Jan 23, 2026
Your immune system is failing. Slowly. Imperceptibly. Every year after age 30, your thymus gland shrinks a little more. By 50, it has lost 80% of its functional tissue. By 70, it is nearly gone. This is not speculation or fear-mongering. It is basic immunology. And it explains why older adults get sicker more often, recover more slowly, and struggle to fight infections that younger people shake off in days.
The thymus is where T-cells mature. Without it, your adaptive immune system cannot produce the specialized defenders that identify and destroy pathogens. This process, called thymic involution, is one of the most predictable markers of biological aging. It happens to everyone.
But what if you could slow it down? What if you could restore thymic function even after decades of decline?
This is where thymalin enters the picture. Developed in Soviet Russia over 50 years ago, this bioregulator peptide has been studied for its ability to rejuvenate the aging thymus, restore T-cell populations, and potentially extend healthy lifespan. It is not a miracle cure. It is not FDA-approved in the West. But the research, spanning decades and thousands of patients, suggests something remarkable is happening at the cellular level.
This guide covers everything researchers need to know about thymalin. The science behind it. The dosing protocols. The clinical evidence. The practical considerations. Whether you are exploring longevity peptides for the first time or looking to add thymalin to an existing peptide stack, the information here will help you make informed decisions about this fascinating compound.
SeekPeptides has compiled this comprehensive resource from published research, clinical studies, and decades of real-world use in Eastern Europe.
The goal is not to sell you on thymalin, but to give you the complete picture so you can evaluate it yourself.
What is thymalin and where does it come from
Thymalin is a polypeptide complex extracted from the thymus glands of young calves. It contains short peptides, typically 2 to 8 amino acids in length, that mimic the signaling molecules naturally produced by a healthy thymus. These peptides regulate gene expression in immune cells, stimulate T-lymphocyte differentiation, and support the broader process of hematopoiesis, the creation of blood cells from stem cells.
The story begins in 1971 at the Military Medical Academy in Leningrad (now St. Petersburg). Vladimir Khavinson and his colleagues were searching for ways to restore immune function in soldiers exposed to radiation and extreme stress. They isolated peptide fractions from thymus tissue and discovered that these extracts could dramatically improve immune markers in compromised subjects.
By 1982, thymalin had received official approval for medical use in the Soviet Union. It became one of the first peptide bioregulators ever approved as a pharmaceutical drug. Over the following decades, Khavinson and his team at the Saint Petersburg Institute of Bioregulation and Gerontology continued refining the extraction process and studying the molecular mechanisms involved.
Today, thymalin remains approved and widely used in Russia, Ukraine, and several other Eastern European countries. It is prescribed for immune deficiency conditions, recovery from chemotherapy and radiation, chronic infections, and general immune support in aging populations. In the West, it is classified as a research peptide and is not approved for human therapeutic use by the FDA or EMA.
The active components of thymalin
Thymalin is not a single molecule. It is a complex mixture of short peptides that work together to modulate immune function. Using high-performance liquid chromatography (HPLC) and mass spectrometry, researchers have identified several key active components.
The dipeptide EW (glutamic acid-tryptophan) was isolated and later synthesized as a standalone drug called thymogen. Studies show thymogen is a potent immunomodulator on its own, suggesting this dipeptide carries significant biological activity.
The dipeptide KE (lysine-glutamic acid), also known as vilon, demonstrates the ability to regulate gene expression and stimulate stem cell differentiation into immune cell lineages.
The tripeptide EDP (glutamic acid-aspartic acid-proline), called crystagen, shows similar immunomodulatory effects and contributes to the overall activity of the thymalin complex.
These short peptides can cross cell membranes and enter the nucleus, where they bind to specific DNA sequences and histone proteins. This allows them to directly influence which genes are expressed, essentially reprogramming cellular behavior at the epigenetic level. Unlike hormones that work through surface receptors, these peptides operate inside the cell itself.
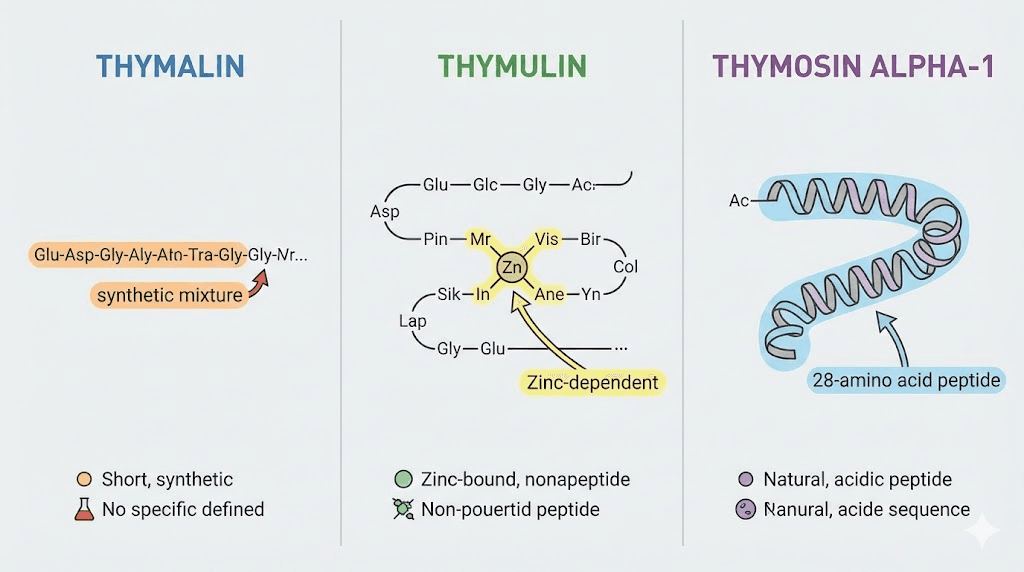
How thymalin differs from thymulin and thymosin alpha-1
The terminology around thymic peptides can be confusing. Thymalin, thymulin, and thymosin alpha-1 are three distinct substances, though they all relate to thymus function.
