Feb 4, 2026
Why you need a retatrutide dosage calculator
You have a vial of retatrutide sitting in front of you. Maybe it is 5mg. Maybe 10mg. Maybe 20mg. And the question gnawing at you is simple but critical: how much bacteriostatic water do I add, and how many units do I draw to get the right dose?
Get this wrong and you waste peptide. Or worse, you underdose for weeks and wonder why nothing is happening. Get it really wrong, and you overshoot your target dose by two or three times, inviting a wave of nausea that could have been avoided entirely.
This is where a retatrutide dosage calculator becomes essential. Not a nice-to-have. Essential. Because the math behind peptide reconstitution involves converting between milligrams, micrograms, milliliters, and insulin syringe units, and one decimal place error changes everything. A 10mg vial reconstituted with 2mL of bacteriostatic water gives you 5,000mcg per mL. That same vial with 1mL gives you 10,000mcg per mL. The difference between drawing 4 units and 8 units on your syringe for the same dose. Miss that distinction and your entire protocol falls apart before it even begins.
Retatrutide is not like older peptides where dosing was relatively straightforward. As a triple-receptor agonist targeting GIP, GLP-1, and glucagon receptors simultaneously, it follows a specific dose escalation schedule that changes every four weeks. You start low. You build gradually. And at every step, you need to know exactly how many units to draw from your reconstituted vial. The retatrutide dosage chart tells you the milligram target. The calculator tells you how to actually get there with the vial and syringe in your hands.
This guide covers everything you need to calculate retatrutide doses accurately. From the basic reconstitution formula to vial-specific reference tables, from dose escalation math to troubleshooting common calculation errors. Whether you are working with a 5mg research vial or a 30mg vial, by the end of this article you will understand exactly how to determine concentration, volume per dose, and total doses per vial without second-guessing yourself. SeekPeptides has helped thousands of researchers navigate these exact calculations, and this guide distills that knowledge into one comprehensive reference.
The fundamental reconstitution formula every researcher needs
Before you can calculate any dose, you need to understand one formula. Just one. Every peptide dosage calculation in existence reduces to this:
Concentration = Peptide Amount (mg) / Water Volume (mL)
That is it. Everything else builds from here.
If you have a 10mg vial of retatrutide and you add 2mL of bacteriostatic water, your concentration becomes 10mg / 2mL = 5mg/mL. In micrograms, that is 5,000mcg/mL. This number is the foundation of every dose you will draw from that vial.
Why micrograms matter here: retatrutide doses are typically discussed in milligrams (1mg, 2mg, 4mg, 8mg, 12mg) at the protocol level, but when you are physically drawing from a syringe, you are working in fractions of a milliliter. Converting to micrograms eliminates decimal confusion. A 2mg dose from a 5mg/mL solution requires 0.4mL, which is 40 units on a standard U-100 insulin syringe. In micrograms, you need 2,000mcg from a 5,000mcg/mL solution. Same math, different notation, fewer errors.
Understanding insulin syringe units
This trips up more researchers than any other part of the calculation. A standard U-100 insulin syringe has 100 units per 1mL. Each unit equals 0.01mL. That is all.
So when someone says "draw 20 units," they mean draw 0.2mL. When they say "draw 5 units," they mean 0.05mL. The unit markings on the syringe are simply a more readable way to measure tiny volumes. No magic. No hidden conversions. Just 100 units equals 1 milliliter.
Here is where it connects to your peptide calculator results. If your reconstituted retatrutide has a concentration of 5mg/mL and you need a 2mg dose, the math goes: 2mg / 5mg per mL = 0.4mL = 40 units. For a 4mg dose: 4mg / 5mg per mL = 0.8mL = 80 units. For an 8mg dose: 8mg / 5mg per mL = 1.6mL. That exceeds a standard 1mL syringe, which means you would either need to split the injection into two draws or use a different reconstitution volume.
This is exactly why choosing the right amount of bacteriostatic water matters from the very start.
Choosing your reconstitution volume
The amount of water you add determines everything downstream. Less water means a more concentrated solution, which means smaller injection volumes. More water means a more dilute solution, which means larger volumes per dose but potentially more precision for smaller doses.
For retatrutide specifically, the dose escalation schedule eventually reaches 8mg or 12mg per week. If you reconstitute too dilute, you will need to draw volumes that exceed your syringe capacity. If you reconstitute too concentrated, the small starting doses of 1mg or 2mg become impossibly tiny volumes to measure accurately.
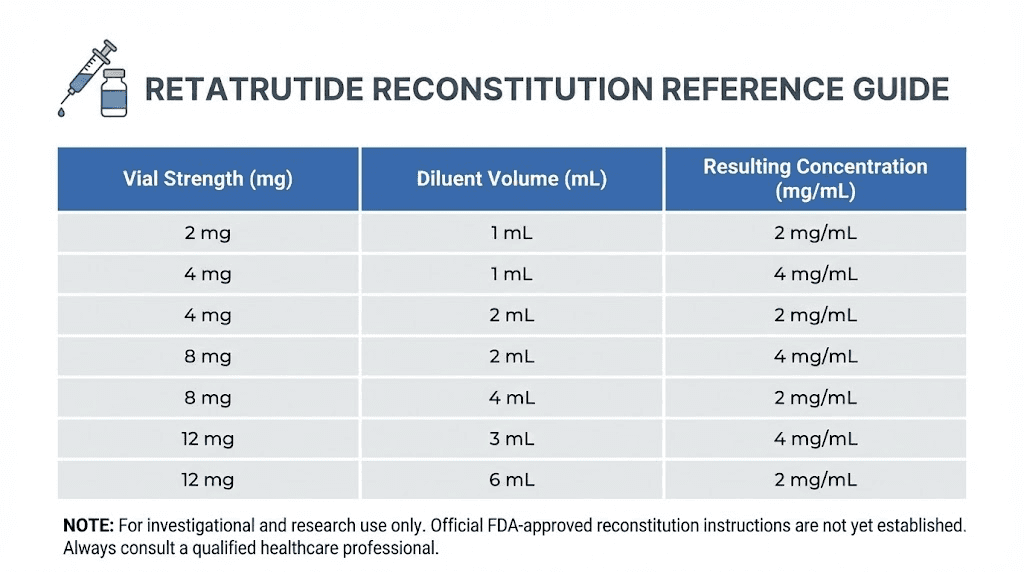
The sweet spot depends on your vial size. Here is a practical guide:
5mg vial: Add 1mL of bacteriostatic water for a concentration of 5mg/mL (5,000mcg/mL). A 1mg dose = 0.2mL = 20 units. A 2mg dose = 0.4mL = 40 units. This gives you 2.5 total doses at 2mg each, which means the 5mg vial works best for starting dose weeks.
10mg vial: Add 2mL of bacteriostatic water for a concentration of 5mg/mL (5,000mcg/mL). A 2mg dose = 0.4mL = 40 units. A 4mg dose = 0.8mL = 80 units. You get 5 doses at 2mg or 2.5 doses at 4mg. This is the most common research vial size and the most versatile for dose escalation.
20mg vial: Add 2mL of bacteriostatic water for a concentration of 10mg/mL (10,000mcg/mL). A 4mg dose = 0.4mL = 40 units. An 8mg dose = 0.8mL = 80 units. A 12mg dose = 1.2mL, which requires two draws. Alternatively, add 1mL for 20mg/mL, making a 4mg dose just 20 units and a 12mg dose 60 units, though the small volumes for lower doses become harder to measure precisely.
30mg vial: Add 3mL of bacteriostatic water for a concentration of 10mg/mL (10,000mcg/mL). A 4mg dose = 0.4mL = 40 units. An 8mg dose = 0.8mL = 80 units. A 12mg dose = 1.2mL. This provides enough volume for a complete dose escalation from a single vial if managed carefully.
