stacking approach addresses tissue repair, bone health, and longevity.
If using multiple peptides, understand how they interact. Consider storage, reconstitution, refrigeration, and injection technique. Use the SeekPeptides peptide stack calculator and reconstitution calculator.
The best peptide stacks for weight loss balance appetite management with muscle preservation and connective tissue support.
Getting started the right way
Establish baseline habits before your first injection. Start a regular exercise routine. Understand the dose escalation timeline. Source quality product from reputable sources. Use testing resources if working with compounded products. Understand proper storage and expiration. Find a qualified peptide therapy provider.
Frequently asked questions
How long does semaglutide take to reduce appetite on the first dose?
Some people notice subtle appetite reduction within the first one to four days. However, reliable appetite suppression typically develops over four to twelve weeks as the dose escalates and steady-state blood levels are reached.
Will I stop feeling hungry completely on semaglutide?
No. Semaglutide reduces the intensity and frequency of hunger, but it does not eliminate it. Complete absence of hunger would be medically concerning.
Why does my appetite come back before my next weekly injection?
Semaglutide blood levels fluctuate throughout the weekly dosing interval, peaking one to three days after injection and declining toward day seven.
Does semaglutide affect what foods I crave?
Yes. Clinical studies show reduced preference for high-fat, energy-dense foods. Many users report lean proteins and lighter options become more appealing.
Can I take anything to enhance semaglutide appetite suppression?
High-protein, high-fiber diet is the most evidence-based enhancement. Some researchers explore combinations with cagrilintide under medical supervision.
Is compounded semaglutide the same as Wegovy?
When compounded correctly, appetite suppression should be equivalent. Use reputable testing to verify potency if uncertain.
Does semaglutide appetite suppression wear off over time?
Most people maintain meaningful suppression long-term, but intensity may moderate after six to twelve months. Dose adjustments can help.
How is semaglutide different from stimulant diet pills?
Stimulants work fast but temporarily with tolerance and cardiovascular risks. Semaglutide works through natural GLP-1 pathways, develops gradually, and maintains effectiveness long-term.
External resources
For researchers serious about optimizing their peptide protocols and weight management strategies, SeekPeptides offers the most comprehensive resource available, with evidence-based guides, dosing calculators, proven protocols, and a community of thousands who have navigated these exact questions. SeekPeptides members access detailed appetite management strategies, dose optimization guidance, and expert-reviewed protocols that account for the individual factors most resources ignore.
In case I do not see you, good afternoon, good evening, and good night. May your appetite stay balanced, your doses stay accurate, and your progress stay consistent. Join us here.