Thymulin is a nonapeptide (nine amino acids) that requires zinc as a cofactor to function. It is naturally produced by thymic epithelial cells and plays a role in T-cell differentiation. Synthetic thymulin is sometimes used in research settings.
Thymosin alpha-1 is a single peptide of 28 amino acids, originally isolated from bovine thymus but now produced synthetically. It has been studied extensively for chronic viral infections, cancer adjunct therapy, and immune modulation. Thymosin alpha-1 is approved as a pharmaceutical in over 35 countries under brand names like Zadaxin.
Thymalin is a mixture of multiple short peptides, not a single molecule. This gives it a broader range of activity, affecting multiple immune pathways simultaneously. Some researchers consider this an advantage because immune function involves complex, interconnected systems. Others prefer the more targeted approach of single-peptide therapies.
For those exploring immune-supporting peptides, understanding these distinctions helps inform protocol design. Thymalin offers comprehensive thymic restoration. Thymosin alpha-1 provides more specific cytokine modulation. They can be used together or separately depending on research goals.
The science of thymic involution and why it matters
The thymus sits behind your sternum, just above your heart. In childhood, it is a robust organ that trains T-cells to recognize threats and tolerate self. But something happens as you age. The functional tissue begins to atrophy. Fat cells replace active thymic epithelium. The hormone output drops. The ability to produce new, naive T-cells diminishes.
This process is called thymic involution, and it is one of the most reliable biomarkers of immunological aging.
By age 40, most people have lost 80% of their thymic function. By 65, the thymus produces fewer than 2% of the T-cells it generated during adolescence. This does not mean older adults have no T-cells. They retain memory T-cells from past infections. But their ability to mount effective responses to novel pathogens is severely compromised.
COVID-19 illustrated this dramatically. Older adults did not just get sicker because of underlying conditions. They struggled to generate effective T-cell responses to a virus they had never encountered before. Their depleted thymus could not produce enough naive T-cells to fight the infection effectively.
The consequences of reduced T-cell diversity
T-cells are not interchangeable.
Each one is programmed to recognize a specific antigen. Your body maintains a repertoire of millions of different T-cell variants, ready to respond to virtually any pathogen. But as thymic function declines, this diversity shrinks.
Memory T-cells accumulate from past infections. Naive T-cells, capable of recognizing new threats, become scarce. The immune system becomes reactive rather than adaptive. It can fight familiar enemies but struggles with novel ones.
This explains several hallmarks of age-related immune dysfunction. Increased susceptibility to new infections. Reduced vaccine efficacy. Higher rates of cancer, as immune surveillance of abnormal cells weakens. Chronic low-grade inflammation, sometimes called inflammaging, as the system becomes dysregulated.
Thymic involution is not the only cause of immunosenescence, but it is a major contributor. Restoring thymic function could theoretically address multiple downstream problems at once.
Can thymic function actually be restored
For decades, thymic involution was considered irreversible. The conventional wisdom held that once thymic tissue was replaced by fat, it was gone forever. Recent research challenges this assumption.
Studies in mice have shown that growth hormone, sex steroid ablation, and certain peptides can regenerate thymic tissue even in aged animals. New naive T-cells appear. Immune function improves. The thymus is not dead. It is dormant.
Human studies are more limited but equally intriguing. The TRIIM (Thymus Regeneration, Immunorestoration, and Insulin Mitigation) trial by Greg Fahy used a combination of growth hormone, DHEA, and metformin to regenerate human thymus tissue over one year. MRI scans confirmed that fatty tissue was replaced by functional thymic epithelium. Participants showed improved immune markers and, remarkably, epigenetic age reversal.
Thymalin operates through different mechanisms than the TRIIM protocol, but the underlying principle is the same. The thymus retains regenerative capacity throughout life. The right signals can reactivate it.
Thymalin peptide benefits supported by research
The research on thymalin spans over 50 years and includes animal studies, clinical trials, and long-term observational studies in human populations. While much of this work was conducted in Russia and may not meet Western standards for clinical evidence, the consistency of findings across multiple researchers and institutions is noteworthy.
