Jan 29, 2026
You are growing a human being inside your body. Every nutrient matters. Every supplement decision carries weight. So when you reach for that collagen powder that has been sitting in your cabinet, you pause. Is this safe? Will it help or harm your baby? The questions multiply faster than the cells dividing in your womb.
Here is what makes this decision particularly frustrating. Collagen is everywhere right now. Social media influencers swear by it for skin and joints. Your pregnant friends mention it casually. Yet when you search for actual answers about collagen peptides and pregnancy safety, you find conflicting information, vague reassurances, and precious little real guidance.
The truth sits somewhere between the marketing hype and the overly cautious disclaimers. Collagen peptides are generally considered safe during pregnancy by most healthcare professionals. But that general statement leaves out crucial details about timing, dosage, sources, and the specific ways collagen might actually benefit you during each trimester. It also ignores the legitimate concerns that deserve attention.
This guide exists because pregnant women deserve better than vague answers. You will find specific research, clear recommendations, trimester-by-trimester guidance, and honest acknowledgment of what we do not yet know. Whether you are trying to conceive, in your first trimester wondering about safety, or in your third trimester dealing with joint pain and stretched skin, this comprehensive resource covers everything about collagen supplementation during pregnancy. SeekPeptides has compiled the latest research and expert opinions into one actionable guide, because growing a baby is hard enough without having to piece together fragmented information about something as simple as a protein supplement.
What collagen peptides actually are and why pregnancy changes everything
Before diving into safety and benefits, understanding what you are actually putting into your body matters. Collagen peptides are not some exotic laboratory creation. They are simply collagen protein that has been broken down into smaller, more easily absorbed pieces through a process called hydrolysis.
Collagen itself is the most abundant protein in your body. It forms the structural framework of your skin, bones, tendons, ligaments, and organs. Think of it as the scaffolding that holds everything together. Your body produces collagen naturally using amino acids from the protein you eat, primarily glycine, proline, and hydroxyproline.
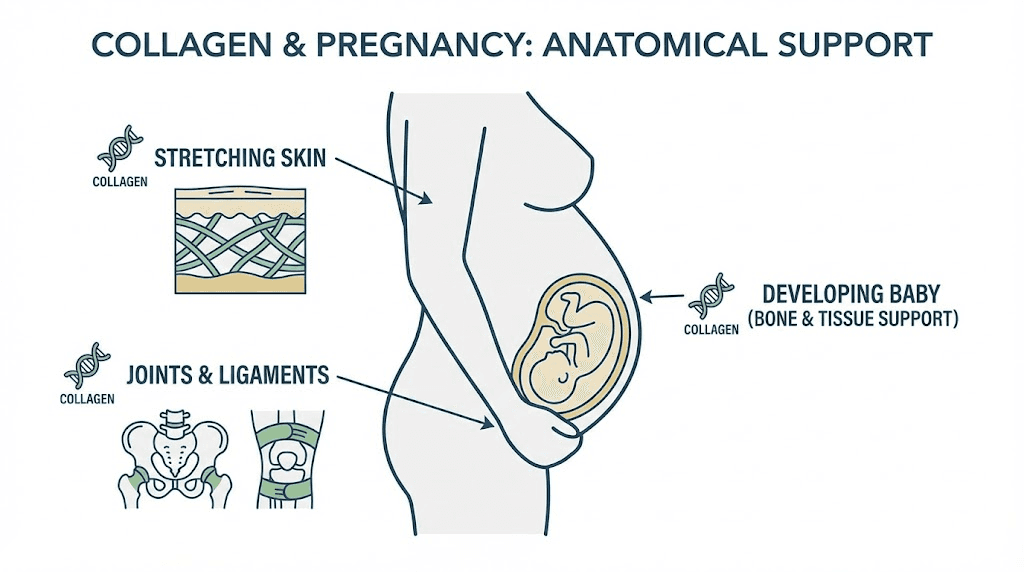
Here is where pregnancy changes the equation. Your body is suddenly building an entirely new human being. The demands on your collagen production skyrocket. Your uterus needs collagen to expand and support the growing baby. Your skin stretches to accommodate your changing body. Your joints loosen as hormones prepare you for childbirth. The placenta relies heavily on collagen for its structural integrity and proper function.