Understanding these relationships is what separates researchers who get consistent results from those who wonder why their retatrutide protocol seems unpredictable. The reconstitution calculator automates this math, but knowing the logic behind it protects you from blindly trusting numbers you do not understand.
Retatrutide dose escalation schedule explained
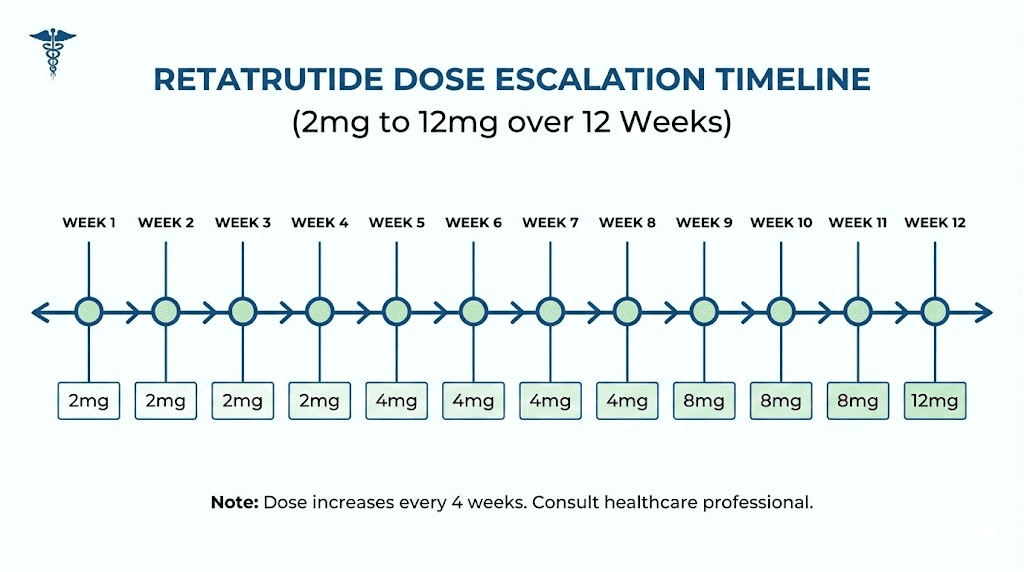
Retatrutide is not a fixed-dose peptide. You do not pick one number and stay there. The clinical escalation protocol from the Phase 2 NEJM trial established a specific titration schedule that increases the dose every four weeks, starting low and building to a target maintenance dose.
Why the gradual approach? Because retatrutide activates three receptors simultaneously. GLP-1 and GIP receptors affect appetite, insulin sensitivity, and satiety. The glucagon receptor component increases energy expenditure and fat oxidation. Hitting all three at full force from day one creates a gastrointestinal response that most people find unmanageable. The slow build lets your body adapt to each receptor activation incrementally.
Standard escalation protocol from clinical trials
The Phase 2 trial published in the New England Journal of Medicine tested several dose groups. The escalation schedules that showed the best balance of efficacy and tolerability followed this general pattern:
Weeks 1 through 4: 2mg once weekly. This is the initiation phase. The primary goal is not weight loss, it is receptor adaptation. Most researchers experience mild appetite changes during this period, and some report no noticeable effects at all. That is normal. The 2mg dose primarily activates GLP-1 with minimal glucagon receptor engagement.
Weeks 5 through 8: 4mg once weekly. The first significant increase. GIP receptor activation becomes more pronounced at this level, and appetite suppression typically becomes noticeably stronger. Gastrointestinal side effects, if they occur, usually appear during this transition. Eating smaller meals and avoiding high-fat foods during the first week at this dose helps considerably.
Weeks 9 through 12: 8mg once weekly. This is where retatrutide begins to differentiate itself from single and dual agonists. The glucagon receptor component becomes meaningfully active at this dose range, increasing thermogenesis and metabolic rate. The Phase 2 trial showed that participants at 8mg achieved an average of 22.8% body weight reduction at 48 weeks.
Weeks 13 onward: 12mg once weekly (target maintenance dose for maximum efficacy). The highest dose studied in Phase 2, producing up to 24.2% average weight loss at 48 weeks. Not everyone needs to reach 12mg. Some researchers find that 8mg provides sufficient results with fewer side effects. The decision to escalate from 8mg to 12mg depends on individual response, tolerability, and research objectives.
An alternative starting protocol uses 1mg for the first four weeks before moving to 2mg, then following the standard escalation from there. This ultra-conservative approach adds four extra weeks to the titration timeline but can significantly reduce initial gastrointestinal symptoms, particularly for researchers who have experienced severe nausea with other GLP-1 based peptides.
What the escalation means for your calculator
Every four weeks, your dose changes. That means the number of units you draw from your syringe changes. This is where errors creep in, because researchers get comfortable drawing the same amount week after week and then forget to adjust when the escalation hits.
Using a 10mg vial reconstituted with 2mL (concentration: 5mg/mL):
At 2mg per week: Draw 0.4mL = 40 units. The 10mg vial provides 5 weekly doses at this level.
At 4mg per week: Draw 0.8mL = 80 units. The 10mg vial provides 2.5 weekly doses, meaning you will need a new vial during weeks 5 through 8.
At 8mg per week: Draw 1.6mL = 160 units. This exceeds a standard 1mL syringe. You would need to split into two draws of 80 units each. The 10mg vial provides only 1.25 weekly doses at this level.
At 12mg per week: Draw 2.4mL = 240 units. At this point, the 10mg vial barely covers one dose. Most researchers at this phase switch to 20mg or 30mg vials for practical efficiency.
This is why planning your vial purchases around your escalation schedule matters. Starting with 10mg vials for the first 8 weeks and transitioning to 20mg or 30mg vials for the maintenance phase is the most cost-effective and practical approach for most research protocols.
Complete dosage reference tables by vial size
These tables give you the exact numbers for every common vial and reconstitution combination. Bookmark this section. You will come back to it.
5mg vial reference table
Water Added | Concentration | 1mg Dose | 2mg Dose | 4mg Dose | Total Doses (2mg) |
|---|---|---|---|---|---|
0.5mL | 10mg/mL | 10 units | 20 units | 40 units | 2.5 |
1.0mL | 5mg/mL | 20 units | 40 units | 80 units | 2.5 |
2.0mL | 2.5mg/mL | 40 units | 80 units | N/A (160 units) | 2.5 |
The 5mg vial works best for the initial 2mg dosing phase. At 1mL reconstitution, each 2mg dose uses 40 units, giving you clean syringe markings that are easy to read. Once you escalate beyond 2mg per week, the 5mg vial becomes impractical because you burn through it too quickly. Some researchers keep a 5mg vial specifically for the first two weeks at 1mg (using just 20 units per dose), then switch to larger vials for the remainder of the protocol.
10mg vial reference table
Water Added | Concentration | 2mg Dose | 4mg Dose | 8mg Dose | Total Doses (4mg) |
|---|---|---|---|---|---|
1.0mL | 10mg/mL | 20 units | 40 units | 80 units | 2.5 |
2.0mL | 5mg/mL | 40 units | 80 units | Split required | 2.5 |
The 10mg vial is the workhorse of most retatrutide research. Reconstituted with 1mL, it covers doses from 2mg (20 units) through 8mg (80 units) without exceeding the syringe capacity. The trade-off is that 1mg and 2mg doses become very small volumes (10 and 20 units respectively), where measurement precision on cheaper syringes can be questionable. If accuracy at low doses concerns you, reconstituting with 2mL gives you more readable volumes at the cost of requiring split draws at 8mg and above.
For researchers using our peptide dosage calculator, simply input 10 for the vial amount, your chosen water volume, and your target dose. The tool handles the conversion automatically and tells you both the units to draw and the total number of doses available from the vial.