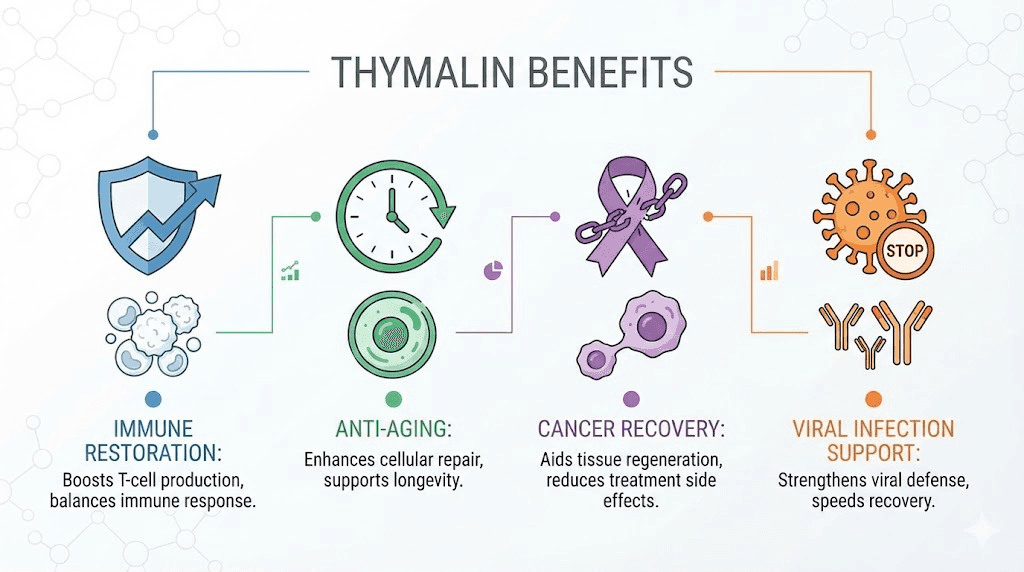
Immune system restoration and T-cell enhancement
The primary benefit of thymalin is immune restoration. Multiple studies show it increases circulating T-lymphocyte counts, improves the ratio of T-helper to T-suppressor cells, and restores immune parameters toward youthful ranges.
In a study of 266 elderly patients followed over 6-8 years, thymalin treatment normalized immune indices including T-cell subpopulations, immunoglobulin levels, and natural killer cell activity. Patients showed reduced incidence of acute respiratory infections, 2.0 to 2.4 times lower than untreated controls.
The mechanism involves stimulation of thymic epithelial cells to produce thymic hormones, promotion of stem cell differentiation into T-lymphocyte precursors, and regulation of cytokine networks that control immune cell behavior. Unlike immunosuppressants that dampen overactive immunity, thymalin appears to normalize immune function, potentially useful in both deficiency and excess states.
For researchers exploring peptides for specific conditions, the immunomodulatory rather than immunostimulatory nature of thymalin is an important distinction. It may help rebalance dysregulated immunity rather than simply boosting it.
Anti-aging and longevity effects
The most remarkable claims about thymalin relate to longevity. Khavinson and his colleagues conducted several long-term studies examining mortality rates in elderly patients treated with thymalin alone or in combination with epithalamin, a pineal peptide also known as epitalon.
In the largest study, 266 patients aged 60-90 were followed for 6-8 years. Those receiving annual thymalin injections showed a mortality rate 2.0-2.1 times lower than untreated controls. The combination of thymalin plus epithalamin was even more effective, with mortality rates 2.5 times lower. In patients who received both peptides annually for 6 consecutive years, mortality was 4.1 times lower than controls.
These are extraordinary claims. A 75% reduction in mortality over 6 years would rival or exceed the effects of any known intervention. The study has limitations: it was not blinded, randomization methods are unclear, and independent replication in Western settings has not occurred. But the magnitude of the effect, if even partially accurate, suggests thymalin deserves serious attention from longevity researchers.
Animal studies support the human findings. Mice given thymalin and epithalamin lived 20-40% longer than untreated controls. The combination appeared to delay multiple age-related diseases and maintain physiological function closer to youthful baselines.
Recovery from chemotherapy and radiation
Thymalin was originally developed to help soldiers recover from radiation exposure, and immune recovery remains one of its primary clinical applications in Russia. Chemotherapy and radiation therapy both devastate the immune system, leaving patients vulnerable to infections during treatment.
Clinical studies show thymalin accelerates immune recovery after cancer treatment. White blood cell counts normalize faster. T-cell populations recover more quickly. Patients experience fewer infectious complications during the vulnerable post-treatment period.
For those researching peptide therapy options, this application has practical significance. Many aging adults undergo cancer treatment at some point. Supporting immune recovery could reduce complications and improve outcomes.
Autoimmune condition support
Counterintuitively, thymalin may help with autoimmune conditions despite being an immune-supporting peptide. The key is its immunomodulatory rather than immunostimulatory action. In autoimmune disease, the immune system is not weak. It is dysregulated, attacking self-tissue while sometimes failing to control actual pathogens.
Studies in patients with rheumatoid arthritis, lupus, and multiple sclerosis have shown thymalin can help rebalance immune function. It appears to increase regulatory T-cells (Tregs) that suppress excessive immune activity while maintaining the ability to fight infections.
This dual action, supporting immunity where weak and calming it where overactive, is unusual among immune therapies. Most interventions either boost or suppress. Thymalin appears to normalize, pushing the system toward a healthy equilibrium.
COVID-19 and acute viral infections
During the COVID-19 pandemic, Russian researchers conducted a clinical trial of thymalin in severe cases. The results, published in Advances in Gerontology, showed that patients receiving thymalin in addition to standard care recovered faster than those on standard care alone.
