Feb 1, 2026
Three months of physical therapy. Two cortisone shots. Enough ibuprofen to fill a swimming pool. And your shoulder still screams every time you reach for a coffee mug on the top shelf. Sound familiar? You are not alone. Shoulder pain ranks among the most common musculoskeletal complaints worldwide, affecting roughly 18 to 26 percent of adults at any given time. The rotator cuff alone accounts for nearly 4.5 million physician visits each year in the United States. And here is what most people discover the hard way: conventional treatments often manage symptoms without addressing the underlying tissue damage that keeps the pain cycle spinning.
That is where peptides enter the conversation.
Not as a magic bullet. Not as a replacement for proper diagnosis or rehabilitation. But as a targeted biological tool that may accelerate the healing processes your body already uses, just not fast enough. Peptides like BPC-157, TB-500, and GHK-Cu have generated significant attention in the research community for their roles in tissue repair, inflammation reduction, and injury recovery. Preclinical studies show accelerated tendon healing, enhanced collagen synthesis, and improved biomechanical outcomes in animal models. Anecdotal reports from researchers and clinicians paint an even more compelling picture, with some describing dramatic improvements in shoulder function within weeks of starting protocols.
This guide covers everything you need to know about using peptides for shoulder pain. We will break down the specific peptides studied for shoulder conditions, the mechanisms behind how they work, practical protocol considerations, what the research actually says versus what is speculation, and how to combine peptide approaches with proper rehabilitation for the best possible outcomes. Whether you are dealing with a nagging rotator cuff issue, frozen shoulder, chronic tendinitis, or post-surgical recovery, understanding these biological tools could change your approach to healing entirely. SeekPeptides has compiled the most comprehensive research available on this topic, and what follows represents the current state of knowledge in this rapidly evolving field.
Understanding shoulder pain and why it resists treatment
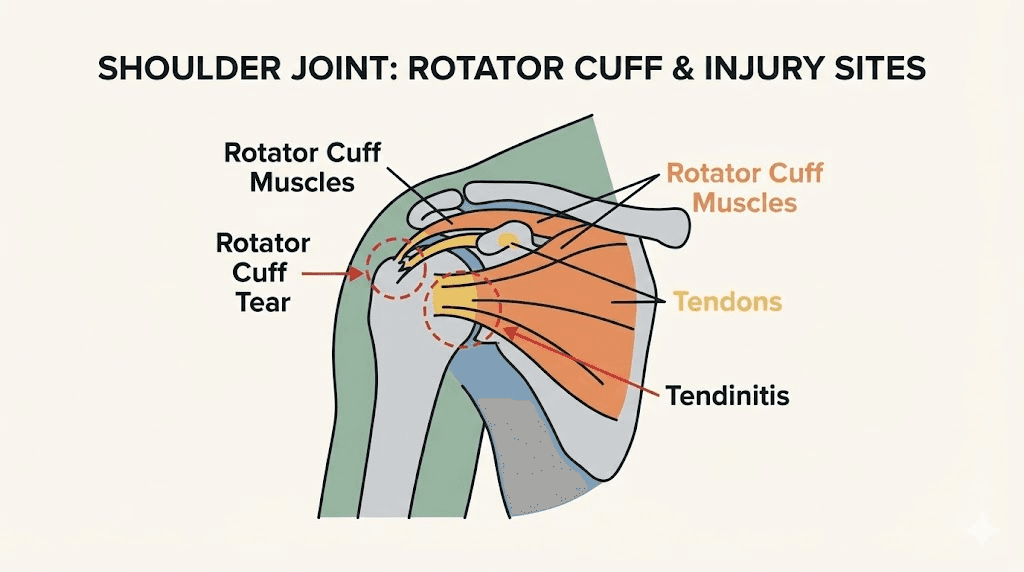
Before exploring peptide solutions, you need to understand what makes shoulder injuries so stubbornly persistent. The shoulder is the most mobile joint in the human body, and that mobility comes at a cost. The rotator cuff, a group of four muscles and their tendons that stabilize the shoulder joint, operates under enormous mechanical stress daily. Every time you lift, push, pull, or reach overhead, these tissues absorb force. Over time, or through acute injury, they break down.
The problem is blood supply.
Tendons receive significantly less blood flow than muscles. The supraspinatus tendon, the most commonly injured rotator cuff structure, has a particularly poor vascular zone near its insertion point on the humerus. This means healing materials, oxygen, nutrients, and growth factors delivered through blood struggle to reach the exact area where damage occurs. A muscle tear might heal in weeks. A tendon injury in the same shoulder can persist for months or years.
This vascular limitation explains why conventional treatments often fall short. Anti-inflammatory medications reduce pain signals but do not accelerate tissue repair. Cortisone injections suppress inflammation temporarily but may actually weaken tendon structure with repeated use. Physical therapy strengthens surrounding muscles and improves movement patterns, which is essential, but it cannot force poorly vascularized tissue to heal faster than biology allows. Even surgical repair of rotator cuff tears carries a retear rate between 20 and 94 percent depending on tear size and patient factors. The tissue itself often lacks the biological capacity to heal properly.
This is precisely the gap that peptides aim to fill. By promoting angiogenesis (new blood vessel formation), enhancing fibroblast activity, stimulating collagen synthesis, and modulating inflammation rather than simply suppressing it, specific peptides target the root biological limitations that make shoulder healing so difficult. They work with the body rather than merely masking symptoms.
Common shoulder conditions where peptides are being researched
Not all shoulder pain is created equal. The specific condition matters enormously when considering which peptides might be relevant and how they might help. Here are the primary shoulder conditions attracting peptide research attention:
Rotator cuff tendinopathy and partial tears. This covers the spectrum from chronic tendon degeneration to partial-thickness tears. The tendon tissue is damaged but not completely severed. These conditions respond poorly to rest alone because the underlying tissue quality has deteriorated. Peptides that promote tendon fibroblast activity and collagen reorganization are particularly relevant here. Research on BPC-157 shows enhanced tendon outgrowth and improved biomechanical strength in preclinical tendon models.
Full-thickness rotator cuff tears. Complete tears where the tendon has fully separated from bone. These typically require surgical repair, but the healing process after surgery is where peptides generate the most interest. The tendon-to-bone healing interface is notoriously weak, and retear rates remain high even after technically successful surgery. Growth hormone-releasing peptide 2 (GHRP-2) has shown reduced M1 macrophage polarization at the tendon-bone interface in rat models, potentially improving the healing environment after surgical repair.
Frozen shoulder (adhesive capsulitis). A condition where the shoulder capsule thickens and tightens, causing progressive pain and severe range-of-motion loss. Current treatments are largely palliative and do not address the underlying fibrosis. Relaxin-2, a peptide hormone, has demonstrated the ability to restore range of motion and eliminate capsular fibrosis in mouse models of shoulder arthrofibrosis, making it perhaps the most specifically relevant peptide for this condition.
Shoulder bursitis and impingement. Inflammation of the bursa or mechanical impingement of soft tissues during overhead movement. The anti-inflammatory properties of peptides like BPC-157 and TB-500 are relevant here, as reducing inflammation in the subacromial space can relieve impingement and allow proper tissue healing.
Post-surgical recovery. Whether after rotator cuff repair, labral repair, or shoulder replacement, the post-operative healing period is critical. Peptides that enhance tendon repair, reduce scar tissue formation, and improve overall tissue quality could theoretically improve surgical outcomes and reduce recovery time.