20mg vial reference table
Water Added | Concentration | 4mg Dose | 8mg Dose | 12mg Dose | Total Doses (8mg) |
|---|---|---|---|---|---|
1.0mL | 20mg/mL | 20 units | 40 units | 60 units | 2.5 |
2.0mL | 10mg/mL | 40 units | 80 units | Split required | 2.5 |
The 20mg vial shines during the escalation and maintenance phases. Reconstituted with 1mL for 20mg/mL concentration, even the highest 12mg dose only requires 60 units, well within a single syringe draw. The 2mL reconstitution option works well for the 4mg and 8mg phases but requires splitting for 12mg doses. Most experienced researchers who plan to reach maintenance doses of 8mg or 12mg prefer the 1mL reconstitution for simplicity.
30mg vial reference table
Water Added | Concentration | 4mg Dose | 8mg Dose | 12mg Dose | Total Doses (12mg) |
|---|---|---|---|---|---|
1.5mL | 20mg/mL | 20 units | 40 units | 60 units | 2.5 |
3.0mL | 10mg/mL | 40 units | 80 units | Split required | 2.5 |
The 30mg vial is ideal for researchers on maintenance doses who want to minimize reconstitution frequency. At 20mg/mL (1.5mL water), a single vial provides 2.5 weeks at 12mg per week. This reduces the number of times you need to reconstitute, which matters because every reconstitution event introduces a small risk of contamination or peptide degradation. Fewer reconstitutions means more consistent potency across your protocol.
Understanding these tables eliminates guesswork. But if you prefer automated calculations, the SeekPeptides reconstitution calculator lets you input any vial size and water volume combination to get instant results. The tool also accounts for proper reconstitution technique, which is just as important as getting the math right.
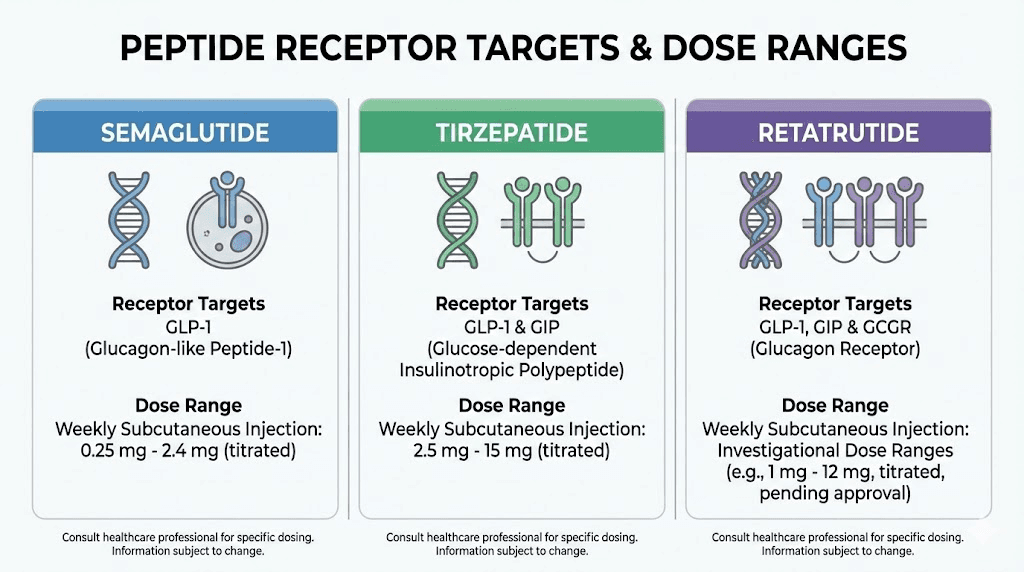
How retatrutide dosing compares to other GLP-1 peptides
If you have experience with semaglutide or tirzepatide, you might assume retatrutide dosing follows a similar pattern. It does not. The triple-receptor mechanism fundamentally changes how dose response works, and failing to appreciate these differences leads to calculation errors that undermine your entire research protocol.
Dose comparison table
Parameter | Semaglutide | Tirzepatide | Retatrutide |
|---|---|---|---|
Receptor targets | GLP-1 only | GLP-1 + GIP | GLP-1 + GIP + Glucagon |
Starting dose | 0.25mg weekly | 2.5mg weekly | 1-2mg weekly |
Maintenance dose range | 1.0-2.4mg weekly | 5-15mg weekly | 8-12mg weekly |
Escalation interval | 4 weeks | 4 weeks | 4 weeks |
Time to maintenance | 16-20 weeks | 16-20 weeks | 12-16 weeks |
Peak weight loss (trials) | ~15-17% | ~21% | ~24.2% |
Administration | Once weekly SC | Once weekly SC | Once weekly SC |
Notice that retatrutide doses are measured in milligrams, similar to tirzepatide, but the dose range is different. Semaglutide operates in sub-milligram to low milligram territory. Tirzepatide spans 2.5mg to 15mg. Retatrutide sits between them at 1mg to 12mg. This distinction matters when switching between peptides or when researchers accidentally apply semaglutide calculation logic to retatrutide, a common and potentially significant mistake.
The glucagon receptor component in retatrutide creates a unique metabolic profile that the other two lack. While semaglutide and tirzepatide primarily reduce food intake through appetite suppression, retatrutide simultaneously increases energy expenditure. This dual mechanism, eating less while burning more, accounts for the superior weight loss outcomes observed in clinical trials. It also means that the dose-response curve is steeper, which reinforces why accurate calculation and gradual escalation are non-negotiable.
For researchers transitioning from other weight loss peptides, the SeekPeptides platform provides detailed comparison tools and protocol guidance for making informed transitions between different GLP-1 class compounds.
Why you cannot simply convert doses between peptides
A question that comes up constantly: "I am on 10mg of tirzepatide, what is the equivalent retatrutide dose?" The honest answer is that there is no direct equivalence. Different receptor binding profiles, different pharmacokinetics, different dose-response curves. A researcher who tries to calculate an "equivalent" starting dose of retatrutide based on their tirzepatide experience is making a category error.
The correct approach is always to start retatrutide at the beginning of its own escalation schedule, regardless of prior peptide experience. Your body needs to adapt to the glucagon receptor activation specifically, and no amount of GLP-1 tolerance from semaglutide or GLP-1/GIP tolerance from tirzepatide prepares you for that third receptor pathway.
Step-by-step guide to calculating your retatrutide dose
Let us walk through the complete calculation process from start to finish. No shortcuts. No assumptions. Every step laid out so you can follow along with whatever vial you have.
Step 1: identify your vial potency
Check the label on your retatrutide vial. It will state the total peptide content in milligrams. Common sizes are 5mg, 10mg, 20mg, and 30mg. Write this number down. This is your starting point and the single most important input for every calculation that follows.
If the label says "5mg lyophilized retatrutide," your vial contains 5 milligrams of peptide in powder form. Nothing else. The powder takes up negligible volume, so when you add bacteriostatic water, the total volume of your reconstituted solution equals the volume of water you added. This simplification makes the math clean and accurate.
Step 2: decide your reconstitution volume
Based on the reference tables above, choose how much bacteriostatic water to add. Your choice should balance two competing needs: measurable volumes for your smallest planned dose, and single-draw capability for your largest planned dose.
A practical rule of thumb: your largest planned weekly dose should require no more than 80 units (0.8mL) from the reconstituted solution. This keeps you within comfortable syringe range with room for small measurement variations.
For a 10mg vial where you plan to escalate to 8mg weekly, the math is: you need 8mg from a solution where drawing 80 units gets you that amount. 80 units = 0.8mL. So 8mg / 0.8mL = 10mg/mL required concentration. 10mg vial / 10mg per mL = 1mL of water needed. Add 1mL of bacteriostatic water.