Specifically, thymalin-treated patients showed more rapid clinical improvement, faster recovery from lymphopenia (low lymphocyte counts), quicker normalization of inflammatory markers like C-reactive protein and D-dimer, and improved natural killer cell counts.
The proposed mechanism relates to cytokine storm prevention. Severe COVID-19 often involves excessive inflammatory cytokine release that damages organs. Thymalin appears to modulate cytokine production, preventing the overreaction that causes much of the damage while supporting the T-cell response needed to clear the virus.
For researchers interested in anti-inflammatory peptides, the thymalin mechanism offers interesting parallels and potential synergies.
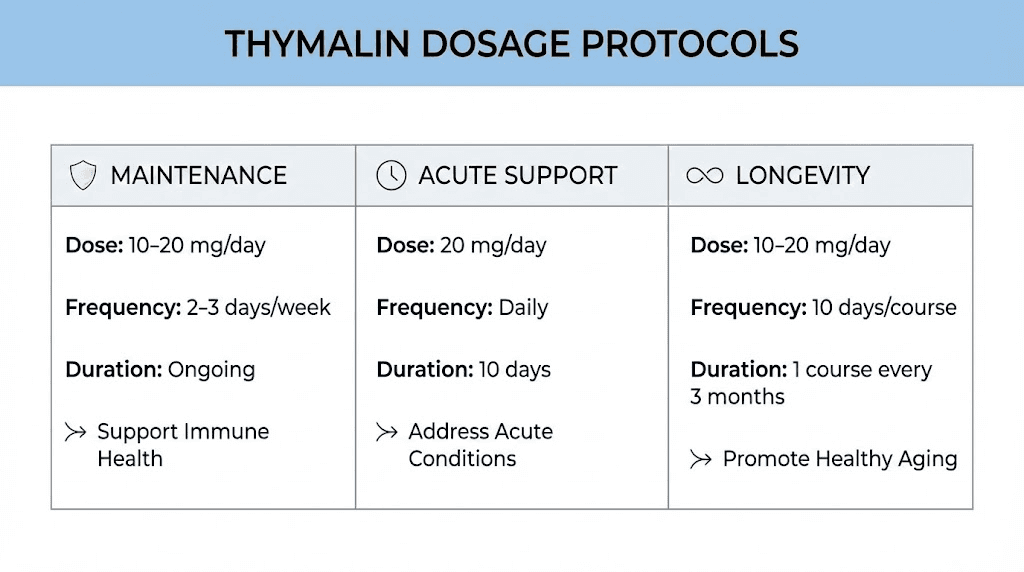
Thymalin dosage protocols for research
Thymalin dosing has been refined over 50 years of clinical use in Russia and Eastern Europe. The protocols below reflect published research and clinical practice, though individual responses vary and medical supervision is recommended for any peptide research.
Standard immune restoration protocol
The most common protocol uses 5-10 mg of thymalin injected intramuscularly or subcutaneously once daily for 10 consecutive days. This cycle is repeated 1-4 times per year depending on the condition being addressed and individual response.
For general immune maintenance in aging adults, a single 10-day cycle once or twice per year may be sufficient. For recovery from illness or cancer treatment, more frequent cycles every 3-6 months might be appropriate. Chronic conditions may warrant quarterly cycles until stability is achieved.
Longevity protocol (Khavinson regimen)
Based on the long-term studies showing mortality reduction, the longevity protocol involves annual or biannual 10-day cycles of thymalin, often combined with epithalamin (epitalon) for synergistic effects.
A typical approach would be thymalin 10 mg daily for 10 days, followed immediately or concurrently by epithalamin 10 mg daily for 10 days. This is repeated every 6-12 months. Some protocols alternate the peptides rather than using them together.
Acute immune support protocol
For acute infections or immune challenges, higher frequency dosing may be used. The Russian COVID-19 study used thymalin at 10 mg daily for 5-10 days during active infection. Similar protocols are used during recovery from surgery or other immune-stressful events.
Dosage considerations
The standard adult dosage range is 2-10 mg daily. Lower doses (2-5 mg) may be appropriate for smaller individuals, those new to peptides, or maintenance purposes. Higher doses (10 mg) are typically used for therapeutic applications and acute situations.
Cycle length of 5-10 days appears optimal based on research. Shorter cycles may not provide full benefit. Longer continuous use is not typically recommended, though the rationale for this is unclear from the literature.
Frequency of cycles ranges from once yearly for prevention to 4 times yearly for therapeutic applications. Using thymalin more often than every 3 months is rarely studied and may not provide additional benefit.
For those learning how to calculate peptide dosages, thymalin is relatively straightforward compared to weight-based peptides like BPC-157 or TB-500. The dose is typically fixed regardless of body weight.
Administration methods
Thymalin can be administered intramuscularly (IM) or subcutaneously (SubQ). Both routes are effective according to research. IM injection may provide slightly faster absorption, while SubQ is easier for self-administration and less uncomfortable.
The peptide comes as a lyophilized powder that must be reconstituted with bacteriostatic water before use. Standard reconstitution procedures apply: use appropriate water volume, inject slowly along the vial wall, allow powder to dissolve without shaking.
Timing does not appear critical. Morning administration is common simply for consistency, but no research suggests time of day affects efficacy. The peptide can be taken with or without food.
Reconstitution and storage guidelines
Proper handling of thymalin ensures maximum potency and safety. Like most research peptides, thymalin requires careful reconstitution and storage to maintain stability.