BPC-157: the most studied peptide for shoulder healing
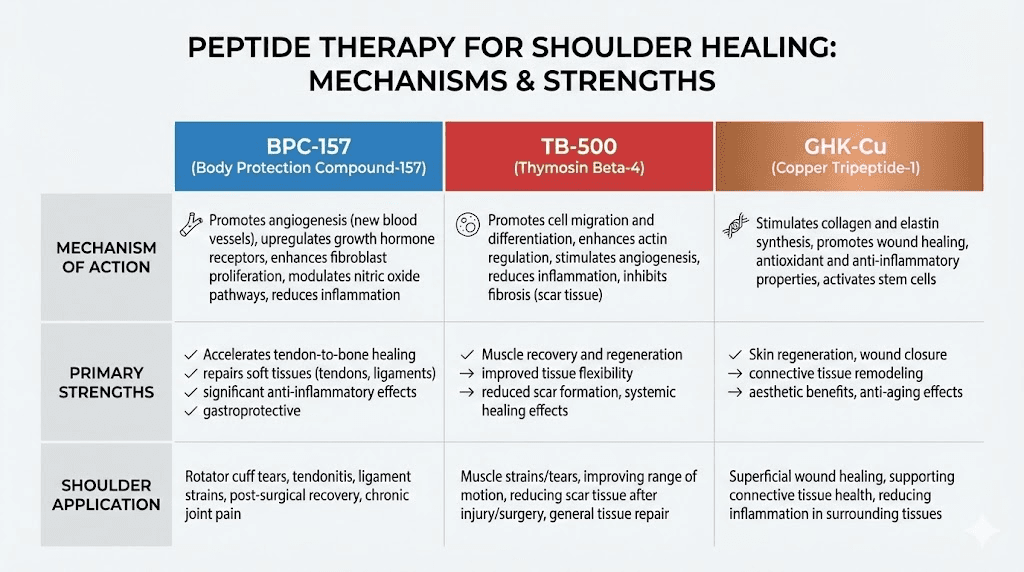
If you have spent any time researching peptides for injury recovery, you have encountered BPC-157. Body Protection Compound-157 is a synthetic pentadecapeptide, meaning it consists of 15 amino acids, derived from a protein naturally found in human gastric juice. Its stability distinguishes it from many naturally occurring peptides. It resists degradation in the acidic environment of the stomach and maintains biological activity across a range of conditions.
The research on BPC-157 for musculoskeletal healing is substantial by peptide standards. A systematic review published in orthopaedic sports medicine literature identified 36 studies from 1993 to 2024. Of those, 35 were preclinical (animal studies) and one was clinical (human). The preclinical evidence consistently shows enhanced healing across multiple tissue types relevant to shoulder injuries.
How BPC-157 works at the cellular level
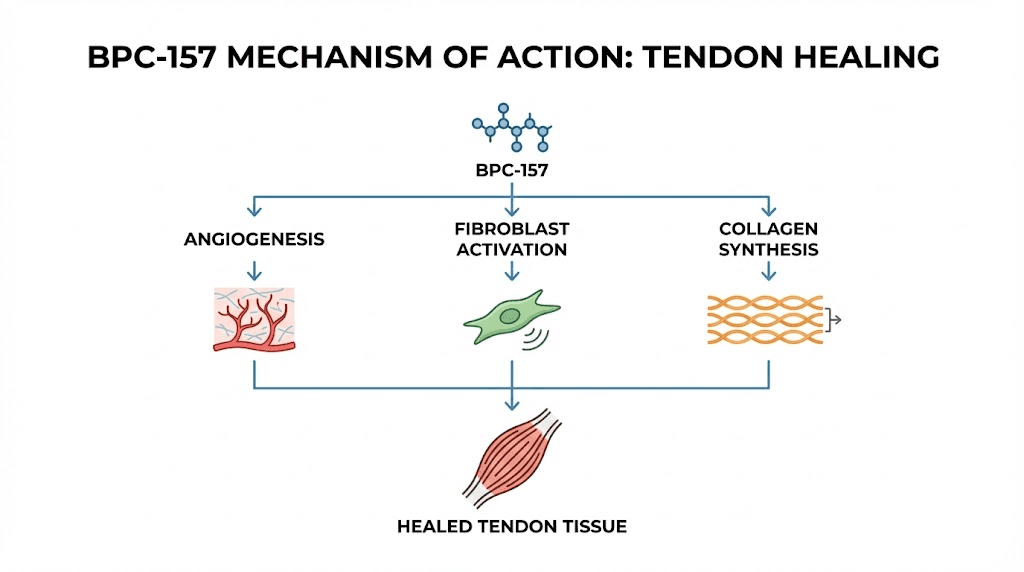
BPC-157 does not do one thing. It activates multiple overlapping pathways simultaneously, which is part of why its effects appear so broad. Understanding these mechanisms helps explain why it shows particular promise for shoulder conditions specifically.
Angiogenesis promotion. BPC-157 activates the VEGFR2 pathway and promotes nitric oxide synthesis via the Akt-eNOS axis. In practical terms, this means it stimulates the growth of new blood vessels. For shoulder tendons with poor vascular supply, this is potentially transformative. More blood vessels mean more oxygen, more nutrients, and more healing factors reaching damaged tissue. Studies in rats show increased blood vessel formation at injury sites treated with BPC-157 compared to controls.
Fibroblast activation. Fibroblasts are the cells responsible for producing collagen and other structural proteins in connective tissue. BPC-157 promotes the outgrowth of tendon fibroblasts from tendon explants, enhances cell survival under stress, and increases the migration of tendon fibroblasts to injury sites. This migration is mediated through the FAK-paxillin pathway, a signaling cascade that controls how cells move and attach to surrounding tissue. For a damaged rotator cuff tendon, more fibroblasts at the injury site means more raw material for tissue repair.
And it goes deeper than just attracting fibroblasts.
BPC-157 also increases the expression of growth hormone receptor in tendon fibroblasts at both the mRNA and protein levels. When growth hormone then interacts with these upregulated receptors, it produces a dose-dependent and time-dependent increase in cell proliferation. This means BPC-157 essentially makes tendon cells more responsive to the body natural growth signals, amplifying the healing response that already exists.
Anti-inflammatory modulation. Rather than simply suppressing inflammation like NSAIDs or cortisone, BPC-157 appears to modulate the inflammatory response. It reduces mononuclear inflammatory cell migration to injury sites while simultaneously promoting productive healing activity. This is a crucial distinction. Some inflammation is necessary for healing. The initial inflammatory response recruits repair cells and clears damaged tissue. But excessive or prolonged inflammation becomes destructive. BPC-157 seems to help the body find the productive middle ground. You can learn more about how different peptides interact with inflammatory pathways in our inflammation peptides guide.
Collagen and extracellular matrix support. In treated tendons, researchers observe formation of granulation tissue with active angiogenesis, increased reticulin fiber production, and organized collagen formation. The healed tendons in BPC-157-treated animals show increased load to failure and significantly higher functionality compared to untreated controls.
BPC-157 research specific to tendon injuries
The most directly relevant studies for shoulder pain involve BPC-157 effects on tendon tissue. Several key findings stand out.
In Achilles tendon transection models in rats, systemic BPC-157 administration via intraperitoneal injection produced significantly improved recovery compared to controls. The improvements were measurable both biochemically and through micro and macroscopic observation. Biomechanically, healed tendons showed increased load to failure, meaning they could withstand more force before breaking, and the Achilles Functional Index showed significantly higher functionality over 14 days.
Another study demonstrated that BPC-157 consistently enhanced healing even in severe injuries where soft tissues were inherently unable to heal on their own without intervention. This finding is particularly relevant for rotator cuff injuries, where the supraspinatus tendon often cannot bridge large gaps without assistance.
The peptide research literature also shows BPC-157 protecting the endothelium (blood vessel lining), which supports sustained blood flow to healing tissues. For a rotator cuff tendon sitting in a relatively avascular zone, maintaining whatever blood supply exists while building new vessels is critical. If you want to understand the broader science behind how peptides work, our foundational guide covers the key concepts.
BPC-157 protocol considerations for shoulder injuries
While no FDA-approved dosing exists for BPC-157, the research literature and clinical observations provide a framework that many practitioners reference. These are educational ranges based on available data, not medical recommendations.