Step 3: reconstitute the peptide
Using a sterile syringe, draw your calculated volume of bacteriostatic water. Insert the needle through the rubber stopper of the retatrutide vial and inject the water slowly along the inside wall. Do not blast it directly onto the powder. Gentle, controlled injection preserves peptide integrity.
Let the water run down the glass wall and contact the powder naturally. Then gently swirl the vial. Do not shake it. Vigorous shaking can damage the peptide through excessive agitation and foaming. Swirl until the powder dissolves completely and the solution is clear. This typically takes 30 seconds to 2 minutes. If the solution remains cloudy after 5 minutes of gentle swirling, something may be wrong with the peptide or the water, and you should not use it.
For a complete walkthrough of reconstitution technique, including what to do if problems arise, see our bacteriostatic water mixing guide. You can also review the free reconstitution calculator walkthrough. Proper technique is just as critical as accurate math. A perfectly calculated dose means nothing if the reconstitution process degraded the peptide.
Step 4: calculate your concentration
Divide the vial potency by the water volume you added.
Example: 10mg vial + 1mL water = 10mg/mL = 10,000mcg/mL
Write this concentration on the vial with a permanent marker along with the reconstitution date. You will reference this number every time you draw a dose. Some researchers also note the concentration in mcg per unit: at 10mg/mL, each unit on a U-100 syringe contains 100mcg (since 10,000mcg per 100 units = 100mcg per unit).
Step 5: determine units per dose
Divide your target dose by the concentration, then multiply by 100 to convert mL to units.
Formula: Units = (Target Dose in mg / Concentration in mg per mL) x 100
Or equivalently: Units = (Target Dose in mcg / mcg per unit)
Examples for a 10mg/mL solution:
For 1mg dose: (1 / 10) x 100 = 10 units
For 2mg dose: (2 / 10) x 100 = 20 units
For 4mg dose: (4 / 10) x 100 = 40 units
For 8mg dose: (8 / 10) x 100 = 80 units
For 12mg dose: (12 / 10) x 100 = 120 units (requires two draws from a 1mL syringe)
Step 6: calculate total doses per vial
Divide the total vial potency by your weekly dose to find how many weeks one vial covers.
Example: 10mg vial / 2mg per week = 5 weeks. 10mg vial / 4mg per week = 2.5 weeks. 10mg vial / 8mg per week = 1.25 weeks.
This calculation drives your vial purchasing decisions. Knowing you need approximately one 10mg vial every 1.25 weeks at the 8mg dose means you need roughly 3.5 vials for a four-week maintenance block. Planning ahead prevents gaps in your protocol, and the peptide cost calculator can help you estimate total research costs across the full escalation schedule.
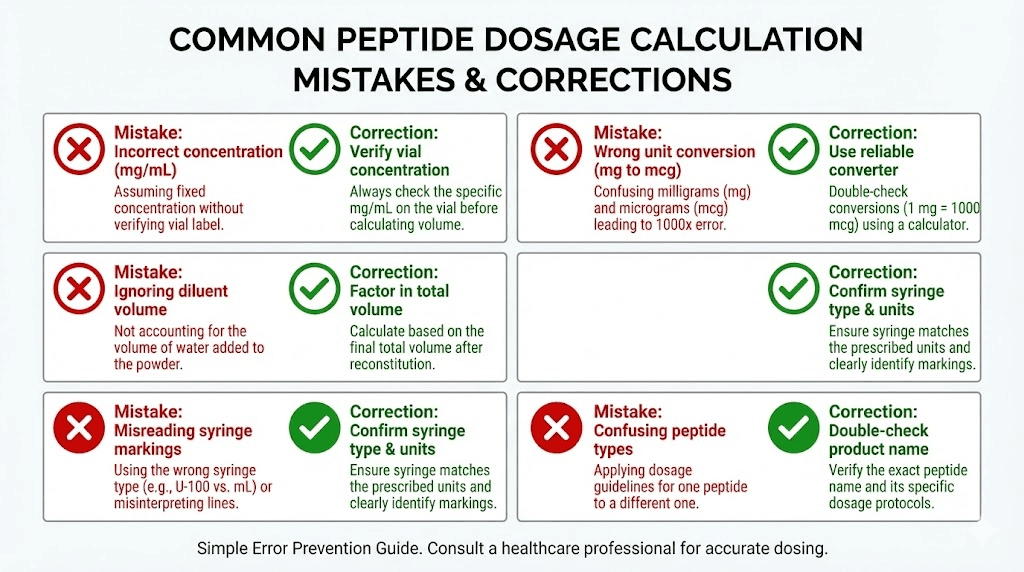
Common dosage calculation mistakes and how to avoid them
Even experienced researchers make these errors. Some of them are simple arithmetic mistakes. Others are conceptual misunderstandings that lead to weeks of incorrect dosing before anyone notices. Each one is preventable if you know what to watch for.
Mistake 1: confusing mg and mcg
This is the most dangerous calculation error. One milligram equals 1,000 micrograms. If a protocol calls for 2mg and you accidentally calculate for 2mcg, you are dosing at one thousandth of the intended amount. If you calculate for 2,000mg instead of 2,000mcg (which equals 2mg), you have a number one thousand times too high.
The fix: always convert your target dose to the same unit as your concentration before dividing. If your concentration is in mg/mL, keep your target dose in mg. If your concentration is in mcg/mL, convert your target dose to mcg first. Never mix units in the same equation.
Mistake 2: forgetting to adjust for dose escalation
You calculate 40 units for your 2mg dose, set a reminder, and draw 40 units every week for three months. Problem: you should have escalated to 4mg at week 5, 8mg at week 9, and potentially 12mg at week 13. By drawing the same 40 units throughout, you never exceeded the starting dose.
The fix: create a complete dosing schedule before you begin. Write down the exact units to draw for each week of the protocol. Put it on your refrigerator, in your phone calendar, or taped to your peptide storage container. Every time the dose changes, the units change, and you need a physical reminder to update your draw amount.
Mistake 3: using the wrong syringe
Insulin syringes come in multiple sizes: 0.3mL (30 units), 0.5mL (50 units), and 1.0mL (100 units). The unit markings mean different things at different scales. On a 0.3mL syringe, the lines are spaced further apart, giving you better precision for small doses but a maximum capacity of only 30 units. On a 1.0mL syringe, each line represents a larger volume increment, reducing precision but allowing draws up to 100 units.
The fix: match your syringe to your dose. For doses under 30 units (common during the 1-2mg starting phase), use a 0.3mL syringe for maximum precision. For doses between 30 and 50 units, a 0.5mL syringe works well. For doses above 50 units, use a 1.0mL syringe. This simple matching eliminates both measurement imprecision at low doses and capacity issues at high doses.
Mistake 4: not accounting for dead space
Every syringe has a small amount of dead space, the volume in the needle hub that does not get expelled when you push the plunger fully. On most insulin syringes, this is roughly 0.5 to 1 unit. Over a single dose, this is negligible. Over a full vial, however, the accumulated dead space means you get slightly fewer total doses than calculated.
For a 10mg vial expected to provide 5 doses at 2mg each, dead space losses of roughly 1 unit per draw mean you lose approximately 5 units total. At 5mg/mL concentration, that is 0.25mg of peptide, about 2.5% of the total vial. Not catastrophic, but worth knowing, especially if your last dose from a vial seems to come up short.
Mistake 5: reconstituting with the wrong water
Bacteriostatic water contains 0.9% benzyl alcohol as a preservative, which allows the reconstituted solution to remain stable and sterile for multiple uses over days or weeks. Sterile water for injection does NOT contain a preservative and should only be used for single-dose reconstitution, as it provides no protection against microbial contamination after the first needle puncture.
Using sterile water instead of bacteriostatic water means your reconstituted peptide must theoretically be used within 24 hours. Since most research protocols involve drawing from the same vial over multiple days or weeks, bacteriostatic water is the correct choice for retatrutide reconstitution. Our guide on water types for peptide reconstitution covers this distinction in detail.