Reconstitution procedure
Thymalin typically comes in vials containing 10-20 mg of lyophilized powder. Reconstitution involves adding bacteriostatic water to create an injectable solution.
For a 10 mg vial, adding 1 ml of bacteriostatic water creates a concentration of 10 mg/ml. Each 0.1 ml (10 units on an insulin syringe) then contains 1 mg of thymalin. Adding 2 ml creates a 5 mg/ml solution, making it easier to measure smaller doses.
The reconstitution process is straightforward. Clean both vial tops with alcohol. Draw the appropriate amount of bacteriostatic water. Insert needle into the thymalin vial at an angle, with the needle tip pointing at the vial wall. Inject slowly, letting the water run down the side rather than blasting the powder directly. Let the vial sit for several minutes. Gently swirl (never shake) to ensure complete dissolution. The solution should be clear and colorless.
Storage requirements
Unreconstituted thymalin (lyophilized powder) is stable for 2 years when stored protected from light at room temperature or refrigerated. For longest shelf life, freezer storage is acceptable.
Reconstituted thymalin must be refrigerated at 2-8 degrees Celsius. At this temperature, it remains stable for approximately 4-6 weeks. Never freeze reconstituted peptide solution, as the freeze-thaw cycle can damage the peptides.
Keep away from light, as UV exposure degrades peptides. Store in the original vial or an amber glass container. Do not pre-load syringes for extended storage.
Signs of degradation
Fresh thymalin solution should be completely clear. Any cloudiness, particles, or color change indicates contamination or degradation. Discard compromised solution immediately.
Loss of potency may not be visible. If expected effects are not observed with a previously effective batch, peptide degradation is a possibility. Purchasing from reputable sources with proper third-party testing reduces this risk.
Thymalin side effects and safety profile
One of thymalin most notable characteristics is its excellent safety record. Over 50 years of clinical use in millions of patients has revealed remarkably few adverse effects.
Reported side effects
The most common side effects are injection-site reactions. Mild redness, swelling, or discomfort at the injection site occurs occasionally and typically resolves within hours. Proper injection technique minimizes this risk.
Some users report mild fatigue during the first few days of treatment.
This is attributed to immune recalibration as the system adjusts to increased thymic activity. The effect is typically transient and may actually indicate the peptide is working.
Rare side effects include headache, nausea, and restlessness (akathisia). These are infrequent and usually resolve with continued use or dose reduction. No serious adverse events have been reported in the published literature.
Long-term safety
The longevity studies following patients for 6-8 years provide valuable long-term safety data. No evidence of carcinogenicity, mutagenicity, or cumulative toxicity emerged. Thymalin-treated patients had lower mortality than controls, suggesting net benefit over extended use.
Unlike immunosuppressants that increase infection risk, or immunostimulants that can trigger autoimmune reactions, thymalin immunomodulatory action appears to normalize rather than push immune function toward extremes. This may explain its favorable safety profile.
Contraindications and precautions
Pregnancy and breastfeeding represent contraindications due to lack of safety data in these populations. The effects on fetal development are unknown.
Individuals with active autoimmune disease should use thymalin cautiously. While some studies suggest benefit, others recommend avoiding immune-modulating substances during autoimmune flares.
Organ transplant recipients on immunosuppressive therapy should avoid thymalin, as it could theoretically interfere with immunosuppression and trigger rejection.
Zinc deficiency substantially reduces thymalin effectiveness. Ensuring adequate zinc status before beginning treatment may improve response. General peptide safety considerations apply, including using sterile technique and sourcing from reputable suppliers.
Drug interactions
No significant drug interactions have been reported in the literature. Thymalin has been used alongside conventional medications including antibiotics, chemotherapy agents, and various cardiovascular drugs without apparent interaction.
Theoretical concerns exist about combining thymalin with other immunomodulators, as effects could potentially be additive or conflicting. In practice, combinations with other peptides like epithalamin and thymosin alpha-1 appear safe and may be synergistic.
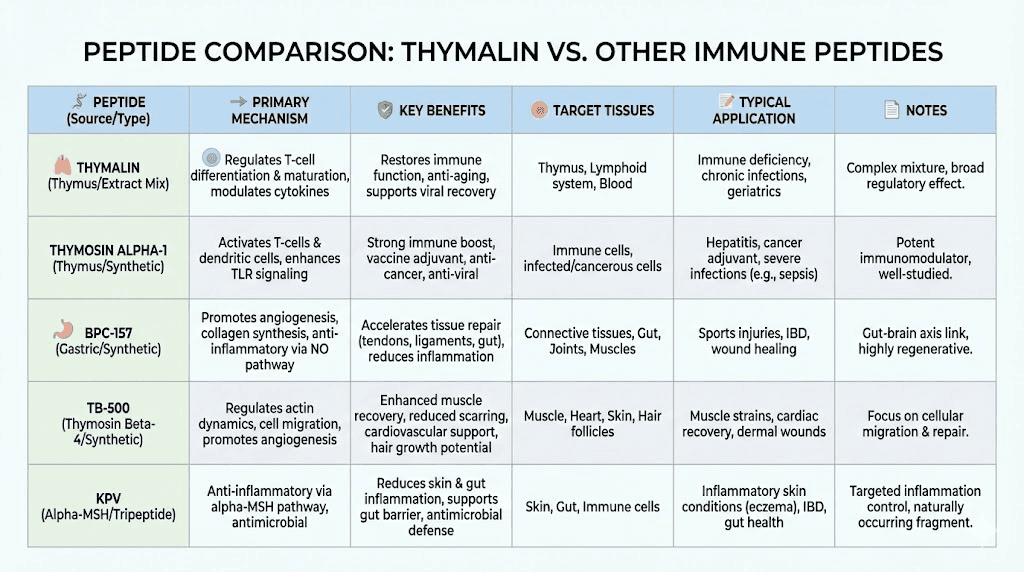
Thymalin compared to other immune peptides
Several peptides claim immune-modulating effects. Understanding how thymalin compares helps researchers select appropriate compounds for their goals.