Research published in the International Journal of Biological Sciences confirms that collagen plays essential roles throughout pregnancy. It helps regulate the formation of blood vessels, contributes to connective tissue development, and may even support the developing immune system. The ratio of different collagen types, particularly Type I to Type III, affects tissue rigidity and function at the maternal-fetal interface.
The glycine question that most guides ignore
Glycine deserves special attention. This amino acid is abundant in collagen and plays a crucial role in pregnancy. It helps promote healthy cell growth and synthesis of collagen in the fetal brain, liver, and other organs. Glycine is essential for the formation of the placenta, fetal organs, and maternal tissues.
Here is the problem. Research suggests that during pregnancy, the body's need for glycine rises significantly to support collagen production. Yet some pregnant women may struggle to produce enough naturally, especially those with limited protein intake or those following plant-based diets that tend to be lower in glycine.
Glycine may become conditionally indispensable in late gestation. This scientific term means that while your body can normally produce glycine on its own, pregnancy demands might exceed your natural production capacity. This finding partly explains the growing interest in collagen supplementation during pregnancy.
The amino acids in collagen, glycine, proline, and hydroxyproline, are exactly what your body needs to build the structural proteins supporting both you and your baby. Rather than relying solely on your body to synthesize these from other protein sources, collagen peptides provide them directly in a form that is easily absorbed.
Types of collagen and which matter during pregnancy
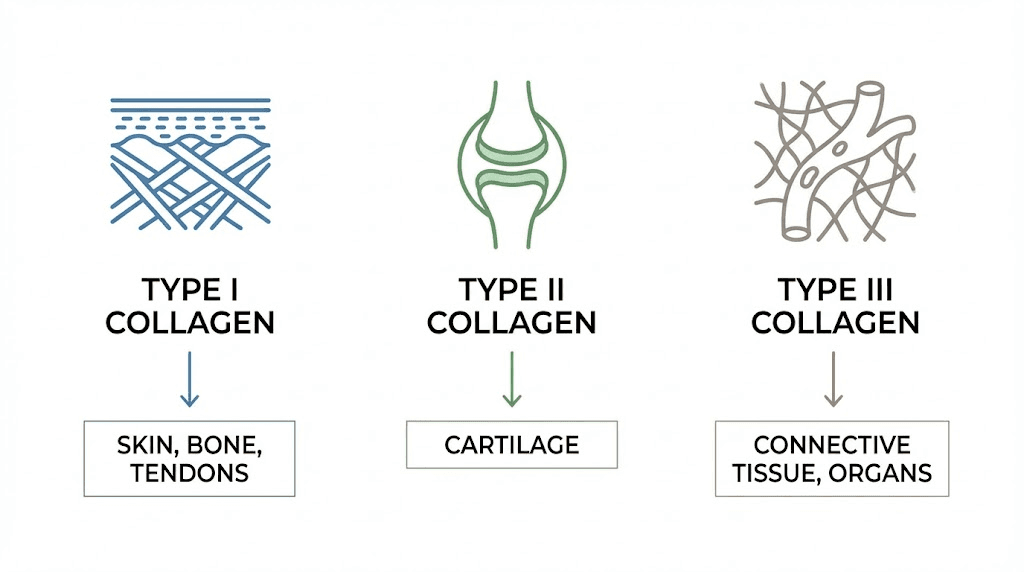
There are at least 28 different types of collagen in the human body, but about 80 to 90 percent falls into just three categories. Understanding these helps you choose the right supplement.
Type I collagen is the most abundant type. It is found in your skin, bones, tendons, and connective tissues. During pregnancy, Type I collagen supports the stretching skin of your growing belly and helps maintain the structural integrity of tissues under increased stress.
Type III collagen is the second most abundant. It supports the structure of muscles, organs, and arteries. Type III collagen is often called immature collagen because it is more flexible and elastic than Type I. This elasticity matters during pregnancy when tissues need to accommodate growth and change.
Type II collagen is primarily found in cartilage. While less relevant for the specific demands of pregnancy, it supports joint health, which can become problematic as pregnancy hormones loosen ligaments.
For pregnancy specifically, Types I and III are considered ideal because they target connective tissues and promote elasticity in the skin and throughout the body. Most collagen supplements on the market contain primarily Type I and III, particularly those derived from bovine sources.