Advanced dosing considerations for experienced researchers
Once you have mastered the basic calculations, several nuanced factors can further optimize your retatrutide research protocol. These are the details that separate adequate dosing from precision dosing, the kind of refinements that experienced researchers in the SeekPeptides community discuss regularly.
Body weight considerations
The Phase 2 clinical trial used fixed doses regardless of body weight. A 70kg participant and a 120kg participant both received the same milligram dose at each escalation step. This simplified the trial design but raises legitimate questions about whether weight-based dosing might improve outcomes.
While no official weight-based protocol exists for retatrutide, the pharmacological principle is straightforward: a larger body distributes the same dose across more tissue, resulting in lower effective tissue concentration. Some researchers adjust timing or escalation speed based on body weight. A 90kg researcher who tolerates 4mg easily might escalate to 8mg sooner than a 60kg researcher who experiences significant appetite suppression at 4mg. Neither approach is wrong, but both should be deliberate decisions based on observed response, not arbitrary changes.
The SeekPeptides peptide calculator provides weight-based reference ranges for various peptides, though for retatrutide specifically, the clinical protocol doses (2mg, 4mg, 8mg, 12mg) remain the standard reference points.
Injection site rotation
Retatrutide is administered subcutaneously, meaning into the fat layer just beneath the skin. The abdomen, upper thigh, and upper arm are the three primary injection sites. Rotating between sites serves two purposes: it prevents lipodystrophy (localized fat changes at repeated injection points) and potentially affects absorption rates.
Subcutaneous absorption varies by site. Abdominal injections typically provide the fastest and most consistent absorption. Thigh injections absorb slightly slower. Upper arm injections fall somewhere between the two. While these differences are generally small for weekly injections, maintaining consistent site selection within each escalation phase can reduce one variable that might otherwise confuse your assessment of dose response.
A practical rotation schedule: abdomen during weeks 1-4, upper thigh during weeks 5-8, upper arm during weeks 9-12, then back to abdomen for maintenance. This ensures that each dose level gets evaluated with a consistent absorption profile.
Timing your weekly injection
Retatrutide has a half-life that supports once-weekly dosing, similar to other long-acting peptides in the GLP-1 class. The key practical consideration is picking a consistent day and time that you can maintain throughout the protocol.
Many researchers prefer morning injections early in the week (Monday or Tuesday mornings) for two reasons. First, any transient gastrointestinal effects from the injection tend to be most noticeable in the first 24-48 hours, and experiencing them during the workweek means they typically resolve before the weekend. Second, the peak appetite suppression effect occurs roughly 1-3 days after injection, which aligns well with maintaining dietary discipline during the working days when routine meals are easier to plan.
What truly matters is consistency. Injecting every Tuesday at 8am creates a reliable 168-hour interval between doses. Shifting between Monday evening, Wednesday morning, and Friday afternoon creates intervals of 132, 156, and 180 hours, introducing unnecessary pharmacokinetic variability into your research data.
Handling dose escalation side effects
The transition periods, especially from 2mg to 4mg and from 4mg to 8mg, are where most side effects occur. Clinical trial data from the NEJM Phase 2 study showed that gastrointestinal events were predominantly mild to moderate, occurred primarily during dose escalation, and were partially mitigated by starting at 2mg rather than 4mg.
Practical management strategies that experienced researchers use:
Meal timing on escalation day: Eat a light, low-fat meal 2-3 hours before your injection. Having food in your stomach provides a buffer against nausea, while keeping the meal light prevents the excessive fullness sensation that higher doses can trigger.
Hydration protocol: Increase water intake to 2.5-3 liters on the day of injection and the following day. Sip consistently rather than drinking large amounts at once. This helps manage the most common side effects including nausea, constipation, and general GI discomfort. For more detail on managing these, our peptide safety guide covers side effect management comprehensively.
The "half-step" approach: Some researchers soften the 2mg to 4mg transition by doing one week at 3mg before moving to 4mg. This is not part of the official clinical protocol, but anecdotally reduces the severity of transitional GI symptoms. Using a calculator makes this easy: at 10mg/mL concentration, a 3mg dose is simply 30 units.
Planning your vial supply for a complete protocol
Running out of peptide mid-escalation is more than an inconvenience. It disrupts your protocol timing, potentially requiring you to restart the escalation process if the gap extends beyond a week. Proper supply planning starts with knowing exactly how many milligrams you need for each phase of the protocol.
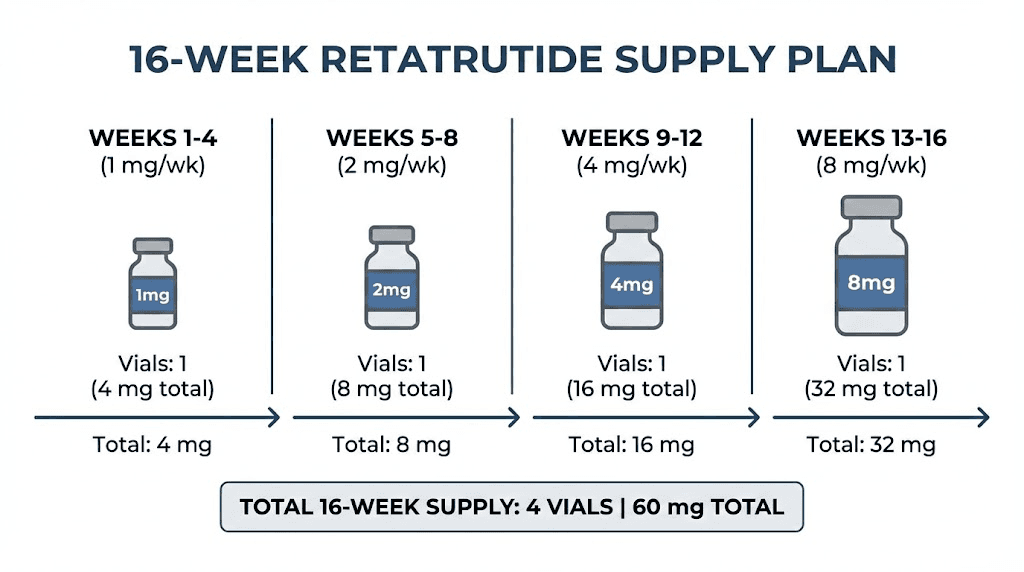
Complete supply calculation for a 16-week protocol
Weeks 1-4 (2mg/week): 2mg x 4 weeks = 8mg total
Weeks 5-8 (4mg/week): 4mg x 4 weeks = 16mg total
Weeks 9-12 (8mg/week): 8mg x 4 weeks = 32mg total
Weeks 13-16 (12mg/week): 12mg x 4 weeks = 48mg total
Grand total: 104mg over 16 weeks
Now translate that into vials:
Using 10mg vials exclusively: 104mg / 10mg = 10.4 vials. Round up to 11 vials. Plus one spare for reconstitution errors or contamination. Budget for 12 vials total.
Using a mix of 10mg and 20mg vials: One 10mg vial for weeks 1-4 (uses 8mg). Four 20mg vials for weeks 5-16 (uses 96mg). Total: 1 x 10mg + 4 x 20mg = 90mg. You still need one more 10mg vial plus some padding. Budget for 1 x 10mg + 5 x 20mg.
Using 30mg vials for the maintenance phase: One 10mg vial for weeks 1-4. One 20mg vial for weeks 5-8. Two 30mg vials for weeks 9-16 (uses 80mg of the 60mg available, meaning you would need additional supply). Three 30mg vials covers 90mg, sufficient for weeks 9-16 with some remaining.
The cost calculator on SeekPeptides can help you compare the total cost of different vial size strategies. Often, fewer larger vials cost less per milligram than many smaller ones, even if the per-vial price is higher.