Thymalin vs thymosin alpha-1
Both peptides originate from thymus research and support immune function, but they work differently.
Thymosin alpha-1 is a single 28-amino acid peptide that primarily stimulates cytokine production and enhances innate immune responses. It is particularly useful for viral infections and cancer adjunct therapy. The action is more targeted and acute.
Thymalin is a mixture of short peptides that restores thymic function more broadly. It supports T-cell production, balances immune subpopulations, and operates at the level of gene expression. The action is more foundational and regenerative.
For acute infection support, thymosin alpha-1 may be preferred. For long-term immune restoration and anti-aging, thymalin offers advantages. Some protocols use both, either concurrently or alternating.
Thymalin vs BPC-157
BPC-157 is a gastric peptide with remarkable healing properties but limited direct immune effects. It excels at tissue repair, including gut healing, tendon recovery, and wound healing. Any immune benefits are secondary to its regenerative action.
Thymalin directly targets the immune system without significant tissue healing properties. For immune restoration, thymalin is the clear choice. For injury recovery, BPC-157 is superior. The peptides address different needs and can be used together.
Thymalin vs TB-500
TB-500 (thymosin beta-4 fragment) shares a name with thymic peptides but functions quite differently. It promotes tissue repair, angiogenesis, and anti-inflammation. The immune effects are minimal compared to its regenerative properties.
Thymalin and TB-500 complement each other well.
Thymalin rebuilds immune capacity while TB-500 supports physical tissue recovery. Combining them could address both immunological and structural aspects of aging or illness.
Thymalin vs KPV
KPV is an anti-inflammatory peptide derived from alpha-melanocyte-stimulating hormone. It suppresses inflammatory cytokines and may benefit autoimmune and inflammatory conditions. The action is primarily anti-inflammatory rather than immune-restorative.
Thymalin modulates immunity more broadly, potentially helping with both excess inflammation and immune deficiency. KPV is specifically anti-inflammatory. For pure inflammation control, KPV may be more targeted. For comprehensive immune support, thymalin offers broader effects.
Stacking thymalin with other peptides
Peptide stacking involves using multiple compounds simultaneously or sequentially to achieve synergistic effects. Thymalin combines well with several other peptides, particularly for longevity and comprehensive health optimization.
Thymalin and epithalamin (epitalon) stack
This is the most studied peptide combination for longevity. Epithalamin is a pineal peptide that regulates melatonin production, circadian rhythms, and potentially telomere maintenance through telomerase activation.
Khavinson long-term studies found the combination more effective than either peptide alone. Mortality reduction was 2.5-fold with the combination versus 2.0-fold with thymalin alone. The proposed mechanism involves thymalin restoring immune function while epithalamin addresses neuroendocrine aging and oxidative stress.
A typical protocol uses thymalin 10 mg daily for 10 days, followed by epithalamin 10 mg daily for 10 days, repeated annually or biannually. Some researchers use both simultaneously for 10 days. Both approaches appear effective based on published research.
Thymalin and GHK-Cu stack
GHK-Cu is a copper peptide with regenerative, anti-inflammatory, and gene-modulating properties. It resets numerous genes toward youthful expression patterns and supports tissue repair throughout the body.
Combining thymalin and GHK-Cu addresses aging through two complementary mechanisms: immune restoration (thymalin) and tissue regeneration (GHK-Cu). The combination may provide comprehensive anti-aging effects spanning multiple organ systems.
Protocol options include concurrent use during the thymalin cycle, or alternating months of each peptide throughout the year. GHK-Cu dosing typically runs 1-2 mg daily, administered subcutaneously.
Thymalin and BPC-157/TB-500 healing stack
For recovering from illness, surgery, or injury, combining thymalin with healing peptides addresses both immune recovery and tissue repair.
Thymalin restores the immune system depleted by illness or medical treatment. BPC-157 and TB-500 accelerate healing of damaged tissues. Together, they support comprehensive recovery that neither alone could achieve.
This stack is particularly relevant after cancer treatment, major surgery, or severe infection. The immune system needs rebuilding while physical tissues need repair. Addressing both simultaneously may speed overall recovery.
Longevity super stack
Advanced longevity protocols sometimes combine multiple bioregulator peptides for maximal effect. A comprehensive stack might include thymalin (immune restoration), epithalamin (pineal and circadian), GHK-Cu (tissue regeneration), and possibly organ-specific peptides like vesugen (vascular) or cardiogen (cardiac).
Such combinations are speculative and lack controlled studies. However, the individual peptides have favorable safety profiles, and the mechanisms appear complementary rather than conflicting. Researchers pursuing aggressive longevity protocols may find this approach interesting.