The research reality on collagen peptides during pregnancy
Honest assessment time. The research on collagen supplementation specifically during pregnancy is limited. This is not because researchers suspect collagen is dangerous. The limitation exists because conducting randomized controlled trials on pregnant women presents significant ethical challenges. You cannot give one group of pregnant women a supplement and another group a placebo when there might be unknown risks to developing babies.
That said, the available evidence points toward safety. Here is what we actually know from research.
The Baginski study: direct evidence from third trimester
An open-label clinical study from 2016 evaluated a bovine collagen supplement taken during the third trimester and early postpartum period. The researchers followed pregnant women who took collagen supplements and compared them to a control group.
Results showed that serum total protein levels normalized in 100 percent of the collagen group, compared to 72 percent in the control group. No serious adverse events were reported by either group. Mild side effects such as gastrointestinal discomfort were infrequent in both groups. The study found no impact on breastfeeding, post-delivery complications, or newborn problems.
The researchers concluded that collagen during pregnancy was safe and well tolerated when taken during the last trimester and breastfeeding. While this is just one study, it provides some of the only direct evidence we have on collagen peptide safety during pregnancy.
What the meta-analyses tell us
In non-pregnant adults, meta-analyses of hydrolyzed collagen peptides report modest improvements in skin hydration and elasticity. These findings are biologically plausible for pregnancy, given the similar mechanisms at play, but have not been confirmed by pregnancy-specific randomized controlled trials.
The foundational research on collagen at the maternal-fetal interface shows that collagen is abundant there and plays crucial roles in tissue structure and immune tolerance. This makes biological sense. Your body already relies heavily on collagen during pregnancy. The question is whether supplementation provides additional benefit or just adds to what your body is already producing.
Expert medical opinions
Board-certified reproductive endocrinologists and fertility specialists have weighed in on this question. Most studies and reviews emphasize that collagen, especially in the form of hydrolyzed collagen peptides, is safe for consumption during pregnancy as long as it is taken in appropriate amounts.
Many healthcare professionals suggest that collagen peptides are safe for pregnant individuals when taken as directed. The consensus is not that collagen is proven safe through rigorous trials, but rather that there is no evidence suggesting harm, and the theoretical basis for benefit is sound.
This distinction matters. Absence of evidence of harm is not the same as evidence of safety. But when combined with the biological plausibility of benefit and the low theoretical risk of a protein supplement that gets broken down into amino acids, most experts land on cautious approval.
Potential benefits of collagen peptides during pregnancy
Understanding potential benefits helps you make an informed decision about whether supplementation makes sense for your situation. These benefits range from well-supported to theoretical, and this section distinguishes between them.
Supporting increased protein needs
Pregnancy significantly increases your protein requirements. Research suggests the average daily protein intake should be approximately 79 grams per day during early gestation around 16 weeks and 108 grams per day during late gestation around 36 weeks for normally nourished women. That is a substantial increase from pre-pregnancy needs.
Collagen peptides provide a convenient way to boost protein intake. A typical serving contains 5 to 15 grams of protein, and the powdered form mixes easily into coffee, tea, soups, smoothies, or baked goods.
Important caveat here. Collagen is not a complete protein. It lacks tryptophan, one of the essential amino acids. This means collagen should supplement your protein intake, not replace balanced protein sources like eggs, meat, fish, legumes, or dairy. Think of it as a protein boost that provides specific amino acids your body needs, not as your primary protein source.
Skin elasticity and stretch marks
Stretch marks affect 50 to 90 percent of pregnant women. They form when the rapid growth of your belly causes tears in the middle layer of skin tissues. Collagen and elastin fibers, which are responsible for skin elasticity, simply cannot keep up with the demands of your expanding skin.
Research from the University of Michigan found that the elastic fiber network in the dermis gets disrupted when stretch marks form. After giving birth, this network remains disrupted. The skin tries to repair it but appears ineffective, which promotes the lax, loose skin seen in more mature stretch marks.
Here is the honest truth about collagen and stretch marks. There is no scientific evidence that taking collagen can prevent stretch marks. Stretch marks are largely genetic and often unpreventable regardless of what creams, oils, or supplements you use.
However, there is evidence that collagen helps with skin elasticity and overall skin health. Studies on oral collagen supplementation show beneficial impacts on skin elasticity and hydration. Whether this translates to fewer or less severe stretch marks during pregnancy remains unproven but biologically plausible.
What experts do agree on is that taking collagen can be a beneficial way to support your skin while pregnant, even if it cannot guarantee stretch mark prevention.