Dosage ranges reported in literature:
Conservative start: 200 to 250 mcg daily, split into two doses of 100 to 125 mcg administered 12 hours apart
Standard protocol: 300 to 400 mcg daily, considered the optimal range for most healing applications based on clinical observations
Acute injury protocol: 400 to 500 mcg daily, split into two to three doses throughout the day
Weight-based considerations:
Under 150 pounds: 200 to 300 mcg daily
150 to 200 pounds: 300 to 400 mcg daily
Over 200 pounds: 400 to 500 mcg daily
Cycle length typically runs four to eight weeks, with some practitioners suggesting six to twelve weeks followed by a four to eight week break. For detailed BPC-157 dosing information, including reconstitution guidance, our dedicated guide walks through the calculations. You can also use the BPC-157 dosage calculator to determine precise amounts based on your vial concentration and target dose.
Injection site considerations for shoulder injuries. This is where shoulder-specific protocols differ from general BPC-157 use. Local injections near the injury site often produce faster results than systemic administration through abdominal subcutaneous injection. For shoulder conditions, some practitioners describe periarticular injections, meaning near but not directly into the joint. The subcutaneous tissue around the shoulder, in the deltoid region or near the specific area of pain, provides a closer delivery route to the target tissue. However, periarticular shoulder injections should only be performed with proper medical guidance. General subcutaneous injection at distant sites like the abdomen can still provide systemic benefits, just potentially with a slower onset for the specific shoulder condition.
Rotation of injection sites remains important regardless of location. Alternating between the abdomen, thigh, and upper arm areas prevents lipohypertrophy and maintains consistent absorption. You can learn more about injection technique and peptide injection best practices in our dedicated guide. For reconstitution instructions, we have a step-by-step walkthrough with proper bacteriostatic water preparation.
Expected timeline for BPC-157 shoulder healing
Based on the available literature and reported observations:
Days 3 to 5: Earliest reports of reduced inflammation and pain. Some users describe a subtle decrease in the constant ache that characterizes chronic shoulder conditions.
Weeks 1 to 2: More noticeable pain reduction and early improvements in range of motion. Tendon and ligament healing processes appear to accelerate during this window based on preclinical data.
Weeks 2 to 4: Significant functional improvements reported. One documented case described a researcher who, after 1.5 weeks, noticed dramatic improvement, and by week 4 could perform a kneeling-to-handstand transition without the shoulder pain that had previously made this impossible.
Weeks 4 to 8: Ongoing tissue remodeling and strengthening. This is where the quality of healed tissue matters. BPC-157-treated tendons show improved collagen organization and biomechanical strength at these timepoints in animal models.
Individual results vary enormously based on injury severity, overall health, compliance with rehabilitation, and other factors. These timelines represent a general pattern, not a guarantee. Understanding how long peptides take to work across different conditions provides useful context for setting realistic expectations.
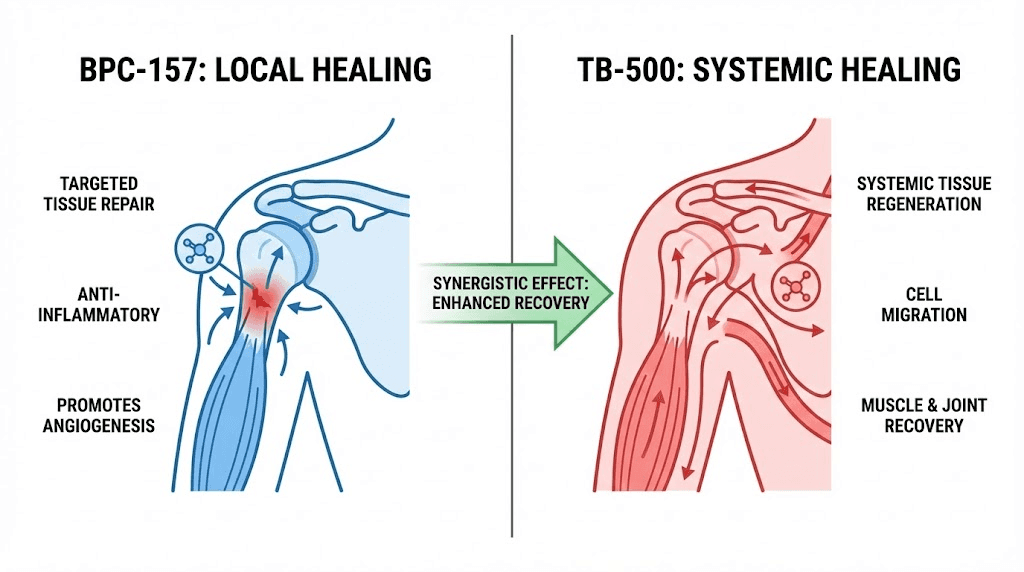
TB-500: systemic healing for shoulder recovery
While BPC-157 gets most of the attention, TB-500 (thymosin beta-4 acetate) brings a different and complementary set of mechanisms to shoulder healing. This synthetic 43-amino-acid peptide derives from thymosin beta-4, one of the most abundant intracellular proteins in mammalian cells. Where BPC-157 tends to work more locally at the site of injury, TB-500 operates systemically, traveling through the body to find and support areas that need repair.
How TB-500 supports shoulder healing
The primary mechanism of TB-500 involves actin sequestration. Actin is a fundamental structural protein in cells, critical for cell movement, tissue structure, and wound healing. When injury occurs, TB-500 sequesters actin at the injury site, triggering a cascade of repair signals. This actin management does several things simultaneously.
First, it promotes cell migration. Stem cells and progenitor cells need to physically move to the injury site before they can contribute to repair. TB-500 facilitates this migration by modulating the cytoskeletal dynamics that cells use to crawl through tissue. For a shoulder injury, this means repair cells arrive at the damaged tendon or capsule faster and in greater numbers.
Second, TB-500 promotes cell differentiation. Once repair cells reach the injury, they need to become the right type of cell. TB-500 signals these cells to differentiate into myocytes (muscle cells), epithelial cells, or connective tissue cells depending on what the local environment needs. For rotator cuff healing, this differentiation into appropriate connective tissue cells is essential.
Third, TB-500 reduces inflammation and promotes new blood vessel formation. In wound healing studies, rats treated with TB-500 showed 42 percent increased re-epithelialization over controls at four days and up to 61 percent at seven days. Treated wounds also showed increased collagen deposition and angiogenesis. These numbers matter because they suggest TB-500 meaningfully accelerates the fundamental processes of tissue repair. You can read more about TB-500 benefits across different applications in our detailed guide.
A significant advantage of TB-500 for shoulder injuries is its systemic distribution. Unlike some peptides that need to be injected near the injury site for maximum effect, TB-500 travels through the body to find damaged tissue. This means standard subcutaneous injection at any site can still deliver benefits to the shoulder. The peptide does not need to be injected into or near the shoulder joint itself.
TB-500 protocol considerations
Reported dosing in the research literature:
Starting dose: 500 mcg daily, subcutaneous injection
Titration: Increase by 100 to 150 mcg every two weeks as tolerated
Target dose: 750 to 1000 mcg daily by weeks five through twelve
Weekly total: Approximately 5 mg per week at full dose
Cycle length: Eight to twelve weeks, with optional extension to sixteen weeks
TB-500 is typically administered once daily via subcutaneous injection, with consistent timing and systematic site rotation. Storage requirements follow standard peptide protocols: lyophilized powder stored frozen, reconstituted solution refrigerated, and avoidance of freeze-thaw cycles. Our peptide storage guide covers these requirements in detail. For understanding how TB-500 compares to BPC-157 specifically, our BPC-157 vs TB-500 comparison breaks down the differences side by side.
The wolverine stack: combining BPC-157 and TB-500 for shoulder injuries
The combination of BPC-157 and TB-500, nicknamed the "wolverine stack" for its purported accelerated healing properties, represents the most discussed peptide approach for serious shoulder injuries. The logic behind this combination is straightforward. BPC-157 and TB-500 work through different mechanisms that complement each other rather than duplicating the same pathway.
BPC-157 focuses on local tissue repair. It promotes angiogenesis at the injury site, activates fibroblasts, enhances growth hormone receptor expression in tendon cells, and modulates inflammation. TB-500 works systemically. It facilitates cell migration to injury sites, promotes cell differentiation, supports actin-mediated tissue remodeling, and reduces scar tissue formation.