SeekPeptides members have access to detailed stacking guides and protocols for optimizing peptide combinations based on individual goals and health status.
Clinical evidence and research studies
The evidence base for thymalin is unusual by Western standards. Most research was conducted in Russia and published in Russian-language journals. Translation and methodological differences make direct comparison to Western clinical trials difficult. Nevertheless, the volume and consistency of findings is notable.
The Khavinson longevity studies
The landmark study followed 266 elderly patients (aged 60-90) for 6-8 years at institutions in St. Petersburg and Kiev. Patients were divided into groups receiving thymalin alone, epithalamin alone, the combination, or no treatment (control).
Results showed consistent benefits across multiple health measures. Cardiovascular function improved. Immune parameters normalized. Bone density stabilized. Cognitive function was preserved. Mortality rates were significantly lower in all treatment groups compared to controls.
The 4.1-fold mortality reduction in the long-term combination group (thymalin plus epithalamin for 6 consecutive years) is extraordinary if accurate. Such an effect would represent the largest longevity intervention ever documented in humans.
Critics note methodological concerns: lack of blinding, unclear randomization, potential selection bias, and absence of independent replication. Supporters counter that the effect size is so large that methodological imperfections could not fully account for it. The debate continues.
COVID-19 clinical trial
A more recent prospective, randomized single-blind controlled trial examined thymalin in severe COVID-19 at the Chita State Medical Academy Hospital. Eighty patients were randomized to standard care (44 patients) or standard care plus thymalin (36 patients).
The thymalin group showed statistically significant improvements in clinical recovery speed, lymphocyte count normalization, C-reactive protein reduction, D-dimer normalization, and natural killer cell recovery. No adverse events were attributed to thymalin.
This study represents better methodology than older Soviet-era research. The results support thymalin efficacy for acute immune support, though larger trials would be needed for definitive conclusions.
Chemotherapy recovery studies
Multiple Russian studies have examined thymalin for immune recovery after cancer treatment. The consistent finding is accelerated normalization of white blood cell counts and lymphocyte subpopulations compared to untreated controls.
Clinical outcomes include fewer infectious complications during chemotherapy, shorter hospitalizations, and better quality of life scores. Some oncologists in Russia routinely prescribe thymalin as supportive care during cancer treatment.
Autoimmune disease research
Studies in rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis show thymalin can help rebalance immune function. The effect appears to involve increasing regulatory T-cells that suppress autoimmune activity while maintaining pathogen defense.
This immunomodulatory action, rather than simple immunostimulation, makes thymalin interesting for conditions where the immune system attacks self-tissue. However, more research is needed to define optimal protocols for specific autoimmune conditions.
Practical considerations for thymalin research
Moving from theory to practice involves several practical decisions. Where to source thymalin. How to verify quality. How to integrate it into a broader health optimization protocol.
Sourcing quality thymalin
Thymalin is available from research peptide suppliers in various countries. Quality varies significantly. The best suppliers provide third-party testing certificates showing peptide purity and identity verification.
Look for HPLC (high-performance liquid chromatography) testing showing purity above 98%. Mass spectrometry confirming peptide identity. Testing for contaminants including endotoxins and heavy metals. Clear labeling with batch numbers and expiration dates.
The best peptide vendors maintain consistent quality and provide documentation. Cheaper sources may offer degraded or mislabeled products that waste money and potentially pose safety risks.
Testing and verification
Beyond supplier certificates, researchers can verify peptide quality through independent testing. Peptide testing labs offer analysis services that confirm what you actually received matches what was ordered.
For thymalin specifically, HPLC with mass spec identification can verify the peptide mixture is genuine. While individual users may not require this level of verification, serious researchers should consider independent testing at least periodically.
Integrating thymalin into health protocols
Thymalin is not a standalone solution. It works best as part of a comprehensive health optimization approach that includes foundational elements like sleep, nutrition, exercise, and stress management. These basics support the immune system that thymalin helps restore.
Complementary interventions that may enhance thymalin effects include zinc supplementation (thymalin requires zinc for optimal function), vitamin D optimization (critical for immune function), regular exercise (supports immune health), adequate sleep (immune system repairs during sleep), and stress management (chronic stress suppresses immunity).
Sequential or concurrent use with other peptides as discussed in the stacking section can address multiple aspects of aging or health optimization simultaneously.
Monitoring response
Tracking response to thymalin helps optimize protocols. Baseline and follow-up blood work can measure complete blood count with differential, showing lymphocyte counts. Lymphocyte subset analysis (CD4, CD8 counts and ratios) provides more detail. Immunoglobulin levels (IgG, IgA, IgM) indicate humoral immunity. Natural killer cell counts and activity measure innate immune surveillance.
Subjective measures like frequency of infections, energy levels, and recovery from illness also indicate immune function changes. Keeping records allows protocol refinement over time.
Cost considerations
Thymalin is moderately priced compared to other research peptides. A 10 mg vial typically costs $30-60 depending on supplier and quantity purchased.
A standard 10-day cycle requires one to two vials, making annual costs relatively modest.
Compared to many peptide therapy costs, thymalin is economical. The short cycle duration (10 days versus continuous daily dosing for many peptides) keeps total consumption low. For longevity applications requiring only annual cycles, the investment is minimal relative to potential benefits.