Joint support during pregnancy
Pregnancy hormones, particularly relaxin, loosen your ligaments to prepare your body for childbirth. While necessary, this loosening can cause joint pain and instability. Add the weight gain and postural shifts of pregnancy, and achy joints become extremely common.
Though research has not specifically looked at the effect of collagen supplements on pregnancy-related joint discomfort, studies on athletes and people with knee osteoarthritis show that supplementing with collagen peptides may provide some relief.
The mechanism makes sense. Collagen provides the structural proteins that support joints, tendons, and ligaments. Supplementation may help maintain these tissues under the increased stress of pregnancy. Many pregnant women report subjective improvement in joint comfort with collagen supplementation, though controlled studies in pregnant populations are lacking.
Supporting fetal development
Collagen is essential for fetal growth and development. It plays a crucial role in forming the connective tissues and bones of the developing baby. Collagen helps the uterus prepare to receive and support an embryo and is needed for fetal organ development and growth.
The specific amino acids in collagen, glycine in particular, support the formation of the placenta, fetal organs, and maternal tissues. Collagen supplies amino acids needed for the baby's bones, skin, and organ development.
Whether supplementation provides benefits beyond a protein-adequate diet remains unproven. The argument for supplementation is that providing the specific amino acids directly may be more efficient than relying on your body to synthesize them from other protein sources, especially given the increased demands of pregnancy.
Cervical support
Your cervix is made of collagen fibers. These fibers help strengthen the cervix during pregnancy, keeping it closed and supporting the weight of your growing baby. Research has shown dynamic collagen changes in the cervix during the first trimester, with decreased collagen content associated with cervical insufficiency.
This is one area where the theoretical benefit of collagen supplementation is particularly interesting, though no clinical trials have specifically tested whether supplementation affects cervical strength or reduces risk of preterm birth.
Trimester by trimester guide to collagen supplementation
The demands on your body change throughout pregnancy. Here is how to think about collagen supplementation during each phase.
First trimester considerations
Collagen is considered safe to take during the first trimester. The supplement breaks down into amino acids during digestion, and these amino acids are the same ones you get from eating any protein. There is no mechanism by which hydrolyzed collagen peptides would pose unique risks during early pregnancy.
Some women find that collagen helps with their nausea. The glycine in collagen may have a calming effect on the digestive system. Others find it increases any nausea they are experiencing. Individual responses vary.
If you are new to collagen, the first trimester is a reasonable time to test how your body reacts. Start with a small dose, perhaps half a serving, and see how you feel before increasing to a full serving.
Practical first trimester tips include mixing collagen into ginger tea if you are dealing with nausea, adding it to smoothies that you can tolerate, and avoiding taking it on an empty stomach if that seems to trigger discomfort.
Second trimester focus
The second trimester is often considered the best time to start thinking seriously about collagen supplementation if you have not already. Your belly is growing, your skin is stretching, and more strain is being placed on your joints.
Supplementing with collagen during this trimester can help manage these changes. When collagen levels are optimal, the increased amino acids can support your joint and skin health as the physical demands of pregnancy intensify.
This is also when protein needs begin to increase more substantially. Adding collagen can help meet those needs without dramatically increasing your food intake, which can be helpful if you are dealing with digestive issues or limited appetite.
Many women notice the effects of pregnancy on their skin during the second trimester as growth accelerates. Beginning collagen supplementation before significant stretching occurs might theoretically provide more benefit than starting after stretch marks have already formed, though this remains unproven.
Third trimester demands
As your due date approaches, your body is working harder than ever. Many women feel heavier, experience swelling, and deal with aching hips or lower back pain. Protein needs are at their highest during this time.
This is where taking collagen supplements can help you finish strong. The third trimester is also the phase with the most direct research support for safety, thanks to the Baginski study mentioned earlier.
The glycine in collagen may also support sleep during the uncomfortable final weeks of pregnancy. Increased collagen production has a role in aiding restful sleep due to glycine. Less inflammation equals a calmer brain, which equals better rest.
If you are considering starting collagen for pregnancy joint pain, beginning earlier rather than later makes sense since it could take weeks or months before you start to notice any relief.
When to start supplementation
There is no official guidance on the optimal time to begin collagen supplementation during pregnancy. Based on available evidence and expert opinions, here are reasonable approaches.