Together, the theory is that they create a more complete healing environment. BPC-157 optimizes conditions at the injury site while TB-500 ensures the right cells arrive in sufficient numbers and differentiate appropriately. Our comprehensive BPC-157 and TB-500 stacking guide covers the combination in depth.
Clinical observations with the combination
Practitioners have reported compelling cases with the BPC-157 and TB-500 combination for shoulder injuries. One documented case involved a 45-year-old tennis player with a partial rotator cuff tear who had found limited relief from traditional treatments. Within six weeks of starting a combined BPC-157 and TB-500 protocol, he reported significant pain reduction, improved range of motion, and a quicker return to daily activities.
Another case involved a former college athlete with severe shoulder arthritis who received TB-500 combined with A2M (alpha-2-macroglobulin) injections. After just two treatment sessions, he noted greater range of motion, reduced morning stiffness, and improved sleep quality.
A particularly striking anecdotal report comes from a practitioner who experienced rotator cuff injuries including frozen shoulder in both shoulders. Over 24 months, numerous conventional and alternative treatments provided inadequate relief. After starting BPC-157, within two weeks pain levels and overall function improved by an estimated 70 percent, enabling sleep without pain and significantly improved range of motion.
These reports are anecdotal and do not constitute clinical evidence. But the consistency of positive reports across different injury types and patient populations is notable. Understanding the wolverine stack approach helps contextualize how practitioners are combining these peptides. For information on combining peptides generally, our guide on cycling different peptides covers important considerations, and the peptide stack calculator can help with planning.
Wolverine stack protocol for shoulder injuries
Based on reported protocols in the literature:
BPC-157 component:
250 to 500 mcg daily, split into morning and evening doses
Subcutaneous injection, ideally near the shoulder (periarticular) with medical guidance, or abdomen/thigh for systemic delivery
TB-500 component:
750 to 2000 mcg twice weekly during loading phase (first two to four weeks)
500 to 1000 mcg twice weekly during maintenance phase
Subcutaneous injection at any standard site
Combined cycle:
Loading phase: four weeks
Maintenance: four to eight additional weeks
Total cycle: eight to twelve weeks
Rest period: four to six weeks between cycles if needed
For precise dosing calculations, the peptide calculator helps determine exact amounts based on your reconstitution volume and vial size. Understanding how to calculate peptide dosages is essential before starting any protocol. And proper mixing with bacteriostatic water ensures sterility and stability throughout the cycle.
GHK-Cu: the collagen builder for shoulder tissue repair
GHK-Cu (glycyl-L-histidyl-L-lysine copper complex) brings a different dimension to shoulder healing. While BPC-157 and TB-500 focus primarily on acute tissue repair signaling, GHK-Cu acts as a broad tissue remodeling agent that enhances collagen synthesis, reduces inflammation, and supports the long-term structural quality of healed tissue.
GHK-Cu occurs naturally in human plasma at approximately 200 ng/mL at age 20, declining to about 80 ng/mL by age 60. This decline correlates with the reduced regenerative capacity that comes with aging, which partly explains why shoulder injuries heal more slowly in older individuals. Supplementing with GHK-Cu may help restore some of that regenerative signaling.
GHK-Cu mechanisms relevant to shoulder healing
Collagen synthesis. GHK-Cu stimulates production of both Type I collagen (structural support) and Type III collagen (tissue flexibility and repair). Research indicates it can increase collagen production by up to 70 percent in laboratory studies. For shoulder tendons that need robust, properly organized collagen to regain strength, this is significant. The copper component serves as an essential cofactor for lysyl oxidase and lysyl hydroxylase, enzymes critical for proper collagen cross-linking. Without adequate copper, newly synthesized collagen remains weak. GHK-Cu provides both the signaling to produce more collagen and the mineral cofactor needed to make that collagen strong.
Tissue remodeling. GHK-Cu stimulates both synthesis and breakdown of collagen and glycosaminoglycans, and it modulates metalloproteinases and their inhibitors. This balanced approach to tissue remodeling is important for healing. You do not want only synthesis without clearing damaged tissue, and you do not want only breakdown without rebuilding. GHK-Cu appears to help coordinate both processes.
Gene expression modulation. Recent research reveals that GHK-Cu influences over 4,000 genes, many involved in tissue repair and regeneration. It activates genes associated with tissue remodeling while suppressing genes linked to inflammation and tissue breakdown. This broad gene-level effect suggests GHK-Cu may influence healing at a more fundamental level than peptides with narrower mechanisms. For details on how to use GHK-Cu injections, our guide covers technique and administration. The GHK-Cu dosage guide provides specific protocol information, and our injection dosage chart breaks down calculations by vial size.
Anti-inflammatory effects. GHK-Cu acts as a potent chemoattractant for mast cells and macrophages, which release proteins that stimulate tissue growth and repair. In diabetic wound models, GHK-Cu treatment promoted elevated levels of glutathione and ascorbic acid, improved epithelialization, and enhanced collagen synthesis. It also reduced TNF-alpha levels, a key inflammatory cytokine. These anti-inflammatory effects make GHK-Cu relevant not just for acute shoulder injuries but for chronic conditions like tendinopathy where ongoing low-grade inflammation contributes to tissue degeneration.
GHK-Cu for shoulder healing: combination approach
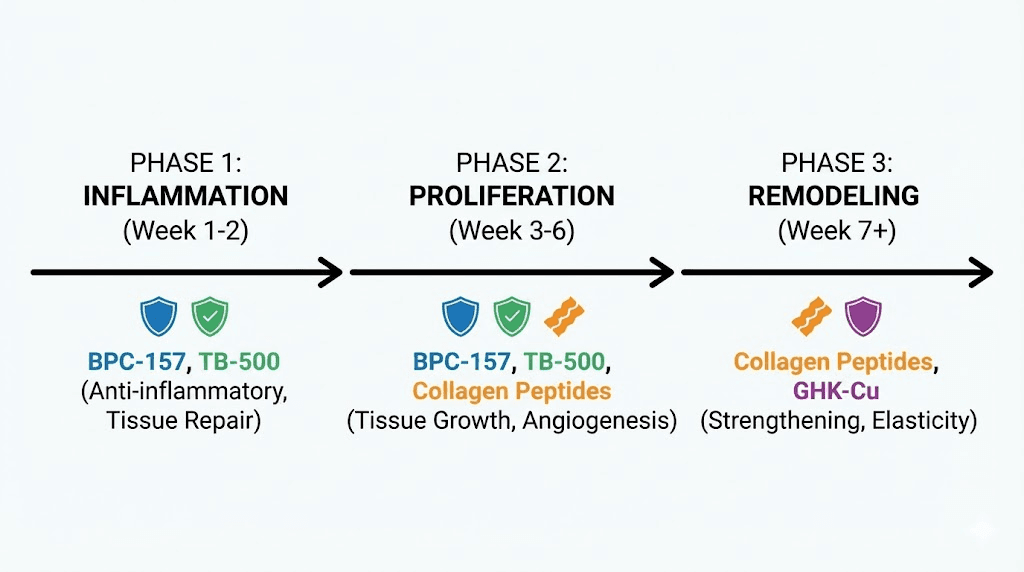
GHK-Cu is often discussed as a complement to BPC-157 rather than a standalone shoulder treatment. The reasoning: BPC-157 focuses on acute repair signaling and angiogenesis while GHK-Cu supports the quality and structure of the tissue being built. Think of BPC-157 as the contractor who organizes the repair crew and ensures materials arrive on site, and GHK-Cu as the quality control specialist who ensures the finished product is structurally sound.
In combination protocols, GHK-Cu is typically administered via subcutaneous injection at doses of 200 to 600 mcg daily. Some practitioners describe using it alongside a BPC-157/TB-500 stack during the later phases of healing when acute repair transitions to tissue remodeling and strengthening. Our peptide stacking guide covers the principles of combining multiple peptides effectively, including timing and sequencing considerations.
Other peptides relevant to shoulder conditions
Beyond the core three, several other peptides have research relevance to shoulder conditions. Some target the specific pathology of certain shoulder conditions more directly than the generalist healing peptides.