Storage and stability during multi-week protocols
Reconstituted retatrutide should be stored at 2-8 degrees Celsius (36-46 degrees Fahrenheit), which means your standard refrigerator. Keep it away from the freezer compartment and the door shelves, which experience the most temperature fluctuation. The back of a middle shelf is typically the most temperature-stable location.
Reconstituted peptide stability varies, but the general consensus among peptide storage guides is that properly reconstituted retatrutide in bacteriostatic water maintains potency for 28-30 days when refrigerated. This means a vial reconstituted for the 2mg phase (which provides 5 weekly doses from a 10mg vial) should be used within about 5 weeks, which aligns perfectly with the 4-week dose escalation schedule plus a small buffer.
Unreconstituted (lyophilized/powder) retatrutide is considerably more stable. Stored in the freezer at -20 degrees Celsius, the powder form can maintain potency for months to years. If you purchase vials in bulk, keep unopened vials frozen and only reconstitute them when you are ready to begin that particular vial. For comprehensive storage recommendations across all forms, see our peptide shelf life guide.
Using the SeekPeptides calculator for retatrutide
While understanding the manual calculations is essential, using a dedicated peptide reconstitution calculator eliminates arithmetic errors and speeds up the process significantly. Here is how to use the SeekPeptides calculator specifically for retatrutide.
Step-by-step calculator walkthrough
Input 1: Syringe size. Select your insulin syringe volume. Most researchers use the 1mL (100 unit) option. If you are using a 0.5mL or 0.3mL syringe, select the corresponding option, as this changes how the calculator displays your draw volume.
Input 2: Vial amount. Enter the total milligrams of retatrutide in your vial. For a 10mg vial, enter 10. For a 20mg vial, enter 20. Double check this against your vial label. Entering the wrong vial potency cascades through every subsequent calculation.
Input 3: Water volume. Enter how many milliliters of bacteriostatic water you added (or plan to add). Use the reconstitution volume guidelines from the tables above. The calculator accepts values from 0.5mL to 5mL.
Input 4: Desired dose. Enter your target dose per injection in micrograms (mcg). Remember: 1mg = 1,000mcg. So for a 2mg dose, enter 2000. For a 4mg dose, enter 4000. For an 8mg dose, enter 8000. For 12mg, enter 12000.
The calculator then outputs:
Concentration: The resulting concentration of your reconstituted solution in mcg/mL and mg/mL.
Volume per dose: How many milliliters to draw for your target dose.
Units per dose: How many units to draw on your insulin syringe.
Total doses per vial: How many complete doses the vial provides at your specified dose level.
This entire process takes about 15 seconds. Compare that to the 5 minutes of manual calculation, and the risk of a misplaced decimal, and the calculator earns its place in every researcher toolkit.
Using the calculator across escalation phases
Here is a practical workflow: at the beginning of each 4-week escalation phase, open the calculator, enter your vial details and new dose, screenshot the results, and save it to your phone. Every injection day, reference the screenshot instead of recalculating. When the dose changes at the next escalation point, generate a new screenshot.
This approach combines the convenience of a calculator with the reliability of a fixed reference. You are not trusting yourself to enter the right numbers every single week, and you are not relying on memory for a number that might change. Simple, foolproof, effective.
Retatrutide pharmacology that affects dosing decisions
Understanding why the doses are what they are helps you make smarter decisions about your protocol. The three-receptor mechanism of retatrutide is not just a marketing claim. Each receptor contributes differently to the overall effect, and each activates at different dose thresholds.
GLP-1 receptor activation
The GLP-1 component of retatrutide reduces appetite through multiple mechanisms: slowing gastric emptying (food stays in your stomach longer, so you feel full sooner), signaling satiety centers in the brain (your brain gets a stronger "stop eating" signal), and enhancing insulin secretion in response to meals. This receptor is already meaningfully activated at the 2mg starting dose, which is why most researchers notice some appetite changes even during the first week.
At higher doses (8-12mg), GLP-1 activation approaches its ceiling effect. This means the appetite suppression does not continue to increase proportionally with dose beyond a certain point. The additional benefits of higher doses come primarily from the other two receptors, not from more GLP-1 activity.
GIP receptor activation
The glucose-dependent insulinotropic polypeptide (GIP) receptor adds a second dimension to the metabolic response. GIP improves insulin sensitivity and enhances beta cell function in the pancreas. It also appears to play a role in fat metabolism, though the exact mechanisms are still being elucidated in clinical research.
GIP receptor activation becomes more significant at the 4mg dose level and continues to increase through the dose range. This is one reason why the 4mg to 8mg transition often produces the most dramatic changes in body composition. The combination of strong GLP-1 appetite suppression with meaningful GIP-mediated metabolic improvement creates a synergistic effect that exceeds what either receptor could produce alone, a principle similar to why peptide stacking sometimes outperforms individual compounds.
Glucagon receptor activation
This is what makes retatrutide unique. The glucagon receptor component increases energy expenditure through thermogenesis, promotes hepatic fat oxidation (your liver burns more fat), and stimulates lipolysis (fat cells release their stored triglycerides for use as fuel). No other approved or late-stage weight loss peptide activates this pathway.
Glucagon receptor activation is minimal at 1-2mg but increases significantly at 4mg and becomes a major driver of the metabolic profile at 8mg and above. This explains the clinical observation that the weight loss acceleration from 4mg to 8mg is proportionally larger than from 2mg to 4mg. You are not just getting more of the same effect. You are unlocking an entirely new metabolic pathway.
The trade-off is that glucagon can raise blood glucose in some contexts, which is why the escalation schedule matters. Starting low lets the GLP-1 and GIP components establish glycemic control before the glucagon component challenges it. In the Phase 2 trial, this approach resulted in net improvements in glycated hemoglobin and fasting glucose across all dose groups, confirming that the three receptors balance each other when introduced gradually.
Troubleshooting your retatrutide dosage protocol
Sometimes things do not go as planned. Here are the most common problems researchers encounter and how to solve them using your calculator and protocol knowledge.
Problem: no noticeable effects after 4 weeks at 2mg
This is actually normal. The 2mg dose is a receptor adaptation phase, not a results phase. Some researchers, especially those with higher body weight or prior GLP-1 exposure, may not notice any appetite or metabolic changes at 2mg. The Phase 2 trial data confirms this: the 1mg dose group achieved only 8.7% weight loss at 48 weeks, indicating that low doses produce modest effects that accumulate slowly.
The solution is not to increase the dose prematurely. Stick with the 4-week timeline at 2mg, then escalate to 4mg as planned. Effects typically become noticeable within 1-2 weeks at the 4mg level. If you skip the 2mg phase entirely and start at 4mg (which some protocols allow), the gastrointestinal side effects are notably more severe, trading impatience now for discomfort later.
Problem: persistent nausea at a new dose level
Nausea during dose escalation typically resolves within 3-7 days as your body adapts. If nausea persists beyond 10 days at the same dose, you have options. First, verify your calculation. A dose that is even 20-30% higher than intended can push you past your tolerance threshold. Use the calculator to double-check your units.
If the calculation is correct, consider splitting the dose. Instead of one 8mg injection weekly, try two 4mg injections spaced 3-4 days apart (for example, Monday and Thursday). The total weekly dose remains 8mg, but the peak plasma concentration is lower, which reduces GI symptoms for many researchers. You will need to recalculate units for the split dose: at 10mg/mL concentration, each 4mg injection is 40 units.
Problem: the last dose from a vial seems weaker
Two possible causes. First, the mathematical dead space issue discussed earlier means you might be drawing slightly less than intended on the last pull. Second, if the vial has been reconstituted for more than 3-4 weeks, peptide degradation may have reduced the effective concentration slightly, even with proper refrigeration.