Who might benefit from thymalin research
Thymalin is not for everyone. Understanding who might benefit helps target research appropriately.
Aging individuals (over 40)
Anyone experiencing age-related immune decline is a potential candidate. This includes most adults over 40, when thymic involution is well underway. Increased frequency of infections, slower recovery from illness, and reduced vaccine response all suggest compromised immune function that thymalin might address.
The longevity studies specifically enrolled elderly patients (60-90 years), and this population showed the most dramatic benefits. For those interested in peptides for aging, thymalin deserves consideration.
Post-cancer treatment recovery
Chemotherapy and radiation devastate the immune system. Thymalin clinical use in Russia centers on accelerating immune recovery in cancer patients. Anyone undergoing or recently completing cancer treatment might benefit from thymalin support.
Obviously, this should be coordinated with oncologists and not undertaken independently. But the evidence suggests thymalin can safely complement conventional cancer care and may improve outcomes during the vulnerable recovery period.
Chronic infection sufferers
Recurrent infections suggest immune deficiency. Chronic viral infections like hepatitis or herpes also indicate the immune system is not adequately controlling pathogens. Thymalin restoration of T-cell function could help break the cycle of recurrent illness.
Autoimmune condition management
Though counterintuitive, some autoimmune patients may benefit from thymalin immunomodulatory effects. By increasing regulatory T-cells and normalizing immune function, thymalin might help rebalance overactive immunity.
This application requires caution and monitoring. Not all autoimmune conditions respond the same way. Working with knowledgeable practitioners is essential for safe application in this population.
Longevity-focused researchers
Anyone pursuing aggressive longevity interventions should consider thymalin based on the Khavinson studies. Even if the mortality reduction claims are exaggerated by methodological issues, even a fraction of the reported benefit would be significant.
The combination with epithalamin appears particularly promising based on the research. For those already exploring longevity peptides, thymalin fills a unique niche addressing immune aging specifically.
Who should not use thymalin
Pregnant or breastfeeding individuals should avoid thymalin due to lack of safety data. Organ transplant recipients on immunosuppression should not use immune-modulating peptides. Those with active lymphoma or leukemia should avoid any immune stimulation without oncologist guidance. Individuals with hypersensitivity to bovine-derived products (thymalin originates from calf thymus) should use caution.
Frequently asked questions
How long does it take for thymalin to work?
Immune markers can begin improving within the first week of a 10-day cycle. Subjective benefits like reduced infection frequency or faster illness recovery may take longer to notice, often becoming apparent over subsequent months. The longevity benefits observed in studies accumulated over years of use, suggesting cumulative effects from repeated annual cycles.
Can thymalin be taken orally instead of injected?
Thymalin is traditionally administered by injection (intramuscular or subcutaneous). Like most peptides, oral administration would likely result in digestion before absorption. Some oral peptide formulations exist, but their bioavailability is generally much lower than injected forms. For optimal results, injection remains the standard administration route.
Is thymalin legal to purchase and use?
In the United States and most Western countries, thymalin is legal to purchase for research purposes. It is not FDA-approved for human therapeutic use, meaning it cannot be prescribed by physicians or sold for medical treatment. The legal status varies by country, and researchers should verify local regulations. Peptide legality depends on jurisdiction and intended use.
Does thymalin need to be cycled or can it be used continuously?
Thymalin is traditionally used in cycles rather than continuously. A typical protocol involves 10 consecutive days of daily injections, repeated 1-4 times per year. Continuous daily use is not studied and not recommended based on current evidence. The cyclical approach may prevent downregulation or tolerance that could occur with constant exposure.
Can thymalin be combined with thymosin alpha-1?
Yes, thymalin and thymosin alpha-1 can be used together or sequentially. Some protocols alternate between them or use thymosin alpha-1 for acute immune challenges and thymalin for baseline restoration. The mechanisms are complementary rather than redundant, potentially providing broader immune support than either alone.
What is the difference between thymalin and thymogen?
Thymogen is a synthetic dipeptide (glutamic acid-tryptophan) isolated from thymalin and produced as a standalone drug. It represents one active component of the thymalin complex. Thymalin contains thymogen plus additional active peptides (KE, EDP, and others). Thymogen may be sufficient for some applications, while thymalin provides a broader spectrum of activity.
Are there any dietary requirements while using thymalin?
Zinc is particularly important for thymalin function. Ensuring adequate zinc intake through diet or supplementation may enhance response. General nutritional adequacy supports immune function. No specific foods need to be avoided, though some researchers maintain general anti-inflammatory dietary practices during peptide protocols.
How should thymalin be stored during travel?
Reconstituted thymalin must remain refrigerated and has limited stability, making travel challenging. Options include using only unreconstituted (powder) form during travel and reconstituting at your destination, using insulated bags with ice packs for short trips (under 24 hours), or planning cycles around periods without travel. Peptide stability at room temperature is limited, making proper cold chain maintenance essential.
For researchers committed to optimizing their immune health and longevity protocols, SeekPeptides provides the most comprehensive peptide education available. Members access detailed protocol guides, stacking recommendations, and a community of experienced researchers who have navigated these questions firsthand.
In case I do not see you, good afternoon, good evening, and good night. May your thymus stay active, your T-cells stay abundant, and your immune system stay vigilant.