GHRP-2 for rotator cuff tendon-bone healing
Growth hormone-releasing peptide 2 has been studied specifically for tendon-bone interface healing in a rotator cuff tear model. A peer-reviewed study found that GHRP-2 reduced expression of Cd86, Nos2, and tnfa (all with statistical significance at P less than 0.01), suggesting inhibited M1 macrophage polarization. In the in vivo experiments, the proportion of M1 macrophages was reduced both two and four weeks after surgery at the tendon-bone interface.
Why does macrophage polarization matter for shoulder healing? M1 macrophages are pro-inflammatory, useful in the very early stages of healing for clearing debris but destructive if they persist. M2 macrophages are anti-inflammatory and pro-repair. By shifting the balance from M1 to M2, GHRP-2 may create a better healing environment at the critical tendon-bone junction. This is particularly relevant after rotator cuff repair surgery, where the quality of tendon-bone healing directly determines whether the repair holds or retears.
GHRP-2 also stimulates growth hormone release from the pituitary, providing systemic anabolic support for tissue repair. For researchers interested in growth hormone releasing peptides, understanding how they compare to other testosterone-supporting peptides and ipamorelin (another growth hormone secretagogue) provides useful context. Our ipamorelin vs CJC-1295 comparison explores the growth hormone peptide category further.
Relaxin-2 for frozen shoulder
Relaxin-2 is perhaps the most specifically targeted peptide for a shoulder condition. This 6 kDa peptide hormone, naturally upregulated during childbirth to soften the cervix, has been studied for adhesive capsulitis (frozen shoulder) because it directly targets fibrosis, the underlying cause of the condition.
In a mouse model of shoulder arthrofibrosis, multiple intraarticular injections of human relaxin-2 restored range of motion and eliminated capsular fibrosis. This is remarkable because current pharmacological treatments for frozen shoulder are entirely palliative. They manage pain and inflammation but do not reduce or eliminate the fibrous tissue buildup within the joint. Relaxin-2 appears to actually reverse the fibrotic process.
Relaxin-2 is still in early research stages and is not as widely available as BPC-157 or TB-500. However, its specificity for the fibrotic pathology of frozen shoulder makes it an important peptide to watch in this space.
CJC-1295 and ipamorelin for recovery support
While not directly targeting shoulder tissue, CJC-1295 and ipamorelin stimulate growth hormone release, which supports overall tissue repair and recovery. Some clinicians include these peptides in shoulder healing protocols to create a more anabolic systemic environment. Growth hormone enhances protein synthesis, supports connective tissue repair, and improves sleep quality, which is when the body does most of its healing work. The CJC-1295 dosage calculator can help with protocol planning.
KPV for inflammatory shoulder conditions
KPV peptide is a tripeptide derived from alpha-melanocyte-stimulating hormone with potent anti-inflammatory properties. For shoulder conditions driven primarily by inflammation, such as bursitis, acute tendinitis, or inflammatory arthropathy, KPV may provide targeted anti-inflammatory support without the tissue-weakening effects associated with corticosteroids. Our KPV peptide dosage guide covers protocol specifics.
Peptide comparison for shoulder conditions
Choosing the right peptide or combination depends on your specific shoulder condition, its severity, and your goals. Here is how the main options compare:
Peptide | Primary mechanism | Best for | Research level | Administration |
|---|---|---|---|---|
BPC-157 | Angiogenesis, fibroblast activation, growth hormone receptor upregulation | Tendinopathy, partial tears, post-surgical healing | 35+ preclinical studies, 1 clinical | Subcutaneous, local preferred |
TB-500 | Cell migration, differentiation, actin sequestration | Broad tissue repair, muscle and tendon injuries | Multiple preclinical, limited clinical | Subcutaneous, systemic effective |
GHK-Cu | Collagen synthesis, gene modulation, tissue remodeling | Chronic tendinopathy, tissue quality improvement | Extensive preclinical, in vitro | Subcutaneous injection |
GHRP-2 | M1/M2 macrophage shift, growth hormone release | Post-surgical tendon-bone healing | Specific RCT model study | Subcutaneous injection |
Relaxin-2 | Anti-fibrotic, capsule softening | Frozen shoulder specifically | Mouse model (PNAS published) | Intraarticular injection |
KPV | Anti-inflammatory (alpha-MSH derived) | Inflammatory shoulder conditions | Multiple preclinical | Subcutaneous injection |
For most shoulder injuries involving tendon damage, the BPC-157 and TB-500 combination represents the most researched approach. Adding GHK-Cu during the remodeling phase may improve the structural quality of healed tissue. For frozen shoulder specifically, relaxin-2 targets the actual pathology more directly than any other peptide, though availability remains limited. If you are exploring which peptides to combine and how many you can use simultaneously, our guide on how many peptides you can take at once addresses this question directly.
Protocols by shoulder condition
Different shoulder problems require different approaches. Here are condition-specific considerations based on the available research and reported clinical observations.
Protocol approach: rotator cuff tendinopathy
Goal: Reduce pain, improve tendon quality, restore function
Peptide approach:
BPC-157: 250 to 500 mcg daily, split morning and evening. Local subcutaneous injection near the shoulder if possible, otherwise systemic
Optional TB-500: 500 to 750 mcg twice weekly for systemic support
Optional GHK-Cu: 200 to 400 mcg daily, added from week three onward for collagen quality
Duration: Eight to twelve weeks
Critical addition: Physical therapy and progressive loading. Peptides may improve tissue quality, but the tendon needs mechanical stimulus to organize collagen fibers properly. Eccentric loading exercises are particularly important for tendinopathy. Without rehabilitation, peptides alone are unlikely to produce lasting structural improvement.
Expected progression:
Weeks one to two: Pain reduction, improved sleep (if night pain present)
Weeks three to four: Increased range of motion, tolerance of rehab exercises improves
Weeks five to eight: Significant functional improvement, return to activities
Weeks eight to twelve: Continued tissue remodeling and strengthening
For more on the general approach to peptides for joint pain, our dedicated guide covers the full landscape of options.
Protocol approach: partial rotator cuff tear
Goal: Promote tissue healing, prevent tear progression, avoid surgery if possible
Peptide approach:
BPC-157: 300 to 500 mcg daily, split doses, local injection near shoulder preferred
TB-500: 750 to 1000 mcg twice weekly (loading phase first four weeks), then 500 mcg twice weekly
GHK-Cu: 300 to 600 mcg daily from week two onward
Duration: Twelve weeks minimum
Critical notes: Partial tears require imaging to determine severity and location. Not all partial tears heal conservatively, and some will progress to full tears requiring surgical intervention. Peptides should complement, not replace, proper orthopedic evaluation and monitoring. Follow-up imaging at six to twelve weeks can help assess whether conservative management is working. For understanding the best peptides for tendon repair broadly, our guide covers the full evidence base.
Protocol approach: frozen shoulder (adhesive capsulitis)
Goal: Reduce capsular fibrosis, restore range of motion, manage pain
Peptide approach:
BPC-157: 300 to 500 mcg daily for anti-inflammatory and tissue healing properties
TB-500: 500 to 750 mcg twice weekly for systemic anti-inflammatory and tissue remodeling
Note on relaxin-2: While the most specifically targeted peptide for this condition, it remains largely in the research phase and is not widely available through standard channels
Duration: Twelve to sixteen weeks (frozen shoulder has a prolonged natural course)
Critical addition: Aggressive physical therapy within pain tolerance. Range-of-motion exercises, joint mobilization, and progressive stretching are essential. Frozen shoulder can be self-limiting (resolving on its own over one to three years), but this natural resolution is slow and often incomplete. The goal with peptides is to accelerate the resolution and improve the final outcome.