The practical solution: when you get to what you estimate is the last dose in a vial, reconstitute your next vial first and draw the new dose from the fresh vial. Use any remaining solution in the old vial for your next injection as a "top-up" if needed, though most researchers simply discard the last remnant rather than risk imprecise dosing.
Problem: you accidentally added the wrong amount of water
If you added too much water, your solution is more dilute than intended. The peptide itself is fine. You simply need to draw more units per dose to compensate. Recalculate using the actual water volume you added. If you intended to add 1mL but added 2mL, your concentration is half of what you planned, so double the units per draw.
If you added too little water, the solution is more concentrated. Again, the peptide is fine, but you now need fewer units per dose. You could also add more bacteriostatic water to bring the concentration to your intended level. Adding water after initial reconstitution is acceptable as long as you maintain sterile technique and account for the new total volume in your calculations.
Either way, run the numbers through the reconstitution calculator with the corrected water volume, and your new units per dose will be accurate.
Retatrutide research landscape and what it means for dosing
Retatrutide is currently in Phase 3 clinical trials under the Eli Lilly TRIUMPH program. The first successful Phase 3 result, from TRIUMPH-4, showed average weight loss of up to 71.2 pounds in adults with obesity and knee osteoarthritis. Seven additional Phase 3 readouts are expected through the remainder of the year, covering applications in type 2 diabetes, obstructive sleep apnea, chronic low back pain, cardiovascular outcomes, and metabolic liver disease.
If the remaining trials produce positive results, Eli Lilly is expected to submit a New Drug Application (NDA) to the FDA in late year. Under standard review timelines of 6-10 months, regulatory approval could come shortly after. Until then, retatrutide remains an investigational compound available only through research channels.
What this means for dosing calculations: the clinical trial protocols use fixed escalation schedules with specific dose targets (typically 8mg or 12mg maintenance). As Phase 3 data becomes available, these protocols may be refined based on larger population data. Researchers who understand the calculator fundamentals will be able to adapt to any protocol changes seamlessly, because the underlying math never changes. Only the target numbers change, and the dosage charts will be updated accordingly as new data emerges.
For researchers tracking the latest developments, SeekPeptides provides regular updates on clinical trial outcomes, protocol refinements, and community-sourced observations that complement the official clinical data.
Retatrutide dosage calculator for specific research goals
Different research objectives call for different approaches to the dose escalation schedule. While the fundamental calculation method remains identical, knowing which dose range aligns with your specific goals helps you plan vial purchases, set realistic timelines, and optimize your protocol from day one.
Weight management research protocol
The primary clinical application of retatrutide centers on weight management. The Phase 2 trial demonstrated that higher doses produce greater reductions in body weight, with the 12mg group achieving 24.2% average weight loss at 48 weeks. For researchers focused specifically on weight management outcomes, the full escalation to 12mg provides the most robust data, though the 8mg dose produced 22.8% weight loss, only 1.4 percentage points less.
The calculator implications are straightforward: plan your vial supply for 12mg maintenance if maximum weight reduction is the research objective, or for 8mg maintenance if tolerability is a higher priority. At 12mg weekly using 20mg vials reconstituted with 1mL (20mg/mL), each dose requires 60 units, and each vial provides approximately 1.7 weekly doses. For a 12-week maintenance phase, budget 7-8 vials of 20mg. For more context on fat loss peptide protocols, our comprehensive guides cover the full landscape of options.
Metabolic health research protocol
Beyond weight management, retatrutide showed remarkable improvements in metabolic markers. The Phase 2 trial reported that 72% of participants with prediabetes at baseline reverted to normoglycemia. Fasting glucose, insulin levels, glycated hemoglobin, and lipid profiles all improved significantly across dose groups.
For metabolic health research, the 4mg to 8mg dose range appears to offer the best balance of metabolic benefit and tolerability. The glucagon receptor activation at these doses enhances hepatic fat oxidation without the more pronounced GI effects of 12mg. Some researchers studying metabolic parameters specifically choose to maintain at 8mg rather than escalating further, allowing for longer protocol durations with the same vial supply.
Understanding the current state of peptide research helps contextualize these decisions within the broader scientific landscape. Retatrutide represents a significant advancement over single-target approaches to visceral fat reduction precisely because the triple-receptor mechanism addresses metabolic dysfunction from multiple angles simultaneously.
Body composition research protocol
Researchers interested in body composition changes, specifically the ratio of fat loss to lean mass preservation, face a nuanced dosing consideration. Higher doses produce more total weight loss, but the proportion of that weight loss coming from fat versus lean tissue varies with dose, activity level, and protein intake during the protocol.
The glucagon receptor activation at 8mg and above drives significant lipolysis and fat oxidation. Combined with adequate protein intake (widely recommended at 1.2-1.6g per kg of body weight during GLP-1 protocols) and resistance training, the higher dose ranges may actually preserve lean mass better than lower doses, because the energy deficit is being met predominantly through fat oxidation rather than muscle catabolism. This hypothesis is supported by emerging data but has not been definitively confirmed in large trials.
For body composition research, calculating your dose is identical, but the supporting protocol matters more. Track body weight alongside other composition metrics. Ensure your muscle-supporting protocols are in place before beginning escalation. And use the calculator to plan a complete protocol timeline that allows for meaningful data collection at each dose level.
Combining retatrutide with other research peptides
Some researchers explore whether retatrutide can be part of a broader peptide protocol. This adds another layer of complexity to dosage calculations, because timing, potential interactions, and total injection volume all need consideration.
Retatrutide and recovery peptides
The weight loss and metabolic effects of retatrutide do not overlap mechanistically with healing and recovery peptides like BPC-157 or TB-500. These peptides target completely different receptor systems, tissue repair and anti-inflammatory pathways versus metabolic hormone signaling. From a purely theoretical pharmacological standpoint, there is no known direct interaction between these compound classes.
However, practical considerations exist. The GI effects of retatrutide, particularly nausea and reduced appetite, can make it harder to maintain the caloric and protein intake needed to support tissue repair processes. Researchers combining retatrutide with recovery peptides should be especially attentive to nutritional adequacy and may benefit from stacking protocols that account for timing and injection scheduling.
From a calculation standpoint, retatrutide and BPC-157 (for example) are reconstituted and dosed independently. You need separate calculations for each: a BPC-157 dosage calculator for one and the retatrutide calculator for the other. Never mix different peptides in the same syringe or vial unless specifically directed by a protocol that has validated the combination stability.
Retatrutide and growth hormone peptides
Research on combining metabolic peptides with growth hormone secretagogues like ipamorelin or CJC-1295 is limited but growing. The theoretical rationale is that GH peptides could help preserve lean mass during the aggressive fat loss driven by retatrutide. Again, the dosing calculations are entirely separate for each compound, using the appropriate CJC-1295 calculator or ipamorelin calculator alongside the retatrutide calculator.
The critical point: adding more peptides to a protocol does not change how you calculate retatrutide doses. The formula is the same regardless of what else you are researching. But keeping a clear, organized dosing log becomes exponentially more important when managing multiple compounds. Our peptide cycle planning guide covers multi-compound protocol management in detail, and the peptide stack calculator helps organize complex multi-peptide protocols.
Retatrutide and other GLP-1 compounds
This one is simple. Do not combine retatrutide with semaglutide, tirzepatide, or any other GLP-1 receptor agonist. The receptor overlap creates compounding effects that dramatically increase side effect risk without proportional benefit. There is no scenario where stacking two GLP-1 agonists makes pharmacological sense, and no calculator can make an unsafe combination safe.
If you are transitioning from semaglutide to retatrutide, allow a washout period of at least 5-7 half-lives of the outgoing compound before beginning the retatrutide escalation. For semaglutide, with a half-life of approximately one week, this means a 5-7 week gap. For tirzepatide, with a similar half-life, the same guidance applies. Then begin retatrutide at the 2mg starting dose, not at a dose you estimate is "equivalent" to your previous protocol.