If you were already taking collagen before pregnancy, continuing is generally considered safe. Your body is already adapted to the supplement.
If you are starting new during pregnancy, the second trimester is often recommended as an ideal time. By then, the first trimester sensitivity has usually passed, and you can address the increasing physical demands before they become overwhelming.
If you want to be most conservative, waiting until the third trimester means using collagen during the pregnancy phase with the most direct safety data.
Regardless of timing, consulting with your healthcare provider before starting any new supplement remains the standard recommendation.
Dosage guidelines for pregnant women
There is no official daily recommendation for collagen during pregnancy. However, most healthcare professionals suggest a safe and effective dose falls between 2.5 and 10 grams per day.
Some sources suggest a slightly broader range of 2 to 15 grams per day. Typical servings in commercial products are 5 to 15 grams per serving. Higher doses are generally achieved through collagen powders rather than capsules.
Practical dosing recommendations
Start with 2.5 to 5 grams per day if you are new to collagen supplementation. This allows you to assess how your body responds before increasing the dose.
Work up to 10 grams per day if you tolerate the initial dose well. This puts you in the range that most studies have used and that most experts recommend.
Count your collagen toward your protein goal. Remember that while collagen adds to your protein intake, it should not displace balanced meals or your prenatal vitamin. Collagen is supplemental, not foundational.
Consistency matters more than exact dosing. Taking 5 grams daily for months will likely produce better results than sporadically taking 15 grams. Build the habit rather than optimizing the dose.
How to take collagen during pregnancy
Hydrolyzed collagen peptides are the best form for pregnancy because they are easily absorbed, gentle on digestion, and versatile in use.
Collagen powder can be added to coffee, tea, soups, smoothies, oatmeal, yogurt, or baked goods. It dissolves easily in both hot and cold liquids. Most hydrolyzed collagen is flavorless or nearly so, making it easy to incorporate without changing the taste of your food or drinks.
Timing is flexible. Unlike some supplements, collagen does not need to be taken at a specific time of day or with or without food. Take it when convenient and when you will remember.
Some women find that taking collagen in the morning as part of their routine works best. Others prefer adding it to an evening beverage. There is no evidence that timing affects efficacy during pregnancy.

Bovine versus marine collagen during pregnancy
Not all collagen supplements are created equal. The source of the collagen matters, particularly during pregnancy.
Bovine collagen: the safer choice during pregnancy
Bovine collagen comes from cows and provides both Type I and Type III collagen. This combination makes it ideal for supporting skin, joints, gut, and muscle health during pregnancy.
Bovine collagen is the form most commonly recommended for pregnant women. It provides eight essential amino acids and is a rich source of glycine and proline. The third trimester safety study used bovine collagen, so it has the most direct research support during pregnancy.
When choosing bovine collagen, look for products from grass-fed sources. Grass-fed bovine collagen tends to be higher quality with fewer additives or contaminants.
Marine collagen: proceed with caution
Marine collagen comes from fish and contains primarily Type I collagen. It is often touted as more bioavailable than bovine collagen, meaning the body may absorb it more easily.
However, there is a significant concern. Marine collagen is obtained from fish skin, which can contain higher amounts of mercury. Some experts suggest avoiding marine collagen during pregnancy due to this potential contamination risk.
The evidence is not definitive. High-quality marine collagen that has been tested for heavy metals and sourced responsibly may be safe. But given that bovine collagen offers similar benefits without this concern, many healthcare providers recommend bovine as the safer default during pregnancy.
If you choose marine collagen, ensure it is from a reputable brand that conducts third-party testing for heavy metals. Wild-caught, sustainably harvested sources are generally preferable to farmed fish sources.
Other collagen sources
Porcine collagen from pigs is another option and shares the safety profile of bovine collagen. It provides similar collagen types and amino acid profiles.
Chicken collagen is less common in supplements but is rich in Type II collagen, which primarily supports cartilage. It is less studied during pregnancy but there is no theoretical reason to consider it less safe than bovine.
Eggshell membrane collagen is emerging as a source but has limited research in pregnancy. Most experts recommend sticking with bovine collagen as the default choice unless you have a specific reason to choose otherwise.
Safety considerations and potential risks
While collagen is generally considered safe during pregnancy, honest discussion of potential risks helps you make an informed decision.