Protocol approach: post-surgical shoulder recovery
Goal: Accelerate healing, reduce retear risk, optimize tissue quality
Peptide approach:
BPC-157: 300 to 500 mcg daily, starting as soon as cleared by surgeon (typically one to two weeks post-op)
TB-500: 750 to 1000 mcg twice weekly
GHK-Cu: 200 to 400 mcg daily from week three to four post-op
Duration: Eight to sixteen weeks, aligned with surgical recovery timeline
Critical notes: Any peptide use after surgery should be discussed with and approved by the operating surgeon. Some surgeons are incorporating peptide protocols into their post-operative care plans. Others may have concerns about potential effects on healing. Transparency with your surgical team is essential. The fast injury healing resource page provides additional context on recovery optimization.
The role of rehabilitation alongside peptide protocols
This point cannot be emphasized enough. No peptide can replace proper rehabilitation.
Peptides may accelerate tissue healing. They may improve the quality of repaired tissue. They may reduce pain and inflammation that limit your ability to participate in therapy. But they cannot address the movement dysfunction, muscle weakness, compensatory patterns, and proprioceptive deficits that develop alongside shoulder injuries.
Think of it this way. If a building foundation is cracked, you can use the best concrete repair material available. But if the building above is structurally unsound with shifted loads and weakened supports, fixing the foundation alone will not prevent future problems. You need both: the repair material and the structural rehabilitation.
For shoulder injuries specifically, rehabilitation addresses:
Scapular mechanics. The shoulder blade provides the stable base from which the rotator cuff operates. Altered scapular movement patterns are present in virtually all chronic shoulder conditions and must be corrected for lasting improvement. No peptide addresses scapular dyskinesis.
Rotator cuff strength and balance. The four rotator cuff muscles must work in proper coordination to center the humeral head in the glenoid during movement. Weakness or imbalance creates impingement, abnormal tendon loading, and continued tissue damage. Progressive strengthening with proper form is essential. The combination of strengthening exercises with peptide-supported tissue healing may be synergistic, with better tissue quality enabling more productive training and better training providing the mechanical signals needed for optimal tissue organization.
Posterior capsule flexibility. Tightness in the posterior shoulder capsule is a common and underappreciated contributor to shoulder pain. It alters glenohumeral kinematics and creates impingement. Targeted stretching and manual therapy address this directly.
Kinetic chain integration. Shoulder function depends on the entire kinetic chain from the ground up. Core stability, thoracic spine mobility, and lower extremity strength all influence shoulder mechanics. A comprehensive rehabilitation program addresses the full chain.
The ideal approach combines peptide support for tissue biology with rehabilitation for mechanical function. Neither alone is as effective as both together. Many SeekPeptides members report that their biggest breakthroughs come when they combine proper protocols with consistent, progressive rehabilitation programs.
Practical considerations and potential pitfalls
Quality and sourcing
The peptide market includes everything from pharmaceutical-grade products to questionable compounds of uncertain purity and potency. For shoulder healing, where you are relying on specific biological activity, product quality matters enormously. Contaminated, degraded, or underdosed peptides will not produce the effects described in the research literature.
Key quality indicators to look for:
Third-party testing: Certificate of analysis (COA) from an independent laboratory showing purity (ideally above 98 percent), identity, and absence of contaminants
Proper storage during shipping: Lyophilized peptides are relatively stable, but improper handling can still degrade them
Transparent sourcing: Reputable suppliers provide information about their manufacturing process and quality control
Our peptide testing labs guide covers how to evaluate quality, and the best peptide vendors guide discusses sourcing considerations. Understanding research grade vs pharmaceutical grade peptides helps set appropriate quality expectations.
Reconstitution and storage
Proper handling is non-negotiable. Peptides degrade with improper storage, contaminated reconstitution water, and repeated freeze-thaw cycles. For a multi-week shoulder healing protocol, maintaining peptide integrity throughout is essential.
Use bacteriostatic water for reconstitution, not sterile water, because the benzyl alcohol preservative in bacteriostatic water inhibits microbial growth in the vial throughout the usage period. The peptide reconstitution calculator helps determine the correct water volume for your desired concentration. Once reconstituted, store in the refrigerator and use within the recommended timeframe. Our guides on how long reconstituted peptides last in the fridge and peptide fridge storage duration provide specific timelines.
What peptides cannot do for shoulder injuries
Honest expectations prevent disappointment and dangerous self-treatment. Peptides cannot:
Reattach a completely torn tendon. A full-thickness rotator cuff tear where the tendon has retracted from the bone typically requires surgical reattachment. Peptides may support healing after surgery, but they cannot bridge a structural gap that no longer has tissue continuity. Imaging is essential to determine tear extent before pursuing conservative treatment.
Fix labral tears. The labrum has extremely limited blood supply and healing capacity. Significant labral tears usually require surgical repair. Peptides like BPC-157 promote angiogenesis, which theoretically could support minor labral healing, but large tears are beyond what non-surgical approaches can address.
Reverse severe arthritis. Once cartilage is significantly eroded and bony changes have occurred, peptides cannot regenerate the joint surface. They may help with pain management and slow further degeneration, but they cannot rebuild a destroyed joint. For information on peptides and bone and cartilage repair, our guide covers what the research shows.
Replace proper diagnosis. Shoulder pain has many causes, including referred pain from the cervical spine, thoracic outlet syndrome, and cardiac conditions (especially left shoulder pain). Using peptides without a proper diagnosis risks treating the wrong problem while a serious underlying condition goes unaddressed.
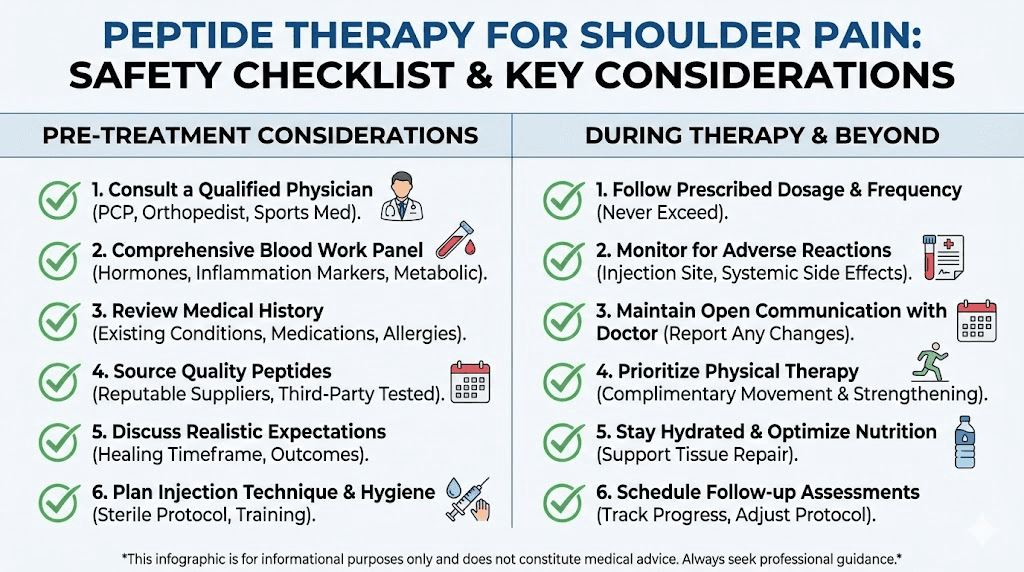
Safety considerations
BPC-157, TB-500, and GHK-Cu are not FDA-approved for human use. The FDA classified BPC-157 as a Category 2 bulk drug substance in 2023, meaning it cannot be compounded by commercial pharmaceutical companies and there is insufficient evidence regarding potential human harm. Both BPC-157 and TB-500 are prohibited by the World Anti-Doping Agency. Our BPC-157 legal status guide covers the regulatory landscape.
Preclinical studies have not identified toxic doses or lethal doses for BPC-157, and researchers reported no teratogenic, genotoxic, anaphylactic, or local toxic effects. However, the absence of adverse effects in animal studies does not guarantee safety in humans. Only three pilot studies have examined BPC-157 in humans, and long-term safety data does not exist. Our peptide safety and risks guide provides a thorough discussion of what is known and what remains unknown. Understanding the legal status of peptides in your jurisdiction is also important before considering any protocol.