Record keeping and protocol documentation
A calculator gives you the right numbers. But numbers without records are numbers you will eventually forget, misremember, or confuse. Maintaining a simple log transforms a good protocol into a reproducible one.
What to track in your dosing log
For each injection, record:
Date and time: Establishes your weekly rhythm and reveals any unintentional irregularities in timing.
Dose (mg): Tracks your escalation progress and provides a reference if you need to recalculate mid-protocol.
Units drawn: Confirms that you translated the calculated dose correctly into syringe units.
Injection site: Tracks your rotation schedule and helps identify if absorption variations between sites affect your response.
Vial number and reconstitution date: Tells you how old the current reconstituted solution is, flagging when you are approaching the 28-30 day stability window.
Side effects (if any): Noting severity and duration of any GI symptoms helps you decide whether to adjust escalation timing, consider dose splitting, or consult additional resources.
Body weight (weekly): The primary outcome metric for most retatrutide research. Weekly measurement at the same time of day (morning, before food or water) provides the most consistent and comparable data points.
This log takes roughly 60 seconds per entry. Over a 16-week protocol, that is less than 20 minutes of total documentation time in exchange for a complete, analyzable record of your research. Members of the SeekPeptides community regularly share insights derived from this kind of careful documentation, contributing to the collective understanding of retatrutide protocols.
Digital versus physical logs
Either works. A spreadsheet offers easy calculation and graphing of weight trends. A simple notebook taped near your peptide storage location is harder to forget. Some researchers photograph their syringe before each injection to create a visual record of the volume drawn, which serves as a double check against their written log.
The format matters less than the consistency. Pick one method, use it every injection, and do not skip entries. Missing data points create gaps that undermine the value of the entire record.
Safety considerations specific to retatrutide dosing
Accurate dosing is a safety issue, not just an efficacy issue. Underdosing wastes time and resources. Overdosing causes unnecessary side effects and potential health risks. The margin between therapeutic and problematic doses in GLP-1 class peptides is relatively wide, but that does not excuse careless calculation.
Signs you may be overdosed
Persistent nausea lasting more than 7 days at the same dose, especially if accompanied by vomiting or inability to maintain hydration. Severe appetite suppression to the point of food aversion (not just reduced hunger). Rapid weight loss exceeding 3-4 pounds per week sustained over multiple weeks. Any of these warrant rechecking your calculation and potentially reducing the dose.
Recheck procedure: go back to step 1 of the calculation process. Verify the vial potency from the label. Verify the water volume from your reconstitution record. Recalculate the concentration. Recalculate the units per dose. Compare against what you have been drawing. A single misread number, like entering 1mL of water when you actually added 2mL, halves your concentration estimate and causes you to draw twice the intended dose.
Signs you may be underdosed
Zero appetite changes after 2 or more weeks at a dose that should produce noticeable effects (typically 4mg and above). Weight plateau during a phase that typically produces weight loss. No GI effects whatsoever, even mild ones, after escalation. While individual variation exists, complete absence of any effect at 4mg or higher suggests a calculation issue or a peptide potency problem.
Recheck procedure: same as overdose, start from step 1. Also verify that your peptide was stored correctly before and after reconstitution. Degraded peptide delivers reduced potency regardless of how accurately you calculated the dose. Review our peptide refrigeration guide and room temperature stability guide to assess whether storage conditions may have compromised your supply.
When to pause or discontinue a protocol
The calculator tells you what to draw. It does not tell you when to stop. These situations warrant pausing:
Severe, persistent vomiting that prevents adequate hydration for more than 48 hours. This is a medical situation, not a dosing optimization problem.
Any chest pain, heart palpitations, or cardiovascular symptoms. While retatrutide Phase 2 data showed improvements in cardiovascular risk markers, individual responses vary, and new cardiac symptoms during any peptide protocol should be evaluated immediately.
Weight loss exceeding 5% of body weight in a single week. Rapid weight loss at this rate suggests either dramatic overdosing, an concurrent illness affecting weight, or dehydration masquerading as fat loss. Pause, assess, recalculate, and resume only when the cause is identified. The comprehensive peptide safety resource covers these scenarios in further detail.
Interactions with other substances
Retatrutide affects gastric emptying, which means it can alter the absorption kinetics of other substances taken orally. Medications with narrow therapeutic windows (thyroid hormones, anticoagulants, certain antibiotics) may be absorbed differently when gastric emptying is slowed. This is a dosing consideration that the calculator cannot address, because it involves pharmacokinetic interactions beyond simple concentration math.
Alcohol tolerance often decreases on GLP-1 class compounds. The slowed gastric emptying means alcohol enters the bloodstream differently, and the appetite-suppressing effects can lead to drinking on an emptier stomach. Researchers should be aware of this practical consideration during their protocol, as it is one of the most commonly reported surprises in the common peptide mistakes literature.
Frequently asked questions
How much bacteriostatic water should I add to a 10mg vial of retatrutide?
For a 10mg vial, adding 1mL of bacteriostatic water creates a 10mg/mL concentration that works well across the full dose escalation range from 2mg (20 units) to 8mg (80 units). Adding 2mL creates a 5mg/mL concentration that gives better precision at lower doses but requires split draws at 8mg and above. Most researchers prefer the 1mL option for its versatility.
How many units do I draw for a 4mg dose of retatrutide?
The answer depends entirely on your reconstitution concentration. At 5mg/mL (10mg vial + 2mL water), a 4mg dose requires 80 units. At 10mg/mL (10mg vial + 1mL water), a 4mg dose requires 40 units. At 20mg/mL (20mg vial + 1mL water), a 4mg dose requires 20 units. Always use the peptide calculator to verify before drawing.
Can I use sterile water instead of bacteriostatic water for retatrutide?
You can, but you should not for multi-dose vials. Sterile water lacks the benzyl alcohol preservative found in bacteriostatic water, meaning it does not protect against microbial contamination after the first needle puncture. Since retatrutide protocols involve drawing from the same vial over multiple weeks, bacteriostatic water is the correct and safer choice.
What happens if I skip a week during dose escalation?
A single missed week is generally not critical, but you should not advance to the next dose level after a gap. If you missed week 3 of the 2mg phase, take the 2mg dose the following week and then complete the remaining planned 2mg weeks before escalating to 4mg. Gaps longer than two weeks may warrant restarting the current dose level for the full 4 weeks to maintain proper receptor adaptation.
How many total milligrams of retatrutide do I need for a full 16-week escalation?
A standard 16-week protocol following the 2mg, 4mg, 8mg, 12mg escalation requires approximately 104mg total. This accounts for 4 weeks at each dose level: (2x4) + (4x4) + (8x4) + (12x4) = 8 + 16 + 32 + 48 = 104mg. Plan for 10-15% extra to cover waste from dead space and potential reconstitution errors.
Is retatrutide dosing weight-based?
The clinical trial protocol uses fixed doses (2mg, 4mg, 8mg, 12mg) regardless of body weight. There is no officially validated weight-based dosing protocol for retatrutide. Some researchers adjust escalation timing based on body weight and individual response, but the target doses themselves remain the same across the research population.
How long does reconstituted retatrutide last in the fridge?
Reconstituted retatrutide in bacteriostatic water maintains potency for approximately 28-30 days when stored properly at 2-8 degrees Celsius. Unreconstituted powder stored frozen can last months to years. See our peptide storage guide for detailed stability information across different conditions.
Can I split my weekly retatrutide dose into two injections?
Yes, and some researchers prefer this approach, especially at higher doses (8mg and 12mg). Splitting a 12mg weekly dose into two 6mg injections (for example Monday and Thursday) reduces peak plasma concentration and can significantly reduce gastrointestinal side effects. Recalculate units for the split dose amount using the same concentration formula.
In case I do not see you, good afternoon, good evening, and good night. Join here.