Quality and contamination concerns
The safety of collagen supplements largely depends on the quality of the product and the absence of harmful additives or contaminants. Low-quality supplements may contain heavy metals or other impurities that could pose risks to both mother and developing baby.
Collagen peptides are regulated in the United States as dietary supplements, not as drugs. This means they do not undergo FDA premarket approval for safety or effectiveness. Many supplements have not been tested in pregnant populations.
Protein powders, antioxidant supplements, and vitamins and minerals are notorious for being contaminated with metals during the manufacturing process. The safest supplements for pregnant women are those free of heavy metals, verified through third-party testing.
How to choose a safe product
Look for third-party testing certifications. NSF, USP, or Informed Choice certification indicates that the product has been tested for purity and quality by an independent laboratory.
Choose products from reputable brands with transparent sourcing. Grass-fed bovine or wild-caught marine collagen from companies that disclose their sources tends to be higher quality.
Check the ingredient list. The safest collagen supplements for pregnancy contain collagen peptides and nothing else. Avoid products with lots of additives, artificial flavors, or sweeteners.
Be especially cautious about supplements that contain added vitamin A. The NHS recommends avoiding excess vitamin A during pregnancy because high doses can harm the developing baby. Make sure your collagen supplement does not contain added vitamin A.
Allergies and sensitivities
Avoid collagen sourced from animals you are allergic to. If you have a beef allergy, avoid bovine collagen. If you have a fish or shellfish allergy, avoid marine collagen.
Some people experience mild side effects from collagen supplementation, including nausea, digestive changes, or gastrointestinal discomfort. These effects are usually mild and infrequent but may be more noticeable during pregnancy when the digestive system is already stressed.
The fundamental limitation of current research
The honest truth is that high-quality pregnancy-specific randomized controlled trials are still lacking. We do not have the same level of evidence for collagen safety during pregnancy that we have for, say, prenatal vitamins.
The general consensus is that collagen is likely safe based on what it is, how it is metabolized, and the absence of reported problems. But likely safe is not the same as proven safe. If you are risk-averse, this distinction matters.
Your healthcare provider can help you weigh the potential benefits against the uncertainty. For some women, the theoretical benefits make supplementation worthwhile. For others, getting collagen from food sources feels more comfortable during pregnancy.
Natural food sources of collagen during pregnancy
If you prefer to support your collagen needs through food rather than supplements, several options provide the building blocks your body needs.
Bone broth: the traditional approach
Bone broth is made by simmering animal bones for extended periods, extracting collagen and other nutrients into a drinkable liquid. It has been used for centuries as a nourishing food during pregnancy and postpartum.
Homemade bone broth from grass-fed or pasture-raised animals provides collagen along with minerals like calcium and magnesium. Commercial bone broth products vary widely in quality and actual collagen content.
The downside of bone broth is that the collagen content is highly variable and generally lower than what you would get from a collagen supplement. You would need to consume significant amounts of bone broth daily to match the collagen in a single serving of hydrolyzed peptides.
Foods that support collagen production
Your body produces collagen from amino acids, primarily glycine, proline, and hydroxyproline. Foods rich in these amino acids support your natural collagen production.
Eggs, dairy, legumes, and soy foods deliver the amino acids needed for collagen synthesis. Chicken, beef, and fish provide complete proteins with all the building blocks.
Vitamin C is essential for collagen synthesis. Incorporate citrus fruits, berries, peppers, and green leafy vegetables to support natural collagen production. Vitamin C and collagen work together, with vitamin C acting as a cofactor in the enzymatic processes that create collagen.
Zinc and copper are also needed for collagen production. Nuts, seeds, and whole grains provide these minerals.
The food versus supplement question
You can meet your collagen needs through a varied diet that includes protein at every meal, plenty of vitamin C, and adequate minerals. Supplementation is not strictly necessary for a healthy pregnancy as long as you are meeting your overall protein needs.
That said, supplements offer convenience and guaranteed dosing. If your diet is limited due to food aversions, nausea, or other pregnancy complications, a collagen supplement can fill nutritional gaps more reliably than trying to eat specific foods.
The best approach depends on your individual circumstances, preferences, and what you can realistically maintain throughout pregnancy.
Collagen during breastfeeding and postpartum
The benefits of collagen do not end at delivery. Postpartum recovery and breastfeeding create their own demands on your body.
Safety during breastfeeding
Collagen is a natural part of the human diet, and it is generally considered safe during breastfeeding. Because it is broken down into amino acids and small peptides during digestion, its impact on breast milk is minimal.