Commonly reported side effects from peptide use include mild injection site reactions (redness, discomfort), temporary fatigue, headache, and occasional nausea. These are generally mild and transient. Serious adverse events have not been widely reported in the community, but the lack of long-term safety data means unknown risks may exist. Always consult a qualified healthcare provider before starting any peptide protocol.
Complementary approaches that support peptide protocols
Peptides do not operate in isolation. The biological environment in which they work dramatically affects their effectiveness. Several complementary approaches can create better conditions for peptide-supported healing.
Nutrition for tendon and tissue repair
Tendon healing requires adequate building materials. Without proper nutritional support, even the strongest healing signals from peptides have limited raw material to work with.
Protein and amino acids. Tendons are primarily collagen, which requires adequate protein intake to build. Research suggests at least 1.2 to 1.6 grams of protein per kilogram of body weight daily during injury recovery. Glycine and proline, key amino acids in collagen, can be supplemented through bone broth or collagen peptides.
Vitamin C. Essential cofactor for collagen synthesis. Without adequate vitamin C, the body cannot produce properly structured collagen regardless of how many peptide signals tell it to. Some research protocols include 500 to 1000 mg of vitamin C taken 30 to 60 minutes before exercise or peptide administration. Our guide on vitamin C and peptides explores this interaction in depth.
Zinc and copper. Both minerals serve as cofactors for enzymes involved in tissue repair. Copper is particularly relevant given its role in collagen cross-linking, which is partly why GHK-Cu (a copper-carrying peptide) is relevant to tissue repair.
Omega-3 fatty acids. Help modulate inflammation and support tissue healing. Anti-inflammatory nutrition complements the anti-inflammatory effects of peptides like BPC-157 and KPV.
Sleep optimization
Growth hormone, which plays a critical role in tissue repair, is released primarily during deep sleep. Poor sleep directly impairs the healing capacity of all tissues, including shoulder tendons. Peptides like DSIP (delta sleep-inducing peptide) and pinealon have been studied for sleep improvement, though they are not specifically shoulder-related. The connection between sleep quality and shoulder pain is bidirectional: shoulder pain disrupts sleep, and poor sleep impairs healing. Breaking this cycle is often a priority in shoulder recovery. SeekPeptides members frequently discuss sleep optimization strategies in the context of recovery protocols.
Stress management
Chronic stress elevates cortisol, which suppresses tissue repair and promotes catabolism. High cortisol levels directly antagonize the anabolic healing processes that peptides are trying to promote. Managing stress through whatever methods work for you, whether meditation, exercise, social connection, or professional support, creates a more favorable healing environment.
PRP and other regenerative therapies
Platelet-rich plasma (PRP) therapy, where concentrated platelets from your own blood are injected into the injury site, has more clinical evidence for shoulder conditions than most peptide therapies. Some practitioners combine PRP with peptides for potentially synergistic effects. A study examining PRP combined with self-assembled peptides on rotator cuff tears in rats found enhanced collagen arrangement, inhibited inflammatory changes, and reduced apoptosis compared to PRP alone. CJC-1295 with ipamorelin is sometimes used to stimulate stem cell activity before procedures, potentially enhancing the regenerative capacity of PRP and similar treatments.
Peptides vs conventional treatments: a realistic comparison
It is tempting to position peptides as superior to conventional shoulder treatments. But an honest assessment requires nuance.
Physical therapy has the strongest evidence base for most shoulder conditions. Systematic reviews consistently show it improves outcomes for rotator cuff tendinopathy, frozen shoulder, and post-surgical recovery. Peptides do not have equivalent human evidence. However, peptides may enhance the biological healing that makes physical therapy more productive. The two approaches are complementary, not competing.
Corticosteroid injections provide rapid pain relief and can break pain cycles that prevent rehabilitation. But repeated cortisone injections may weaken tendon tissue over time. Peptides offer a theoretically different approach: addressing tissue biology rather than just inflammation. For acute pain crises, cortisone may still be the pragmatic choice. For chronic conditions where tissue quality matters, peptides offer a biologically different strategy.
NSAIDs manage pain effectively but do not promote healing and may actually impair tendon repair when used long-term. Peptides with anti-inflammatory properties (BPC-157, KPV, TB-500) modulate rather than suppress inflammation, which may preserve the healing-promoting aspects of the inflammatory response while reducing its destructive elements.
Surgery remains necessary for many shoulder conditions: full-thickness rotator cuff tears, unstable shoulder dislocations, significant labral tears. Peptides cannot replace surgical intervention when structural repair is needed. But they may improve healing after surgery, potentially reducing retear rates and accelerating functional recovery.
PRP therapy has more human clinical data than most peptide therapies for shoulder conditions. It represents a more established regenerative option. However, peptide therapy offers the advantage of extended treatment duration (daily dosing over weeks) versus the single or limited injection approach of PRP. Some evidence suggests combining the two approaches may be superior to either alone.
For researchers comparing different therapeutic approaches, understanding the distinction between injectable vs oral peptide administration is relevant. Some BPC-157 users opt for oral administration, though injectable forms are generally considered to provide more predictable results for localized injuries like shoulder conditions. You can also explore the broader landscape of BPC-157 alternatives and TB-500 alternatives to understand the full range of options available.
Common mistakes when using peptides for shoulder pain
Based on community reports and clinical observations, these are the most frequent errors people make when attempting peptide-based shoulder healing protocols.
Mistake 1: skipping proper diagnosis
Shoulder pain has dozens of potential causes. Rotator cuff tendinopathy, labral tears, biceps tendon pathology, acromioclavicular joint dysfunction, cervical radiculopathy, thoracic outlet syndrome, and even cardiac conditions can all present as shoulder pain. Using peptides without knowing what you are treating is like putting premium fuel in a car with a flat tire. You might have the right supplement, but you are addressing the wrong problem. Get imaging. Get a proper examination. Know what you are dealing with before choosing a treatment approach.
Mistake 2: using peptides as a substitute for rehabilitation
We have covered this, but it bears repeating. The most common complaint from people disappointed with peptide results is that they expected peptides alone to solve the problem. Healing tissue still needs proper mechanical loading to organize correctly. Muscles still need strengthening. Movement patterns still need correction. Peptides optimize the biological side of healing. Rehabilitation optimizes the mechanical side. You need both. Our common peptide mistakes guide covers additional pitfalls to avoid.
Mistake 3: inadequate protocol duration
Tendon healing is slow. Even with peptide support, meaningful structural improvement in shoulder tendons takes weeks to months. People who use peptides for two weeks, feel some pain relief, and stop often find the pain returns because the underlying tissue has not had time to fully remodel. Four to eight weeks is a minimum for most shoulder conditions, with twelve weeks or more being appropriate for significant tears or chronic tendinopathy. Understanding the peptide cycle planning process helps set appropriate durations.
Mistake 4: poor injection technique
Contamination, incorrect injection depth, failure to rotate sites, and improper reconstitution all reduce effectiveness and increase risk. Subcutaneous injection is a skill that improves with practice and proper instruction. Using the correct needle gauge (25 to 27 gauge for subcutaneous), proper angle (45 to 90 degrees), and sterile technique throughout is non-negotiable. The getting started with peptides guide covers fundamental technique, and our peptide injection overview explains the process in detail.
Mistake 5: unrealistic expectations
Peptides are biological tools, not miracles. A severely degenerated rotator cuff in a 65-year-old with decades of wear will not become a healthy 25-year-old tendon. A massive full-thickness tear will not spontaneously heal without surgical repair. Peptides work within the constraints of biology. They optimize healing, they do not transcend it. Setting realistic expectations based on your specific condition, age, overall health, and injury severity leads to better decision-making and less disappointment.
Mistake 6: ignoring product quality
The peptide market ranges from pharmaceutical-grade products to potentially dangerous counterfeits. Using cheap, untested peptides to save money on a shoulder healing protocol is a false economy. If the peptide is degraded, contaminated, or underdosed, you get none of the benefits while potentially introducing harmful substances. The peptide vial research guide helps you evaluate what you are purchasing.
The current state of evidence: what we know and what we do not
Intellectual honesty requires acknowledging the limitations of current peptide research for shoulder conditions.
What the evidence supports:
BPC-157 consistently improves tendon healing outcomes in animal models across multiple tissue types and injury models
TB-500 accelerates wound healing and tissue repair in preclinical studies with measurable improvements in re-epithelialization, collagen deposition, and angiogenesis
GHK-Cu enhances collagen synthesis and modulates thousands of genes involved in tissue repair
GHRP-2 shifts macrophage polarization favorably in a rotator cuff tear model
Relaxin-2 eliminates capsular fibrosis in a frozen shoulder mouse model
No significant toxicity has been identified in preclinical BPC-157 studies
What remains uncertain:
Whether animal study results translate to equivalent human outcomes for shoulder conditions specifically
Optimal dosing for human shoulder injuries (all protocols are extrapolated from animal data and clinical observation)
Long-term safety with repeated use
Whether peptides meaningfully reduce rotator cuff retear rates after surgical repair in humans
How peptide therapy compares to established treatments like PRP in controlled human studies
Potential interactions with medications commonly used by shoulder pain patients
What we need:
Randomized controlled trials of BPC-157 and TB-500 for specific shoulder conditions in humans
Head-to-head comparisons of peptide therapy versus established treatments
Long-term safety data from monitored human use
Standardized dosing protocols based on human pharmacokinetic data
Studies combining peptides with rehabilitation to assess synergistic effects
The preclinical evidence is compelling. The anecdotal reports are consistently positive. But the gap between animal studies and proven human treatments remains real. People choosing peptide protocols for shoulder conditions are making informed decisions based on incomplete evidence, which is worth acknowledging honestly. For those interested in diving deeper into the research, our peptide research and studies compilation provides direct links to key papers.
Building your shoulder healing protocol: a practical framework
If you are considering peptides for shoulder pain after consulting with a qualified healthcare provider, here is a structured framework for thinking through the process.
Step 1: Get a proper diagnosis. Know exactly what is causing your shoulder pain. MRI imaging is the gold standard for soft tissue shoulder pathology. X-rays for bony changes. Physical examination for functional assessment. Without a diagnosis, you are guessing.
Step 2: Determine if peptides are appropriate. Not every shoulder condition is a good candidate. Inflammatory conditions, tendinopathy, partial tears, and post-surgical recovery are the strongest cases based on available research. Full-thickness tears requiring surgical repair need surgery first. Referred pain from the neck needs cervical treatment.
Step 3: Select your peptide approach. Based on your specific condition, choose from the options discussed in this guide. Most people start with BPC-157 alone or the BPC-157/TB-500 combination. Adding GHK-Cu during the remodeling phase is optional and more relevant for chronic conditions where tissue quality has deteriorated.
Step 4: Source quality products. Verify third-party testing, proper storage, and reputable sourcing. The peptide testing labs guide helps with evaluation.
Step 5: Plan your protocol. Determine dosing, cycle length, injection schedule, and reconstitution plan before starting. The peptide calculator and reconstitution calculator help with the math. Planning how you will mix your peptides with water and store them ensures consistency throughout the cycle. Review the peptide dosing guide for general principles, and the peptide dosage chart for quick reference.
Step 6: Start rehabilitation simultaneously. Do not wait for peptides to do their thing before starting physical therapy. Begin both together. The peptide-supported improvement in tissue biology makes rehabilitation more productive from day one.
Step 7: Monitor and adjust. Track pain levels, range of motion, functional capacity, and sleep quality throughout. If no improvement is evident by weeks three to four, reassess. The condition may need a different approach, the dose may need adjustment, or the product quality may be questionable.
Step 8: Plan your transition. As the peptide cycle ends, ensure your rehabilitation program is progressing to maintain and build on gains. The tissue improvements peptides support need to be reinforced with ongoing mechanical loading and proper movement patterns. SeekPeptides members get access to comprehensive protocol builders and expert guidance that account for these transition phases.
Frequently asked questions
Can peptides heal a torn rotator cuff without surgery?
For partial-thickness tears, peptides like BPC-157 may support tissue healing based on preclinical evidence showing enhanced tendon repair. However, full-thickness tears where the tendon has completely detached from bone typically require surgical reattachment. Peptides cannot bridge a structural gap without tissue continuity. Even for partial tears, proper rehabilitation is essential alongside any peptide protocol, and imaging follow-up helps determine whether conservative management is working.
How long does it take for peptides to help with shoulder pain?
Based on reported observations, initial pain reduction may be noticeable within the first one to two weeks. More substantial functional improvements typically occur between weeks three and six. Full tissue remodeling continues for eight to twelve weeks or longer. The timeline varies significantly based on injury severity, peptide protocol, rehabilitation compliance, and individual healing capacity. Our guide on how long peptides take to work provides more detailed timelines across conditions.
Should I inject BPC-157 directly into my shoulder?
Periarticular injection (near but not into the joint) near the shoulder injury site may produce faster localized effects than distant subcutaneous injection. However, shoulder injections should be performed with proper medical guidance due to the complex anatomy. Many users achieve results with standard subcutaneous injection at other sites (abdomen, thigh) which provides systemic distribution. For injection technique guidance, our peptide injection guide covers proper technique.
Can I use peptides after rotator cuff surgery?
Some practitioners are incorporating peptide protocols into post-surgical recovery plans to support tendon-bone healing and reduce retear risk. However, any post-surgical peptide use should be discussed with and approved by your operating surgeon. Starting too early could theoretically interfere with the natural healing cascade, though preclinical data generally suggests BPC-157 supports rather than disrupts normal healing processes. The fast injury healing resource provides additional recovery context.
Are peptides better than cortisone injections for shoulder pain?
They serve different purposes. Cortisone provides rapid anti-inflammatory relief and can break pain cycles. Peptides theoretically promote tissue repair rather than just symptom management. Cortisone has more human clinical evidence. Peptides have more compelling biological mechanisms but limited human data. For acute pain crises, cortisone may be more practical. For chronic conditions where tissue quality matters, peptides offer a different biological approach. They are not necessarily better or worse, just different tools for different aspects of the problem.
What is the best peptide stack for shoulder injuries?
The most commonly discussed combination for shoulder injuries is BPC-157 (250 to 500 mcg daily) plus TB-500 (750 to 1000 mcg twice weekly), sometimes called the wolverine stack. Adding GHK-Cu (200 to 400 mcg daily) from week three onward provides additional collagen synthesis support. The peptide stack calculator helps with planning multi-peptide protocols, and our stacking guide covers the principles of combining peptides effectively.
Do peptides work for frozen shoulder?
BPC-157 and TB-500 may provide anti-inflammatory and tissue healing support for frozen shoulder. However, relaxin-2 is the most specifically targeted peptide for adhesive capsulitis, as it directly addresses the capsular fibrosis that causes the condition. Relaxin-2 eliminated capsular fibrosis in a mouse model but remains in early research stages. Regardless of peptide use, aggressive physical therapy within pain tolerance remains the cornerstone of frozen shoulder treatment.
Can I use peptides for shoulder pain if I am over 50?
Age is actually one reason peptides may be particularly relevant. Natural healing capacity declines with age partly due to reduced peptide levels. GHK-Cu, for example, drops from 200 ng/mL at age 20 to 80 ng/mL by age 60. Supplementing with healing peptides may help partially compensate for this age-related decline. For those interested in longevity peptides and age-related health support, our guide covers the broader category. Anti-aging peptide research continues to grow as well.
External resources
Emerging Use of BPC-157 in Orthopaedic Sports Medicine: A Systematic Review (PMC)
Local and Systemic Peptide Therapies for Soft Tissue Regeneration (PMC)
For researchers serious about optimizing their shoulder recovery protocols, SeekPeptides offers the most comprehensive resource available, with evidence-based guides, proven protocols, and a community of thousands who have navigated these exact questions.
In case I do not see you, good afternoon, good evening, and good night. May your tendons stay strong, your shoulders stay mobile, and your healing stay steady. Join us.