There is currently no evidence suggesting collagen supplementation is harmful to either a breastfeeding mother or her baby. Studies indicate that moderate changes in a mother's protein intake do not significantly alter the overall protein content of her breast milk.
There is also no evidence that collagen harms milk supply. Getting enough protein overall supports healthy milk production, and collagen contributes to protein intake.
Postpartum recovery benefits
Collagen supplementation can aid postpartum recovery by supporting tissue repair and healing. After childbirth, your body needs to recover from the physical strains of pregnancy and delivery.
Collagen helps restore skin elasticity after childbirth, may reduce the appearance of stretch marks over time, and supports overall tissue repair. If you had a cesarean section, collagen may support wound healing, though this has not been specifically studied.
The joint laxity that develops during pregnancy due to relaxin does not immediately reverse after delivery. Collagen supplementation may support joint recovery as your body returns to its pre-pregnancy state.
Timing recommendations for postpartum
It is fine to continue taking collagen after pregnancy if you were using it during pregnancy. Some women who waited until the third trimester to start continue into the postpartum period.
Some experts recommend that mothers wait at least six months postpartum before starting collagen supplementation if they were not using it during pregnancy. This conservative approach ensures the baby's systems are more mature before introducing any new supplements to the mother's diet that could potentially affect breast milk.
However, this recommendation is not based on evidence of harm but rather on an abundance of caution given the limited research. Most breastfeeding mothers who choose to use collagen do so without waiting and without reported problems.
Common concerns and misconceptions
Will collagen cause weight gain during pregnancy?
Collagen does not cause weight gain beyond what any protein source would contribute. A typical serving contains 30 to 50 calories from protein. This is negligible in the context of pregnancy nutrition and will not meaningfully impact weight.
In fact, protein tends to be satiating, which may help manage hunger and prevent excessive weight gain from less nutritious food choices.
Can collagen prevent stretch marks?
There is no scientific evidence that collagen can prevent stretch marks. Stretch marks are largely determined by genetics, how much weight you gain, how quickly you gain it, and hormonal factors. No cream, oil, or supplement has been proven to prevent them.
That said, collagen supports overall skin health and elasticity, which may reduce the severity of stretch marks or support skin recovery after they form.
Does collagen break a fast?
If you are practicing intermittent fasting during pregnancy, which most healthcare providers advise against, collagen would technically break a fast because it contains protein and calories. However, intermittent fasting is generally not recommended during pregnancy due to the constant nutritional needs of the developing baby.
Can I take collagen with my prenatal vitamin?
Yes. Collagen does not interact with the vitamins and minerals in prenatal supplements. You can take both without concern. In fact, the vitamin C in many prenatal vitamins supports collagen synthesis.
Just ensure your collagen supplement does not contain added vitamin A, which could push your total intake too high when combined with a prenatal vitamin.
Is hydrolyzed collagen different from regular collagen?
Hydrolyzed collagen, also called collagen peptides or collagen hydrolysate, has been broken down into smaller peptides for easier absorption. Regular collagen would be the intact protein, which is harder for your body to absorb and use.
For supplementation purposes, hydrolyzed collagen or collagen peptides are the recommended forms because they are more bioavailable. The terms are often used interchangeably.
Creating your pregnancy collagen protocol
Based on the available evidence and expert recommendations, here is a practical protocol for using collagen peptides during pregnancy.
Before starting
Consult with your healthcare provider. While collagen is generally considered safe, your provider knows your specific health situation and can advise accordingly.
Choose a high-quality supplement. Look for grass-fed bovine collagen with third-party testing certification. Avoid products with unnecessary additives or added vitamin A.
Check for allergens. Ensure the collagen source does not conflict with any food allergies you have.
Starting protocol
Begin with 2.5 to 5 grams per day. This lower dose allows you to assess tolerance before increasing. Take it with food initially to minimize any digestive discomfort.
Monitor how you feel for the first week. Most women tolerate collagen well, but some experience mild nausea or digestive changes. If you experience discomfort, try taking it at a different time of day or with different foods.
Maintenance protocol
Increase to 10 grams per day if you tolerate the initial dose well. This puts you in the range that most experts recommend and that most studies have used.
Take it consistently. Daily use over weeks to months is more important than any single high dose. Build it into your routine so you do not forget.
Continue through pregnancy and into postpartum if you find it beneficial. There is no need to stop at delivery if you were using collagen during pregnancy.
Optimizing absorption
Combine collagen with vitamin C to support your body's natural collagen synthesis. Adding collagen to a citrus smoothie or taking it alongside a vitamin C rich meal may enhance benefits.
Hydration matters. Collagen works with water to support tissue health. Ensure you are drinking adequate fluids, which is especially important during pregnancy anyway.
Consistency trumps timing. There is no evidence that taking collagen at a specific time of day enhances its effects. Take it when convenient for you.
When to avoid collagen during pregnancy
While collagen is safe for most pregnant women, there are situations where caution or avoidance is appropriate.
If you have a known allergy to the collagen source, avoid that type. Bovine collagen should be avoided by those with beef allergies. Marine collagen should be avoided by those with fish or shellfish allergies.
If you have a high-risk pregnancy with complications, discuss any supplement use with your healthcare provider before starting. The general safety profile may not apply to complex medical situations.
If you experience persistent nausea, digestive upset, or any adverse reaction after starting collagen, discontinue use and consult your provider.
If you cannot find a product that meets quality standards, meaning third-party tested, from a reputable source, and free of concerning additives, then waiting until you can find a suitable product is reasonable.
Frequently asked questions
Is collagen peptides safe during pregnancy?
Yes, collagen peptides are generally considered safe during pregnancy when taken as directed. They break down into amino acids during digestion, similar to any protein food. While research specifically on pregnant women is limited, there is no evidence of harm, and most healthcare professionals consider them safe for pregnant individuals. Always consult your healthcare provider before starting any supplement during pregnancy.
When should I start taking collagen during pregnancy?
You can start taking collagen at any point during pregnancy. The second trimester is often recommended as an ideal time to begin because first trimester nausea has usually passed and you can address the increasing physical demands before they become overwhelming. If you want the most conservative approach, the third trimester has the most direct safety research. If you were already taking collagen before pregnancy, continuing is generally considered safe.
How much collagen should a pregnant woman take daily?
Most healthcare professionals suggest between 2.5 and 10 grams of collagen per day during pregnancy. Start with 2.5 to 5 grams to assess tolerance, then increase to 10 grams if you tolerate it well. Count this toward your overall protein intake, which should be approximately 79 grams per day in early pregnancy and 108 grams per day in late pregnancy. Consult your provider for personalized recommendations.
Which type of collagen is best during pregnancy?
Bovine collagen is generally recommended as the safest choice during pregnancy. It provides Types I and III collagen, which support skin, joints, and connective tissues. Bovine collagen has the most direct research support during pregnancy. Marine collagen may contain higher levels of mercury, so if you choose marine collagen, ensure it is from a reputable source with third-party testing for heavy metals.
Can collagen help prevent stretch marks during pregnancy?
There is no scientific evidence that collagen can prevent stretch marks. Stretch marks are largely genetic and often unpreventable. However, collagen supports skin elasticity and overall skin health, which may reduce the severity of stretch marks or support skin recovery after they form. Think of collagen as supportive rather than preventive.
Is it safe to take collagen while breastfeeding?
Yes, collagen is generally considered safe during breastfeeding. Because it breaks down into amino acids during digestion, its impact on breast milk is minimal. There is no evidence that collagen harms milk supply or affects the baby. Some experts suggest waiting six months postpartum before starting if you did not use collagen during pregnancy, though this recommendation is based on caution rather than evidence of harm.
Can I take collagen with my prenatal vitamin?
Yes, you can safely take collagen with your prenatal vitamin. Collagen does not interact with the vitamins and minerals in prenatal supplements. Just ensure your collagen product does not contain added vitamin A, which could push your total intake too high when combined with a prenatal vitamin.
Does collagen have any side effects during pregnancy?
Most people tolerate collagen well, but some experience mild side effects such as nausea, digestive changes, or gastrointestinal discomfort. These effects may be more noticeable during pregnancy when the digestive system is already stressed. If you experience persistent discomfort, try adjusting the timing, taking it with food, or reducing the dose. Discontinue use and consult your provider if problems persist.
For women serious about optimizing their pregnancy nutrition and understanding how supplements can support their journey, SeekPeptides provides comprehensive resources on peptides, proteins, and evidence-based supplementation strategies.



